Pulmonary pathology is the scientific study of ailments to the lungs affecting its functions and structural responsibilities.
What are Congenital Anomalies of the Pulmonary System?
Congenital anomalies of the pulmonary system are developmental abnormalities of the lungs.
Examples of congenital anomalies of the pulmonary system include:
Table showing congenital anomalies of the pulmonary system
| Agents | Diseases |
| Coal | Simple coal-workers’ pneumoconiosisProgressive massive fibrosisCaplan’s syndrome |
| Silica | SilicosisCaplan’s syndrome |
| Asbestos | Asbestosis Pleural diseasesTumors |
| Beryllium | Berylliosis |
| Mouldy hay | Farmer’s lung |
What is Atelectasis?
Atelectasis is the fractional or total complete collapse of the lung or a specific portion of the lung. Incomplete expansion of the lungs (Neonatal Atelectasis).
What is the Pathology of Atelectasis?
The pathology of atelectasis is: Incomplete expansion of the lungs or partial/total Collapse collapse of the lungs leading to impaired gaseous exchange.
-Etiology: The cause of atelectasis is, impaired surfactant production, bronchial impediment by foreign bodies, growths, Plugs of sputum, or endobronchial tumors, hyaline membrane disease, pleural effusion. Causes grouped into congenital or acquired(Resorption, Compression, and contraction atelectasis)
-Genes involved: surfactant protein A (SPA1, SPA2)
-Pathogenesis: The sequence of events that lead to atelectasis is collapsed alveoli.
-Histology: The histology associated with atelectasis shows collapsed alveoli.
How does Atelectasis Present?
Patients with atelectasis typically have no gender predilection, present at age range of 60 years. The symptoms, features, and clinical findings associated with atelectasis include chest pain, abrupt dyspnea, and cyanosis, tachycardia hypotension, shock and fever.
How is Atelectasis Diagnosed?
Atelectasis is diagnosed through laboratory studies, ABGs determine hypoxemia. Imaging studies, CT scans, and chest radiology check for lobar collapse. Bronchoscopy assesses bronchial obstruction.
How is Atelectasis Treated?
Atelectasis is treated through medical care, oxygen therapy, mechanical and intubation support, CPAP, a broad-spectrum antibiotic, treatment of underlying causes, chest physiotherapy, and nebulization.
What is the Prognosis of Atelectasis?
The prognosis of atelectasis is fair.
What is Pulmonary Edema?
Pulmonary edema is a life-threatening emergency characterized by excessive interstitial fluid that accumulates in the alveolar space.
What is the Pathology of Pulmonary Edema?
The pathology of pulmonary edema is: The anomaly resulting from hemodynamic disturbances (hemodynamic or cardiogenic pulmonary edema) or direct increases in capillary permeability, owing to microvascular injury.
-Etiology: The cause of pulmonary edema is, lymphatic impediment, injury to the alveolar-capillary barrier, reduced plasma oncotic pressure, augmented negative interstitial pressure, and Idiopathic mechanism.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary edema is as follows, Augmented pressure/pooling, leads to amplified pulmonary venous pressure, which leads to augmented pulmonary capillary pressure further leading to fluid in interstitial spaces causing augmented pressure in Interstitial spaces hence resulting to pulmonary edema (fluid in alveoli).
-Histology: The histology associated with pulmonary edema shows the pulmonary venules and alveolar capillaries are dilated and engorged with blood. The alveolar walls are thickened due to edema and later due to fibrosis. The alveolar spaces contain RBCs and many large macrophages with brownish hemosiderin pigment granules.
How does Pulmonary Edema Present?
Patients with pulmonary edema typically Men are affected more than women, present at age range of above 50 years. The symptoms, features, and clinical findings associated with pulmonary edema include breathlessness, wheezing, anxiety, sweating, frothy, blood-tinged sputum, and tachypnoeic with peripheral shutdown
How is Pulmonary Edema Diagnosed?
Pulmonary edema is diagnosed in Laboratory studies, complete blood count to assess anemia. pulse oximetry assessing hypoxia, arterial blood gas analysis, blood urea nitrogen level. Imaging studies, electrocardiography, CT scanning.
How is Pulmonary Edema Treated?
Pulmonary edema is treated as an emergency. General, Addressing (ABC) Airway, Breathing, Circulation. Prop up, oxygen therapy, mechanical and ventilatory support, IV access, and monitoring urine output. Underlying cause treatment, Noninvasive pressure-support ventilation CPAP, and BiPAP. Nitroglycerin for preload reduction. Diuretics. ACE inhibitors for afterload reduction.
What is the Prognosis of Pulmonary Edema?
The prognosis of pulmonary edema is poor especially in patients with congestive heart failure.
What is Hemodynamic Pulmonary Edema?
Hemodynamic Pulmonary Edema is a life-threatening type of Pulmonary edema due to increased hydrostatic pressure. Can be caused by left-sided congestive heart failure.
What is Noncardiogenic Pulmonary Edema?
Noncardiogenic pulmonary edema is the abrupt onset of bilateral pulmonary infiltrates and significant hypoxemia.
What is Acute Lung Injury?
Acute lung injury is an ailment of acute inflammation causing interruption of the lung endothelial and epithelial barriers.
What is the Pathology of Acute Lung Injury?
The pathology of acute lung injury is:
-Etiology: The cause of acute lung injury is acute lung injury.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acute lung injury is unclear, although both local and systemic inflammatory responses occur. accumulate neutrophils are considered to play a role in the pathogenesis. Activated neutrophils release proteolytic enzymes, toxic oxygen species, and phospholipid products that upsurge the inflammatory response and cause more damage to the capillary alveolar epithelium and endothelium.
-Histology: The histology associated with acute lung injury shows injury of alveolar-capillary membrane integrity, extreme transepithelial neutrophil relocation, and pro-inflammatory, cytotoxic mediators release.
How does Acute Lung Injury Present?
Patients with acute lung injury typically have no gender prevalence present at age range of any age. The symptoms, features, and clinical findings associated with acute lung injury include respiratory distress, an increase in respiratory rate, and signs of respiratory failure, and hypoxemia.
How is Acute Lung Injury Diagnosed?
Acute lung injury is diagnosed through laboratory tests, with PaO2 less than 300, alkalosis in ABGs test. Imaging studies, Radiography, CT scans, and echocardiography.
How is Acute Lung Injury Treated?
Acute lung injury is treated through mechanical and ventilatory support.
What is the Prognosis of Acute Lung Injury?
The prognosis of acute lung injury is fair.
