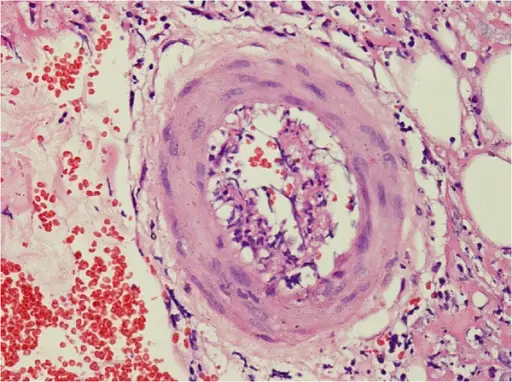
Polyarteritis nodosa is a systemic vasculitis associated with necrotizing inflammatory lesions that affects medium and small muscular arteries at bifurcations.
What is the Pathology of Polyarteritis Nodosa?
The pathology of polyarteritis nodosa is:
-Etiology: The cause of polyarteritis nodosa is unknown but is strongly linked with hepatitis B virus.
-Pathogenesis: The sequence of events that lead to polyarteritis nodosa start with immune complex mediated inflammation that may be due to hepatitis B virus infection leading to destruction of internal and external elastic lamina that results to fibrinoid necrosis.
-Morphologic changes: The morphologic changes involved with polyarteritis nodosa is segmental transmural necrotising inflammation
How does Polyarteritis Nodosa Present?
Patients with polyarteritis nodosa are typically men with no racial predilection and present at age range 45-65 years old. The symptoms, features, and clinical findings associated with polyarteritis nodosa include constitutional symptoms such as fever, malaise, fatigue, anorexia and weight loss, myalgia and arthralgia. Transient monocular blindness is the most common CNS presentation, while encephalopathy and seizures may occur due to multiple organ failure. Skin rashs, purpura, gangrene, nodules, and Raynaud phenomenon may also be present.
How is Polyarteritis Nodosa Diagnosed?
Polyarteritis nodosa is diagnosed with physical exam and laboratory tests. Althou non-specific, lab tests can help determine systemic nature of disease such as elevated ESR, leukocytosis, hepatitis B antigen, elevated creatinine level, proteinuria, elevated liver enzymes and hyper gammaglobulinemia.
How is Polyarteritis Nodosa Treated?
Polyarteritis Nodosa is treated with corticosteroids and cyclophosphamide.
What is the Prognosis of Polyarteritis Nodosa?
The prognosis of polyarteritis nodosa with cutaneous manifestation has better prognosis than those with abdominal manifestation.