Pulmonary eosinophilia is a group of immunologically-mediated lung diseases categorized by a 2 features: Infiltration of the lungs in chest radiographs and raised eosinophil count in the peripheral blood.
Examples of pulmonary eosinophilia that cause restrictive lung diseases are:
- Acute eosinophilic pneumonia with respiratory failure
- Idiopathic chronic eosinophilic pneumonia
- Secondary eosinophilia
What is the Pathology of Pulmonary Eosinophilia?
The pathology of pulmonary eosinophilia is:
-Etiology: The cause of pulmonary eosinophilia is infections, ingested or substances inhaled, drugs like cocaine. Contaminated cooking oil, and dietary supplements L-tryptophan.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary eosinophilia is unknown in some types like Loffler Syndrome.
-Histology: The histology associated with pulmonary eosinophilia shows thickened alveolar walls by edema and exudate, chiefly of eosinophils, lymphocytes, and plasma cells.
How does Pulmonary Eosinophilia Present?
Patients with pulmonary eosinophilia typically have a male-to-female ratio around 4:1, present at age range of 20-50 years. The symptoms, features, and clinical findings associated with pulmonary eosinophilia include progressing dyspnea, myalgias, abdominal complaints, pruritic rash, rhinitis/sinusitis, distension of jugular venous, peripheral edema.
How is Pulmonary Eosinophilia Diagnosed?
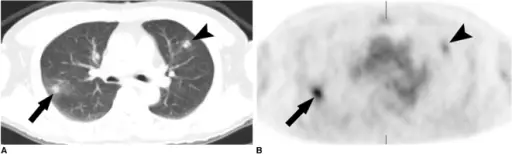
Pulmonary eosinophilia is diagnosed pulmonary function test. Laboratory Studies- stool examination, leukocyte count, serologic testing. Imaging Studies- Chest CT scan and Chest radiography.
How is Pulmonary Eosinophilia Treated?
Pulmonary eosinophilia is treated through oxygen therapy, medical care- bronchodilator therapy, steroid therapy.
What is the Prognosis of Pulmonary Eosinophilia?
The prognosis of pulmonary eosinophilia is fair.