What is Acute Respiratory Distress Syndrome?
Acute respiratory distress syndrome is a clinical syndrome characterized by one week of respiratory distress, bilateral opacities, edema, and PaO2/FiO2 ratio <200, caused by progressive respiratory insufficiency due to diffuse alveolar damage.
What is the Pathology of Acute Respiratory Distress Syndrome?
The pathology of acute respiratory distress syndrome is:
-Etiology: The cause of acute respiratory distress syndrome is direct lung injuries, burns, bacteremia, massive transfusion, sepsis, pneumonia, fractures, aspiration near-drowning fat embolism.
-Genes involved: FAS gene.
-Pathogenesis: The sequence of events that lead to acute respiratory distress syndrome are diffuse damage to the alveolar-capillary walls, followed by a relatively nonspecific, often predictable series of morphologic and physiologic alterations leading to respiratory failure.
-Histology: The histology associated with acute respiratory distress syndrome shows diffuse alveolar injury, thickened alveolar walls, and the presence of hyaline membranes.
How does Acute Respiratory Distress Syndrome Present?
Patients with acute respiratory distress syndrome typically have no gender prevalence present at any age range. The symptoms, features, and clinical findings associated with acute respiratory distress syndrome include acute hypoxemia and dyspnea, clinically ill, tachycardia, agitation, anxiety, tachypnea, low PaO2/FiO2 ratio, bilateral rales on lung examination, cyanosis, peripheral vasoconstriction, and hypotension.
How is Acute Respiratory Distress Syndrome Diagnosed?
Acute respiratory distress syndrome is diagnosed through laboratory tests, ABGs. Imaging studies, Radiography indicate bilateral rales, CT scans, and echocardiograph.
How is Acute Respiratory Distress Syndrome Treated?
Acute respiratory distress syndrome is treated through mechanical and ventilatory support.
What is the Prognosis of Acute Respiratory Distress Syndrome?
The prognosis of acute respiratory distress syndrome is poor associated with a high mortality rate due to its complications.
What is Acute Interstitial Pneumonia?
Acute interstitial pneumonia is a rare and fulminant form of idiopathic interstitial widespread acute lung injury associated with sudden onset of dyspnea and rapid pulmonary decline.
What is the Pathology of Acute Interstitial Pneumonia?
The pathology of acute interstitial pneumonia is:
-Etiology: The cause of acute interstitial pneumonia is unknown
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to is acute interstitial pneumonia alveolar damage.
-Histology: The histology associated with acute interstitial pneumonia shows diffuse alveolar injury, diffuse interstitial fibrosis thicken spindle cell proliferation.
How does Acute Interstitial Pneumonia Present?
Patients with acute interstitial pneumonia typically have no gender preference, present at age range of the mean of 54years. The symptoms, features, and clinical findings associated with acute interstitial pneumonia include acute hypoxemia and dyspnea, clinically ill, tachycardia, agitation, anxiety, tachypnea,on lung examination, cyanosis, peripheral vasoconstriction, and hypotension.
How is Acute Interstitial Pneumonia Diagnosed?
Acute interstitial pneumonia is diagnosed through Imaging studies, Radiography indicates bilateral rales, CT scans, Echocardiograph with features overlapping those of acute respiratory distress syndrome.
How is Acute Interstitial Pneumonia Treated?
Acute interstitial pneumonia is treated through mechanical and ventilator support.
What is the Prognosis of Acute Interstitial Pneumonia?
The prognosis of acute interstitial pneumonia is poor with a mortality rate of about 50%, most deaths happening within 1 to 2 months of the disease.
What is Obstructive Lung Disease?
Obstructive Lung Diseases is one of the category of diffuse pulmonary ailment, an airway diseases characterized by an increase in resistance to airflow due to complete or partial obstruction of the respiratory tree.
Examples of obstructive lung disease include:
- Asthma
- Bronchiectasis
- Chronic bronchitis
- Emphysema
- Bronchiolitis
What is Asthma?
Asthma is immunologic bronchoconstriction, inflammation, and mucus production due to increased airway sensitivity.
Types of asthma include:
Atopic Asthma
Drug-Induced Asthma
Exercise-Induced Asthma
Non-Atopic Asthma
Occupational Asthma
What is the Pathology of Asthma?
The pathology of asthma is:
-Etiology: The cause of asthma is, atopy, environmental factor including sensitizing chemicals, air pollution by allergens, or indoor allergens. Over
-Genes involved: ORMDL3 gene.
-Pathogenesis: The sequence of events that lead to asthma areas follows. Airway inflammation. Walls are infiltrated by inflammatory cells, eosinophils, neutrophils, plasma, cells, and lymphocytes which causes hyperemia, mucosal and submucosal edema. Intermittent airflow obstruction due to edema and finally bronchial hyperresponsiveness.
-Histology: The histology associated with asthma shows permeation of the inflammatory cells, airway lumina taping, mucus masses, and bronchial/bronchiolar epithelial stripping.
How does Asthma Present?
Patients with asthma typically a male-to-female ratio of 2:1 in children and 1:1 in adults, present at age range of 18 years. The symptoms, features, and clinical findings associated with asthma include chest tightness, wheezing, shortness of, breath and cough frequently worse at night.
How is Asthma Diagnosed?
Asthma is diagnosed through medical and physical examination, laboratory studies which include Spirometry assessments, Peak Flow Monitoring, Sputum and Blood Eosinophils ( Blood eosinophil >4% indicate asthma), Serum Immunoglobulin E > 100 IU, Arterial Blood Gas, Pulse Oximetry Assessment, Allergy Skin Testing. Imaging studies, Chest radiography, Chest CT scanning, Electrocardiography, Nuclear Imaging, MRI.
How is Asthma Treated?
Asthma is treated through environmental control for allergens and pharmacologic treatment.
What is the Prognosis of Asthma?
The prognosis of asthma is good with proper treatment and management.
What is Bronchiectasis?
Bronchiectasis is permanent dilation of bronchi and bronchioles due to destruction of smooth muscle and elastic tissue by chronic necrotizing infections.
What is the Pathology of Bronchiectasis?
The pathology of bronchiectasis is:
-Etiology: The cause of bronchiectasis is persistent or severe infections, Congenital anatomic defects, Allergic bronchopulmonary aspergillosis, Connective-tissue disorders, Immunodeficiency states,
-Genes involved: Cytotoxic T-lymphocyte antigen (CTLA) 4.
