Oral herpes is an infection caused by the herpes simplex virus.
What is the Pathology of Oral Herpes?
The pathology of oral herpes is:
-Etiology: The cause of oral herpes is caused by the herpes simplex virus type 1 (HSV-1).
-Pathogenesis: The sequence of events that lead to oral herpes the virus is spread by contact, the usual site for the implantation is skin or mucous membrane.
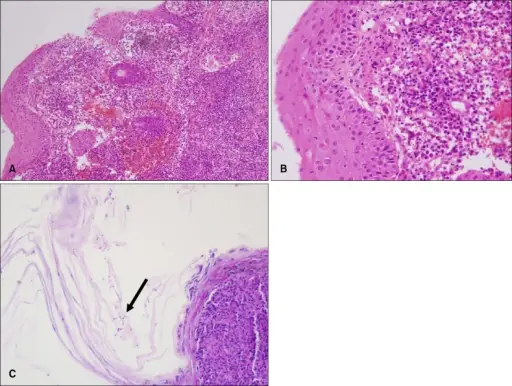
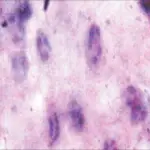
-Histology: The histology associated with oral herpes shows a low power pattern of a typical lesion is of an intraepidermal blister the key feature is acantholysis with solitary keratinocytes within the blister cavity.
How does Oral Herpes Present?
Patients with oral herpes typically affect males and females both present at the range of 25 and above. The symptoms, features, and clinical findings associated with oral herpes include open sores or rashes with a burning sensation.
How is Oral Herpes Diagnosed?
Oral herpes is diagnosed with a virus culture called PCR, blood test, or biopsy. PCR is the preferred test for diagnosing herpes infections.
How is Oral Herpes Treated?
Oral Herpes is treated by keeping the infected area clean and dry. Taking antiviral oral medications, such as acyclovir, famciclovir, and valacyclovir.
What is the Prognosis of Oral Herpes?
The prognosis of oral herpes is good. The sores and symptoms of oral herpes usually completely disappear in two to three weeks with no scarring. However, the sores may reappear under certain stressful situations.