Peripheral giant cell granuloma is an oral pathologic condition that appears in the mouth as an overgrowth of tissue due to irritation or trauma.
What is the Pathology of Peripheral Giant Cell Granuloma?
The pathology of peripheral giant cell granuloma is:
-Etiology: The cause of peripheral giant cell granuloma is unknown, although local irritation due to dental plaque or calculus, periodontal disease, poor dental restorations, ill-fitting dental appliances, or dental extractions has been suggested to contribute to the development of the lesion.
-Pathogenesis: The sequence of events that lead to peripheral giant cell granuloma presumably arises from the periodontal ligament and thus occurs exclusively on the gingiva, usually between the permanent molars and incisors. The mandible and maxilla are involved at an almost equal frequency. PGCG classically presents as a solitary broad-based reddish-blue polypoid nodule
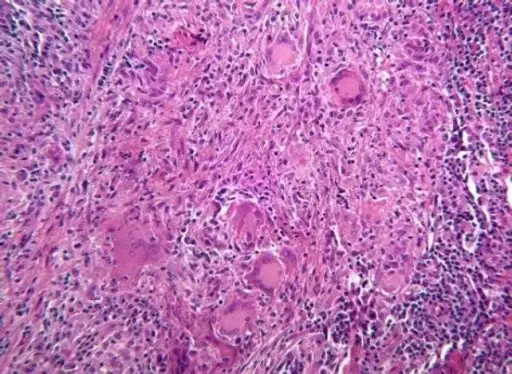
-Histology: The histology associated with peripheral giant cell granuloma shows fibrillar and reticular connective tissue stroma with abundant young connective tissue cells of fusiform shape, and multinucleated giant cells.
How does Peripheral Giant Cell Granuloma Present?
Patients with peripheral giant cell granuloma typically affect females present at the age range of 40-60 years. The symptoms, features, and clinical findings associated with peripheral giant cell granuloma include reddish-blue rubbery nodules that range in size from a few millimeters to 2cm. Surface ulceration is common
How is Peripheral Giant Cell Granuloma Diagnosed?
Peripheral giant cell granuloma is diagnosed by blood tests, chest X-rays, CT or MRI, and biopsy.
How is Peripheral Giant Cell Granuloma Treated?
Peripheral giant cell granuloma is treated by local surgical excision down to the bone.
What is the Prognosis of Peripheral Giant Cell Granuloma?
The prognosis of peripheral giant cell Granuloma is fair.