-Pathogenesis: The sequence of events that lead to bronchiectasis, after episodes of infections the bronchial walls are enfeebled and lack support, and are extended by the force of inspiration. The dilated bronchi become packed together with loss of the prevailing lung parenchyma. Squamous metaplasia often follows and eventually the cavities become chronically infected.
-Histology: The histology associated with bronchi shows a marked increase in goblet cells and excess mucus production with plugging of the airway lumen, inflammatory infiltration, and fibrosis of the bronchiolar wall. The pleura in the affected area is adherent and shows bands of fibrous tissue.
How does Bronchiectasis Present?
Patients with bronchiectasis typically affect females than males present at age range of 60 years. The symptoms, features, and clinical findings associated with bronchiectasis include recurrent bronchopulmonary infection; coughing; production of copious amounts of foul-smelling, purulent sputum; and hemoptysis. Weight loss and anemia are common.
How is Bronchiectasis Diagnosed?
Bronchiectasis is diagnosed based on history and imaging studies, chest radiographs. Chest CT scanning allows for definitive diagnosis.
How is Bronchiectasis Treated?
Bronchiectasis is treated through acknowledgment and treatment of episodic infections, regular postural drainage, and chest physical therapy.
What is the Prognosis of bronchiectasis?
The prognosis of bronchiectasis is good when treatment regimens are adhered to.
What is Chronic Bronchitis?
Chronic bronchitis is a common chronic condition defined Persistent cough with sputum for minimum of three months in at least two consecutive years not due to another cause. Typically associated with smoking.
What is the Pathology of Chronic Bronchitis?
The pathology of chronic bronchitis is:
-Etiology: The cause of chronic bronchitis is, atmospheric pollution and cigarette smoking (Most common). Other factors are genetic factors, occupation, and infection.
-Genes involved: Cytotoxic T-lymphocyte antigen (CTLA) 4.
-Pathogenesis: The sequence of events that lead to chronic bronchitis results from a succession of occurrences of acute bronchitis. Throughout,bronchial-lining tissue cells are irritated, the mucous membrane turns out to be hyperemic, edematous, weakening bronchial mucociliary purpose. May also progress progressively due to inhalation of air contaminated with pollutants or heavy smoking.
-Histology: The histology associated with chronic bronchitis shows increased Reid index, epithelium show squamous metaplasia and dysplasia, and little inflammatory cell infiltrate.
How does Chronic Bronchitis Present?
Patients with chronic bronchitis typically affect males more compared to females present at age range of >50 years. The symptoms, features, and clinical findings associated with chronic bronchitis include Cough, sputum production, nausea, vomiting, sore throat, fever general malaise, and chest pain.
How is Chronic Bronchitis Diagnosed?
Chronic bronchitis is diagnosed through history taking (persistent cough with expectoration on most days for at least three months of the year for two or more consecutive years), cultures, and staining for influenza virus. Imaging studies, Chest radiography, Bronchoscopy exclude tumors and aspiration.
How is Chronic Bronchitis Treated?
Chronic bronchitis is treated through symptom and episodic infection treatment, environmental changes.
What is the Prognosis of Chronic Bronchitis?
The prognosis of Chronic Bronchitis is good. The condition is self-limited
What is Emphysema?
Emphysema is a condition of the lung characterized by airspaces distal to the terminal bronchiole becoming destroyed, and there is an irreversible enlargement of the airspaces.
Types of emphysema included:
Airspace Enlargement with Fibrosis (Irregular Emphysema)
Bullous Emphysema
Compensatory Hyperinflation
Centriacinar (Centrilobar)
Distal Acinar (Paraseptal)
Interstial Emphysema
Obstructive Overinflation
Panacinar (Panlobar)
Alpha-1-Antitrypsin Deficiency
What is the Pathology of Emphysema?
The pathology of emphysema is:
-Etiology: The cause of emphysema is Tobacco smoking others include inhalation exposure to chemical vapors, mineral specks of dust, organic dust metal fumes, and exhaust fumes.
-Genes involved: Cytotoxic T-lymphocyte antigen (CTLA) 4.
-Pathogenesis: The sequence of events that lead to emphysema thought to result from the elastin and other alveolar wall components breakdown by enzymes, proteases, that digest protein. Infiltration by foreign antigen to lung epithelial cell barrier, inflammatory immune cells carry the antigens to BALT layer where Proteolytic reaction takes place damaging lungs epithelial.
-Histology: The histology associated with emphysema shows dilation of air spaces and injuries of septal walls of part of acinus intricate.
How does Emphysema Present?
Patients with emphysema typically have gender differences in the prevalence of smoking with females more likely to develop than males, present at age range of > 50 years. The symptoms, features, and clinical findings associated with emphysema include productive cough, dyspnea, wheezing, and acute chest illness.
How is Emphysema Diagnosed?
Emphysema is diagnosed through Spirometry assessment, Arterial blood gas analysis, sputum evaluation, and hematocrit. Imaging Studies, chest radiograph reveals hyper infiltration and HRCT scanning of the chest.
How is Emphysema Treated?
Emphysema is treated through, smoking cessation, medical care for symptoms- bronchodilators, phosphodiesterase inhibitors, anti-inflammatory therapy antibiotics, and oxygen therapy.
What is the Prognosis of Emphysema?
The prognosis of emphysema is fair.
What is Bronchiolitis?
Bronchiolitis is a condition characterized by acute inflammatory damage to the bronchioles that are typically instigated by viral infections.
What is the Pathology of Bronchiolitis?
The pathology of bronchiolitis is:
-Etiology: The cause of bronchiolitis is an inhalation injury, infection, drug or chemical-induced reactions, connective tissue diseases, organ transplantation, and idiopathic.
-Genes involved: Cytotoxic T-lymphocyte antigen (CTLA) 4.
-Pathogenesis: The sequence of events that lead to bronchiolitis are: Goblet cells Proliferation marks an excessive mucus production. Chemokines and cytokines from ill respiratory epithelial cells, intensify cellular enrolment into infected airways by immune response resulting in inflammation, edema which obstruct bronchioles.
-Histology: The histology associated with bronchiolitis shows bronchiolar inflammation, peribronchiolar fibrosis and obliterative fibrosis of the bronchiolar lumen.
How does Bronchiolitis Present?
Patients with bronchiolitis typically more frequently in males than in females present at age range of 1 to 2 years with peaks at 2 to 8 months. The symptoms, features, and clinical findings associated with bronchiolitis include breathlessness, wheezing rapid shallow breathing, cough, and retractions of lower ribs and sternum during inspiration.
How is Bronchiolitis Diagnosed?
