Polyarteritis nodosa is a necrotizing and systemic vasculitis relating to multiple organs and tissues’ small and medium-sized muscular arteries.
What is the Pathology of Polyarteritis Nodosa?
The pathology of polyarteritis nodosa is:
-Etiology: The cause of polyarteritis nodosa is genetic factors, other conditions such as hepatitis B.
-Genes involved: CECR1(ADA2).
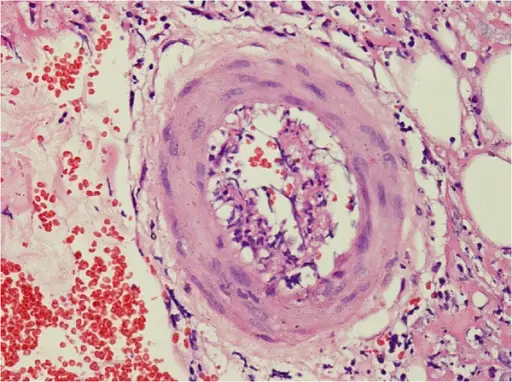
-Pathogenesis: The sequence of events that lead to polyarteritis nodosa are not well known. Believed to be due to Inflammation of the medium-sized muscular arteries. Originate at the vessel, intima progresses to comprise the whole arterial wall, destroying the entire elastic lamina, resulting in fibrinoid necrosis, aneurysms, and sometimes thrombi.
-Morphology: The morphology associated with polyarteritis nodosa shows necrotizing inflammation of arteries.
-Histology: The histology associated with polyarteritis nodosa shows neutrophils, eosinophils, and mononuclear cells present at the site of the lesion.
How does Polyarteritis Nodosa Present?
Patients with polyarteritis nodosa typically affect men more often than women present at an age range of 20 to 40. The symptoms, features, and clinical findings associated with polyarteritis nodosa include fever of unknown cause, malaise, weight loss, bloody stool, abdominal pain, and hypertension.
How is Polyarteritis Nodosa Diagnosed?
Polyarteritis nodosa is diagnosed through the clinical presentation. Imaging studies- angiography disclose stenoses and larger aneurysms. Laboratory studies- establish the systemic nature of the condition, elevated ESR, Hepatitis B surface antigen test, proteinuria.
How is Polyarteritis Nodosa Treated?
Polyarteritis nodosa is treated through medical care, corticosteroid therapy, cyclophosphamide therapy.
What is the Prognosis of Polyarteritis Nodosa?
The prognosis of polyarteritis nodosa is good in cutaneous PAN without systemic involvement.