Passive congestion of the liver is the acute liver injury due to a sudden, profound reduction in systemic blood flow.
What is the Pathology of Passive Congestion of the Liver?
The pathology of passive congestion of the liver is:
-Etiology: The cause of passive congestion of the liver includes congestive heart failure, restrictive cardiomyopathy, constrictive pericarditis, a right sided valvular disease involving the tricuspid or pulmonary valves, severe hypovolemia, septic shock, massive pulmonary embolism, hyperpyrexia, or heat stroke
-Genes involved: None.
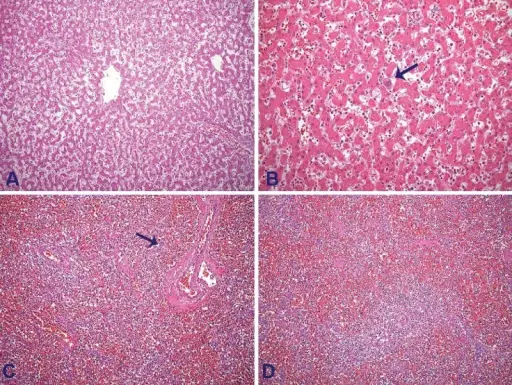
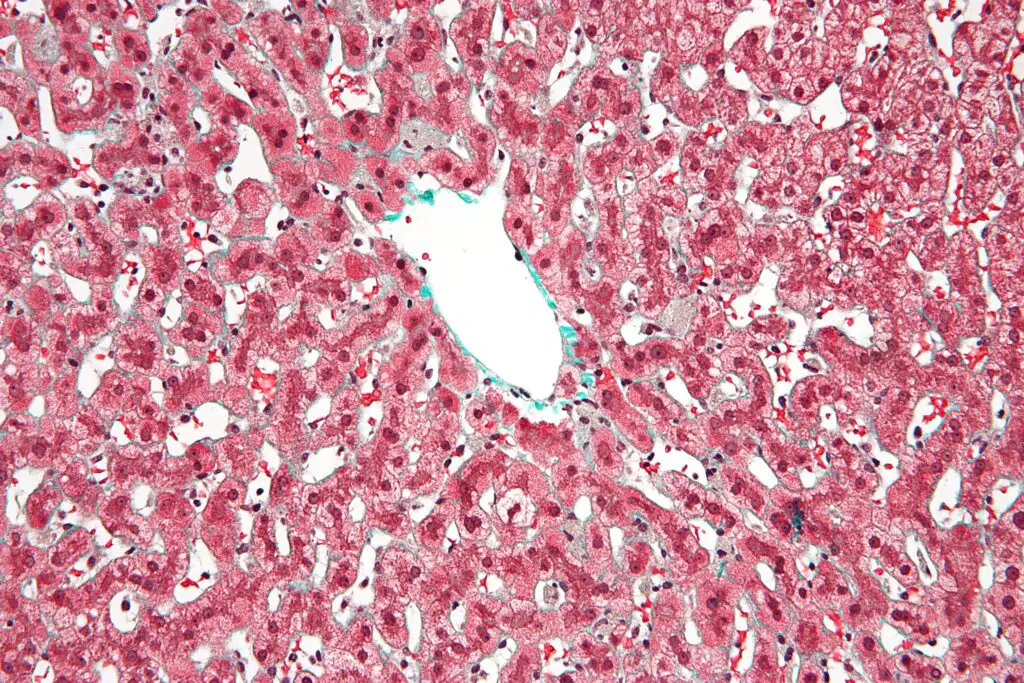
-Pathogenesis: The sequence of events that lead to passive congestion of the liver includes stasis of blood in the hepatic parenchyma, due to impaired hepatic venous drainage, which leads to the dilation of central hepatic veins and hepatomegaly. Elevated hepatic venous pressure, and decrease in hepatic venous flow causes hypoxic injury to hepatocytes and eventual diffuse hepatocyte death and fibrosis.
-Histology: The histology associated with passive congestion of the liver shows centrilobular ischemic necrosis and hepatic infarction.
How does Passive Congestion of the Liver Present?
Patients with passive congestion of the liver are typically males 50-years-old or older. The symptoms, features, and clinical findings associated with passive congestion of the liver include mild right upper quadrant abdominal pain, and right-sided heart failure.
How is Passive Congestion of the Liver Diagnosed?
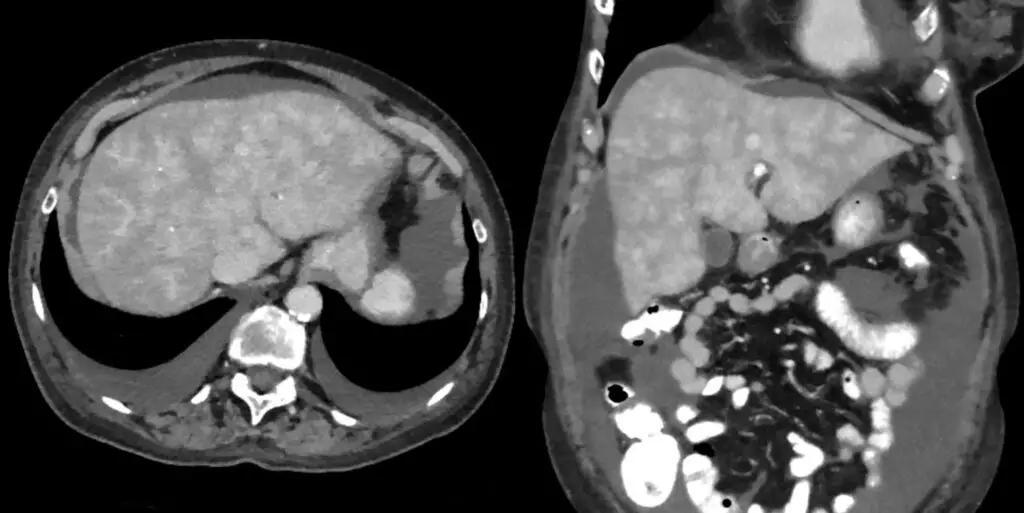
Passive congestion of the liver is diagnosed using a CT scan, MRI, ultrasound, and biopsy.
How is Passive Congestion of the Liver Treated?
Passive congestion of the liver is treated with surgical excision.
What is the Prognosis of Passive Congestion of the Liver?
The prognosis of passive congestion of the liver is poor with a higher mortality rate.