Bronchiolitis is diagnosed through a medical history and physical exam, laboratory studies- WBC Count and differential, pulse oximetry, viral testing. Imaging chest radiography.
How is Bronchiolitis Treated?
Bronchiolitis is treated through symptomatic relief, oxygen therapy, medical treatment- Anti-inflammatory agents, bronchodilators, antivirals, and antibiotics.
What is the Prognosis of Bronchiolitis?
The prognosis of bronchiolitis is good with mortality ranging from 0.2% to 7%.
What is Restrictive Lung Disease?
Restrictive lung disease is a diverse category of lung ailments producing similar inflammatory and fibrotic changes in the interstitium or interalveolar septa of the lung. Characterized by decreased total lung capacity and reduced expansion of lung parenchyma.
Examples of restrictive lung disease include:
- Fibrosing diseases
- Granulomatous diseases
- Pulmonary alveolar proteinosis
- Pulmonary eosinophilia
- Pulmonary langerhans cell histiocytosis
- Smoking-related interstitial diseases
- Surfactant dysfunction disorders
What are Fibrosing Diseases that Cause Restrictive Lung Diseases?
Fibrosing diseases that cause restrictive lung diseases are diseases of the lungs that cause fibrosis.
Examples of Fibrosing diseases that cause restrictive lung diseases are:
- Complications of therapies
- Cryptogenic organizing pneumonia
- Idiopathic pulmonary fibrosis
- Nonspecific interstitial pneumonia
- Pneumoconioses
- Pulmonary involvement in autoimmune diseases
What is Cryptogenic Organizing Pneumonia?
Cryptogenic organizing pneumonia is a clinicopathologic disorder that swiftly resolves with corticosteroids treatment, and has high relapses frequency when management is stopped.
What is the Pathology of Cryptogenic Organizing Pneumonia?
The pathology of cryptogenic organizing pneumonia is:
-Etiology: The cause of cryptogenic organizing pneumonia is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to cryptogenic organizing pneumonia alveolar epithelial damage owing to a mysterious provoking insult, believed to cause plasma proteins leakage to the alveolar space resultant in the recruitment of inflammatory cells, fibrin bands formation mononuclear inflammatory cells along with infiltration at the intra-alveolar stage. fibroblasts proliferation of laying down reticulin framework. Finally, formation of connective tissue and fibroblasts matrix.
-Histology: The histology associated with cryptogenic organizing pneumonia shows polypoid plugs of loose organizing connective tissue in alveolar ducts, alveoli, and often bronchioles.
How does Cryptogenic Organizing Pneumonia Present?
Patients with cryptogenic organizing pneumonia typically both genders affected equally, present at age range of 50 to 60 years. The symptoms, features, and clinical findings associated with Cryptogenic organizing pneumonia include cough, dyspnea, have subpleural or peribronchial patchy areas of airspace consolidation on radiographically.
How is Cryptogenic Organizing Pneumonia Diagnosed?
cryptogenic organizing pneumonia is diagnosed through laboratory studies, WBC count with elevated neutrophilia, high ESR and c-reactive protein. Imaging studies, chest radiograph showing diffuse patchy consolidations, and lung CT scan shows bilateral patchy consolidation.
How is Cryptogenic Organizing Pneumonia Treated?
Cryptogenic organizing pneumonia is treated through medica care with steroids- oral glucocorticoids, prednisolone (IV).
What is the Prognosis of Cryptogenic Organizing Pneumonia?
The prognosis of cryptogenic organizing pneumonia is good, some patients recover spontaneously while others need oral steroids treatment for 6 months or longer for complete recovery.
What is Idiopathic Pulmonary Fibrosis?
Idiopathic Pulmonary Fibrosis is a chronic progressive syndrome of the lungs with 3–5 years projected median survival time after diagnosis was made.
What is the Pathology of Idiopathic Pulmonary Fibrosis?
The pathology of idiopathic pulmonary fibrosis is:
-Etiology: The cause of idiopathic pulmonary fibrosis is unknown
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to idiopathic pulmonary fibrosis is unknown.
-Histology: The histology associated with idiopathic pulmonary fibrosis shows alveolar exudate, fibrosis in the alveoli, and the interstitial septal wall with inconstant inflammation.
How does Idiopathic Pulmonary Fibrosis Present?
Patients with idiopathic pulmonary fibrosis typically males are affected more frequently, and present at age range of 20 to 45 years. The symptoms, features, and clinical findings associated with idiopathic pulmonary fibrosis include a dry cough and slowly developing dyspnea, cor-pulmonale fingers clubbing.
How is Idiopathic Pulmonary Fibrosis Diagnosed?
Idiopathic pulmonary fibrosis is diagnosed by excluding all known causes of interstitial fibrosis.
How is Idiopathic Pulmonary Fibrosis Treated?
Idiopathic pulmonary fibrosis is treated medical care-, pirfenidone and nintedanib antifibrotic drugs slow the lung functions weakening.
What is the Prognosis of Idiopathic Pulmonary Fibrosis?
The prognosis of idiopathic pulmonary fibrosis is poor, death within 6 weeks to 6 months.
What is Nonspecific Interstitial Pneumonia?
Nonspecific Interstitial Pneumonia is an anomaly that could not be classified into one of the idiopathic interstitial pneumonia types.
What is the Pathology of Nonspecific Interstitial Pneumonia?
The pathology of nonspecific interstitial pneumonia is:
-Etiology: The cause of nonspecific interstitial pneumonia is idiopathic, associated with systemic ailments and exposures to some drugs
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to nonspecific interstitial pneumonia is unknown.
-Histology: The histology associated with nonspecific interstitial pneumonia shows a temporally unvarying interstitial course with fluctuating sizes to the fibrosis and interstitial inflammation.
How does Nonspecific Interstitial Pneumonia Present?
Patients with nonspecific interstitial pneumonia typically have an insignificant female prevalence, present at age range of 46 and 55 years. The symptoms, features, and clinical findings associated with nonspecific interstitial pneumonia include shortness of breath for some months, cough, weight loss, and fever.
How is Nonspecific Interstitial Pneumonia Diagnosed?
Nonspecific interstitial pneumonia is diagnosed through transbronchial biopsy, a High-resolution CT scan to differentiate from usual interstitial pneumonia.
How is Nonspecific Interstitial Pneumonia Treated?
Nonspecific interstitial pneumonia is treated medical care corticosteroid therapy and follow-up.
What is the Prognosis of Nonspecific Interstitial Pneumonia?
The prognosis of nonspecific Interstitial pneumonia is good as many clients respond well to corticosteroid therapy.
What are Pneumoconioses?
Pneumoconioses are a group of interstitial lung diseases usually caused by inhalation of dust, mostly at work.
What is the Pathology of Pneumoconioses?
The pathology of pneumoconioses is:
-Etiology: The cause of pneumoconioses is occupational exposure to specific airborne agents.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pneumoconioses is as follows inhaled particles deposited at the distal airways and alveoli. There is phagocytizing of the particles by macrophages. profibrotic pathways and proinflammatory are activated. Consequent exposure and ingestion of dust by macrophages causes cell necrosis and autophagy, repeated cycles cause advanced alveolar fibrosis and inflammation.
-Histology: The histology associated with pneumoconioses shows aggregates of dust-laden macrophages at the bronchiolar and alveolar walls. Distended bronchioles and alveoli surrounding the macules.
Table of Common Pneumoconiosis
| Agents | Diseases |
| Coal | Simple coal-workers’ pneumoconiosisProgressive massive fibrosisCaplan’s syndrome |
| Silica | SilicosisCaplan’s syndrome |
| Asbestos | Asbestosis Pleural diseasesTumors |
| Beryllium | Berylliosis |
| Mouldy hay | Farmer’s lung |
How does Pneumoconiosis Present?
Patients with pneumoconiosis typically have varying preferences male workers affected most. present at age range of above 45 years. The symptoms, features, and clinical findings associated with pneumoconiosis include; exercise tolerance reduction, the steady beginning of a cough nonproductive, some are symptomless with an anomalous chest X-ray.
How is Pneumoconiosis Diagnosed?
Pneumoconiosis is diagnosed through a history of long-time exposure to agents. Pulmonary function tests show a characteristic restrictive outline. Imaging studies- chest X-ray, CT scan showing small diffuse nodules.
How is Pneumoconiosis Treated?
Pneumoconiosis is treated through enhanced workout tolerance and avoidance of causative exposure. There is no cure.
What is the Prognosis of Pneumoconiosis?
The prognosis of pneumoconiosis is poor in a fibrotic stage of illnesses.
What is Pulmonary Involvement in Autoimmune Diseases?
Pulmonary involvement in autoimmune diseases is when collagen vascular diseases involve the lung to a slighter or more degree in their course.
What is the Pulmonary Involvement in Autoimmune Diseases?
The pathology of pulmonary involvement in autoimmune diseases is:
-Etiology: The cause of pulmonary involvement in autoimmune diseases are; rheumatoid arthritis systemic lupus erythematosus, scleroderma, mixed connective tissue disease, and dermatomyositis-polymyositis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary involvement in autoimmune diseases: Diffuse interstitial fibrosis pattern happens typically in scleroderma.
-Histology: The histology associated with pulmonary involvement in autoimmune diseases shows patchy, transient parenchymal infiltrates in lupus erythematosus.
How does Pulmonary Involvement in Autoimmune Diseases Present?
Patients with pulmonary involvement in autoimmune diseases typically, males more affected than females, present at the age range of 46 and 55 years. The symptoms, features, and clinical findings associated with nonspecific interstitial pneumonia include shortness of breath for some months, cough, weight loss, and fever.
How is Pulmonary Involvement in Autoimmune Diseases Diagnosed?
Pulmonary involvement in autoimmune diseases is diagnosed through the diagnosis of ailment it presents in. Transbronchial biopsy, a High-resolution CT scan to differentiate from usual interstitial pneumonia.
How is Pulmonary Involvement in Autoimmune Diseases Treated?
Pulmonary involvement in autoimmune diseases is treated through specific treatment of systemic autoimmune disease present.
What is the Prognosis of Pulmonary Involvement in Autoimmune Diseases?
The prognosis of pulmonary involvement in autoimmune diseases is poor.
What are Granulomatous diseases that cause restrictive lung diseases?
Granulomatous diseases that cause restrictive lung diseases are an assorted group of illnesses with a wide range of pathologies with inconstant clinical appearances and outcomes.
Examples of granulomatous diseases that cause restrictive lung diseases are:
- Hypersensitivity pneumonitis
- Sarcoidosis
What is Hypersensitivity Pneumonitis?
Hypersensitivity pneumonitis is a range of immunologically arbitrated, predominantly interstitial, lung ailments caused by intense, and prolonged contact to inhaled organic specks of dust and related job-related antigens.
What is the Pathology of Hypersensitivity Pneumonitis?
The pathology of hypersensitivity pneumonitis is:
-Etiology: The cause of hypersensitivity pneumonitis is reactivity to an antigen which include, thermoactinomyces sacchari, avian or animal proteins, saccharopolyspora rectivirgula among others.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to hypersensitivity pneumonitis are partly understood. Thought to happen chiefly through type III hypersensitivity response for acute hypersensitivity. Chronic hypersensitivity pneumonitis is believed to be a result of type IV, T-cell mediated responses.
-Histology: The histology associated with hypersensitivity pneumonitis shows interstitial pneumonitis entailing lymphocytes, plasma cells, and macrophages. Noncaseating granulomas, interstitial fibrosis, and obliterative bronchiolitis may also be seen.
How does Hypersensitivity Pneumonitis Present?
Patients with hypersensitivity pneumonitis typically males are more affected than females present at age range of 40 to60 years. The symptoms, features, and clinical findings associated with hypersensitivity pneumonitis include episodes of fever, dyspnea, cough, and leukocytosis. On chest radiograph, diffuse and nodular infiltrates appear.
How is Hypersensitivity Pneumonitis Diagnosed?
Hypersensitivity pneumonitis is diagnosed through physical and history examination, Imaging- Chest radiograph and CT scan display radiographic indication. Bronchoscopic alveolar lavage displays an indication of lymphocytic predominance.
How is Hypersensitivity Pneumonitis Treated?
Hypersensitivity pneumonitis is treated through antigen avoidance, medical care- corticosteroid therapy, antihistamines, bronchodilators, and cromolyn sodium.
What is the Prognosis of Hypersensitivity Pneumonitis?
The prognosis of hypersensitivity pneumonitis is poor especially on an indication of pulmonary fibrosis.
What is Sarcoidosis?
Sarcoidosis is a systemic ailment of mysterious cause characterized by noncaseating granulomas in several tissues and organs.
What is the Pathology of Sarcoidosis?
The pathology of sarcoidosis is:
-Etiology: The cause of sarcoidosis is unknown.
-Genes involved: HLA genotypes (class I HLA-A1 and HLA-B8).
-Pathogenesis: The sequence of events that lead to sarcoidosis is not fully understood, some evidence proposes that it is an illness of disordered immune regulation in genetically susceptible persons exposed to certain agents.
-Histology: The histology associated with sarcoidosis shows lesions that are disseminated along the lymphatics, around the bronchi, and blood vessels.
How does Sarcoidosis Present?
Patients with sarcoidosis typically male-to-female ratio is roughly 1:2. present at age range of 25-35 years. The symptoms, features, and clinical findings associated with sarcoidosis include the onset of shortness of breath, cough, chest pain, hemoptysis, fever, fatigue, weight loss, anorexia, night sweats.
How is Sarcoidosis Diagnosed?
Sarcoidosis is diagnosed through laboratory Studies- Serum markers of sarcoidosis (sIL-2R), (SAA) (ACE). Imaging Studies-Chest radiograph and High-resolution CT scan detect fibrosis and active alveolitis.
How is Sarcoidosis Treated?
Sarcoidosis is treated through medical care- steroid treatment and surgical care lung transplantation.
What is the Prognosis of Sarcoidosis?
The prognosis of sarcoidosis is good with 65% to 70% of affected patients recovering with minimal or no residual manifestations.
What is Pulmonary Alveolar Proteinosis?
Pulmonary alveolar proteinosis is rare chronic illness where distal airspaces of the lungs are filled with granular, PAS-positive, eosinophilic material with abundant lipid in it.
Examples of pulmonary alveolar proteinosis that cause restrictive lung diseases are:
- Autoimmune pulmonary alveolar proteinosis
- Hereditary pulmonary alveolar proteinosis
- Secondary pulmonary alveolar proteinosis
What is the Pathology of Pulmonary Alveolar Proteinosis?
The pathology of pulmonary alveolar proteinosis is:
-Etiology: The cause of pulmonary alveolar proteinosis is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary alveolar proteinosis is unknown.
-Histology: The histology associated with pulmonary alveolar proteinosis shows the presence of homogeneous, granular, eosinophilic material which stains brightly with PAS.
How does Pulmonary Alveolar Proteinosis Present?
Patients with pulmonary alveolar proteinosis typically males are more affected than females, present at age range of 20-50years. The symptoms, features, and clinical findings associated with pulmonary alveolar proteinosis include dyspnoea, cough, chest pain, pyrexia, fatigue and loss of weight confluent. Areas of consolidation on a chest x-ray
How is Pulmonary Alveolar Proteinosis Diagnosed?
Pulmonary alveolar proteinosis is diagnosed through Imaging studies- Chest radiographs, X-rays, and CT scans.
How is Pulmonary Alveolar Proteinosis Treated?
Pulmonary alveolar proteinosis is treated through therapeutic whole-lung lavage.
What is the Prognosis of Pulmonary Alveolar Proteinosis?
The prognosis of pulmonary alveolar proteinosis is good on effective treatment.
What is Pulmonary Eosinophilia?
Pulmonary eosinophilia is a group of immunologically-mediated lung diseases categorized by a 2 features: Infiltration of the lungs in chest radiographs and raised eosinophil count in the peripheral blood.
Examples of pulmonary eosinophilia that cause restrictive lung diseases are:
- Acute eosinophilic pneumonia with respiratory failure
- Idiopathic chronic eosinophilic pneumonia
- Secondary eosinophilia
What is the Pathology of Pulmonary Eosinophilia?
The pathology of pulmonary eosinophilia is:
-Etiology: The cause of pulmonary eosinophilia is infections, ingested or substances inhaled, drugs like cocaine. Contaminated cooking oil, and dietary supplements L-tryptophan.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary eosinophilia is unknown in some types like Loffler Syndrome.
-Histology: The histology associated with pulmonary eosinophilia shows thickened alveolar walls by edema and exudate, chiefly of eosinophils, lymphocytes, and plasma cells.
How does Pulmonary Eosinophilia Present?
Patients with pulmonary eosinophilia typically have a male-to-female ratio around 4:1, present at age range of 20-50 years. The symptoms, features, and clinical findings associated with pulmonary eosinophilia include progressing dyspnea, myalgias, abdominal complaints, pruritic rash, rhinitis/sinusitis, distension of jugular venous, peripheral edema.
How is Pulmonary Eosinophilia Diagnosed?
Pulmonary eosinophilia is diagnosed pulmonary function test. Laboratory Studies- stool examination, leukocyte count, serologic testing. Imaging Studies- Chest CT scan and Chest radiography.
How is Pulmonary Eosinophilia Treated?
Pulmonary eosinophilia is treated through oxygen therapy, medical care- bronchodilator therapy, steroid therapy.
What is the Prognosis of Pulmonary Eosinophilia?
The prognosis of pulmonary eosinophilia is fair.
What is Pulmonary Langerhans Cell Histiocytosis?
Pulmonary langerhans cell histiocytosis is a rare syndrome of unidentified etiology occurring mostly in young smokers, characterized by focal collections of langerhans cells that cause scarring, alveolar damage, and airway obstruction.
What is the Pathology of Pulmonary Langerhans Cell Histiocytosis?
The pathology of pulmonary langerhans cell histiocytosis is:
-Etiology: The cause of pulmonary langerhans cell histiocytosis is believed to be exposure to cigarette smoke.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to pulmonary langerhans cell histiocytosis is not clearly understood.
-Histology: The histology associated with pulmonary langerhans cell histiocytosis shows poorly-defined nodules distributed in peribronchiolar location. Nodules are sclerosing containing langerhans cells and inflammatory cells. Also shows fibrosis with concomitant cystic change.
How does Pulmonary Langerhans Cell Histiocytosis Present?
Patients with pulmonary langerhans cell histiocytosis typically have no gender prevalence present at age range of 20 to 40 years. The symptoms, features, and clinical findings associated with pulmonary langerhans cell histiocytosis include cough, dyspnoea, weight loss, and fever. CT scan shows the presence of ill-defined stellate nodules and thin-walled cysts.
How is Pulmonary Langerhans Cell Histiocytosis Diagnosed?
Pulmonary langerhans cell histiocytosis is diagnosed through laboratory tests- CBC and ESR, Radiographic Tests- chest x-rays, CT scan. Biopsy may be useful.
How is Pulmonary Langerhans Cell Histiocytosis Treated?
Pulmonary langerhans cell histiocytosis is treated through smoking cessation, medical care- oxygen therapy, treatment for pulmonary infections, and bronchodilator therapy. Surgical therapy such as lung transplantation may be needed.
What is the Prognosis of Pulmonary Langerhans Cell Histiocytosis?
The prognosis of pulmonary Langerhans cell histiocytosis is fair and it is related to cessation of smoking.
What are Smoking-Related Interstitial Diseases that Cause Restrictive Lung Diseases?
Smoking-related interstitial diseases that cause restrictive lung diseases are as follows.
Examples of smoking-related interstitial diseases that cause restrictive lung diseases are:
- Desquamative interstitial pneumonia
- Respiratory bronchiolitis-associated interstitial lung disease
What is Desquamative Interstitial Pneumonia?
Desquamative interstitial pneumonia is a disease characterized by wide alveolar penetration by macrophages shadowed by fibrosis and interstitial inflammation.
What is the Pathology of Desquamative Interstitial Pneumonia?
The pathology of desquamative interstitial pneumonia is:
-Etiology: The cause of desquamative interstitial pneumonia is attributed to smoking.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to desquamative interstitial pneumonia are: Accumulation of macrophage at the respiratory bronchioles in retort to smoking, these provoke fibrosis and interstitial inflammation in a time-sensitive style.
-Histology: The histology associated with desquamative interstitial pneumonia shows the large accumulation of macrophages with plentiful cytoplasm comprising dusty brown color in the airspaces.
How does Desquamative Interstitial Pneumonia Present?
Patients with Desquamative Interstitial Pneumonia typically affect more males than females by a ratio of 2:1 present at age range of 40 to 50 years. The symptoms, features, and clinical findings associated with desquamative interstitial pneumonia include insidious commencement of dyspnea and dry cough over weeks or months, and clubbing of digits.
How is Desquamative Interstitial Pneumonia Diagnosed?
Desquamative interstitial pneumonia is diagnosed through laboratory studies- CBC count surge in eosinophil and neutrophil count. Imaging studies- Chest x-ray indicates reticulonodular infiltrates at lower lung regions.
How is Desquamative Interstitial Pneumonia Treated?
Desquamative interstitial pneumonia is treated through Medical treatment with steroid therapy and cessation of smoking.
What is the Prognosis of Desquamative Interstitial Pneumonia?
The prognosis of desquamative interstitial pneumonia is good with a brilliant response to treatment.
What is Respiratory Bronchiolitis-Associated Interstitial Lung Disease?
Respiratory bronchiolitis-associated interstitial lung disease is a syndrome of the small airway of well-organized lesions found in the lungs of those who smoke.
What is the Pathology of Respiratory Bronchiolitis-Associated Interstitial Lung Disease?
The pathology of respiratory bronchiolitis is:
-Etiology: The cause of bronchiolitis-associated interstitial lung disease is smoking, exposure to toxic fumes.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to bronchiolitis-associated interstitial lung disease are unknown.
-Histology: The histology associated with bronchiolitis-associated interstitial lung disease shows yellow to light brown and finely defined granular cytoplasmic pigments.
How does Respiratory Bronchiolitis-Associated Interstitial Lung Disease Present?
Patients with respiratory bronchiolitis-associated interstitial lung disease typically are from both genders in the age of between 30-60 years. The symptoms, features, and clinical findings associated with include respiratory bronchiolitis-associated interstitial lung disease is dyspnea, obstructive and restrictive pulmonary signs, cough, and tiredness.
How is Respiratory Bronchiolitis-Associated Interstitial Lung Disease Diagnosed?
Respiratory bronchiolitis-associated interstitial lung disease is diagnosed through imaging chest radiography and high-resolution computed topography, clinically using the presenting symptoms.
How is Respiratory Bronchiolitis-Associated Interstitial Lung Disease Treated?
Respiratory bronchiolitis-associated interstitial lung disease is treated mostly and effectively by encouraging cessation of smoking and also con current use of corticosteroids and immunosuppressives.
What is the Prognosis of Respiratory Bronchiolitis-Associated Interstitial Lung Disease?
The prognosis of respiratory bronchiolitis-associated interstitial lung disease is good. This is because those with the disease have a higher and prolonged survival rate.
What are Surfactant Dysfunction Disorders that Cause Restrictive Lung Diseases?
Surfactant dysfunction disorders that cause restrictive lung diseases are a group of conditions that result from anomalies in the surfactant function or composition.
Examples of surfactant dysfunction disorders that cause restrictive lung diseases are:
Disorders due to mutations in genes involved in surfactant secretion or trafficking.
What are Pulmonary Diseases of Vascular Origin?
Pulmonary diseases of vascular origin are diseases that occur in the bloodstream and the blood vessels are involved.
Examples of pulmonary diseases of vascular origin include:
- Pulmonary embolism
- Pulmonary hypertension
- Diffuse pulmonary hemorrhage syndromes
What is Pulmonary Embolism?
Pulmonary embolism is a condition in which one or more arteries become occluded by a blood clot.
What is Pulmonary Hypertension?
Pulmonary hypertension is systolic blood pressure in the pulmonary arterial circulation above 30mmhg where the mean pulmonary artery pressure is equal to or greater than 25 mm Hg at rest. There are five types:
- Group 1: Pulmonary arterial hypertension
- Group 2: Pulmonary hypertension due to left-sided heart failure
- Group 3: Pulmonary hypertension due to lung disease or hypoxia
- Group 4: Chronic thromboembolic pulmonary hypertension
- Group 5: Pulmonary hypertension with unknown causes
What are Diffuse Pulmonary Hemorrhage Syndromes?
Diffuse pulmonary hemorrhage syndromes are a collection of symptoms that occur due to the extensive bleeding of the lungs and they may include hemoptysis, hypoxemia with respiratory failure a drop in the hematocrit levels and the presence of diffuse pulmonary infiltrates.
Examples of diffuse pulmonary hemorrhage syndromes include:
- Goodpasture syndrome
- Idiopathic pulmonary hemosiderosis
- Polyangiitis with granulomatosis
What is Goodpasture Syndrome?
Goodpasture syndrome is inflammation of the glomerulus with or without pieces of evidence of pulmonary hemorrhage in the presence of antibodies known as the anti-glomerular basement antibodies caused by the body producing antibodies to fight the lung tissues.
What is the Pathology of Goodpasture Syndrome?
The pathology of goodpasture syndrome is:
-Etiology: The cause of goodpasture syndrome is corrosion and disturbance of the normal morphology of the tissue mostly caused by exposure to hydrocarbons, cocaine inhalation, smoking and lymphocyte depletion therapy.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to goodpasture syndrome occurs when there is the binding of the antibodies on the alpha 3 collagen causing pulmonary hemorrhage and glomerulonephritis.
-Histology: The histology associated with goodpasture shows crescentic glomerulonephritis which in turn changes to fibrotic glomerulosclerosis.
How does Goodpasture Syndrome Present?
Patients with goodpasture syndrome typically is higher in young males and older female.it occurs in two age ranges 20-30 years and 60-80 years respectively. symptoms, features, and clinical findings associated with goodpasture syndrome include dyspnea, fatigue, cough, hematuria, and hemoptysis.
How is Goodpasture Syndrome Diagnosed?
Goodpasture syndrome is diagnosed mostly through a biopsy of the kidneys since it gives accurate results. Another lab test done is the confirmation of the cytoplasmic antineutrophilic antibodies in the bloodstream.
How is Goodpasture Syndrome Treated?
Goodpasture syndrome is treated by the use of three guiding principles they involve; plasmapheresis which is the removal of the antibodies circulating in the system, use of immunosuppressive medication which stops the production of more antibodies, and getting rid of the provoking agents.
What is the Prognosis of Goodpasture Syndrome?
The prognosis of goodpasture syndrome is good since those who are diagnosed with, they have a 5-year survival rate once they are adhering to the treatments.
What is Idiopathic Pulmonary Hemosiderosis?
Idiopathic Pulmonary Hemosiderosis is a medical condition characterized by increased episodes of bleeding in the intra-alveolar which in turn leads to increased accumulation of iron in form of hemosiderin.
What is the Pathology of Idiopathic Pulmonary Hemosiderosis?
The pathology of idiopathic pulmonary hemosiderosis is:
-Etiology: The cause of idiopathic pulmonary hemosiderosis is Early childhood age, presence of antibodies Anti-glomerular basement membrane antibody, acquired or congenital cardiopulmonary abnormalities, infections e.g. pneumonia
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to idiopathic pulmonary hemosiderosis is divided into three categories. When there is the presence of circulating anti-GBM antibodies which leads to deposition of iron in the pulmonary system. When immune complexes are found in the pulmonary system example is in the Systemic Lupus erythematosus. The last category occurs with an unknown cause since none of the above causes are noted or found.
-Histology: The histology associated with idiopathic pulmonary hemosiderosis shows macrophages filled with hemosiderin, shedding, and hyperplasia of the alveolar epithelial cells.
How does Idiopathic Pulmonary Hemosiderosis Present?
Patients with idiopathic pulmonary hemosiderosis typically are of any age from the early neonatal ages to late adulthood. at age range of children 1-7 years. The symptoms, features, and clinical findings associated with idiopathic pulmonary hemosiderosis include Pallor and cyanosis due to increased blood loss, Tachypnea, Crackles, wheezing, and fever, in extreme cases there is growth retardation.
How is Idiopathic Pulmonary Hemosiderosis Diagnosed?
The diagnosis of Idiopathic Pulmonary Hemosiderosis is done through a series of blood workups imaging and at the time one can use lung biopsy. the clinical presentation of the patient also helps.
How is Idiopathic Pulmonary Hemosiderosis Treated?
this disease, Idiopathic Pulmonary Hemosiderosis is treated according to the symptoms that present and also as a long-term therapy. It includes oxygen supplementation, blood transfusion in case of shock mechanical ventilation, and immunosuppressive therapy. medical treatment options are the use of corticosteroids.
What is the Prognosis of Idiopathic Pulmonary Hemosiderosis?
The prognosis of idiopathic pulmonary hemosiderosis is fair with a mean survival rate of 3-5 years which is 86% survival rate.
What is Granulomatosis with Polyangiitis?
Granulomatosis with polyangiitis is also known as Wegener’s granulomatosis a condition that causes inflammation of the blood vessels falling under necrotizing vasculitis.
What is the Pathology of Granulomatosis with Polyangiitis?
The pathology of granulomatosis with polyangiitis is:
-Etiology: The cause of granulomatosis with polyangiitis presence of immunocomplexes circulating in the bloodstream.
-Genes involved: the presence of the HLA-DPB1 gene.
-Pathogenesis: The sequence of events that lead to granulomatosis with polyangiitis is a result of ANCA induced leukocyte activation in which the cytokines and the metabolites of lipids are produced this, in turn, leads to inflammation and formation of necrosis of the blood vessels wall.
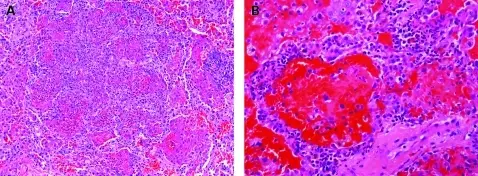
-Histology: The histology associated with granulomatosis with polyangiitis shows necrotic fibrinoid granulomas which are extensively infiltrated by neutrophils and mononuclear cells, giant cells of foreign bodies are also seen.
How does Granulomatosis with Polyangiitis Present?
Patients with granulomatosis with polyangiitis typically are male. The symptoms, features, and clinical findings associated with polyangiitis with Granulomatosis hearing loss and blood in urine sinus pain, joint pain, fever, cough.
How is Granulomatosis with Polyangiitis Diagnosed?
The granulomatosis with polyangiitis is diagnosed through physical examination followed by a couple of lab-works tom check for any antibodies in the circulating system.
How is Granulomatosis with Polyangiitis Treated?
Granulomatosis with polyangiitis is treated mostly depending on the severity of the disease. Medication includes steroids, immunosuppressors, antibiotics, and also antibodies. Other options are palliative care and hemodialysis if it affects the kidneys.
What is the Prognosis of Granulomatosis with Polyangiitis?
The prognosis of granulomatosis with polyangiitis is good with a survival rate of 80%.
What are Pulmonary Infections?
Pulmonary infections are diseases caused by the presence of infectious organisms in the pulmonary system.
Examples of pulmonary infections include:
- Community-acquired bacterial pneumonias
- Community-acquired viral pneumonia
- Health care-associated pneumonia
- Hospital-acquired pneumonia
- Aspiration pneumonia
- Lung abscess
- Chronic pneumonia
- Pneumonia in the immunocompromised
- Pulmonary disease in human immunodeficiency virus infection
| PULMONARY INFECTIONS | EXAMPLES |
| Community-Acquired Bacterial Pneumonias | Hemophilus Influenzae, Klebsiella Pneumoniae, Legionella Pneumophilia, Moraxella Catarrhalis, Mycoplasma Pneumoniae, Pseudomonas Aeruginosa, Staphylococcus Aureus, Streptococcus Pneumoniae. |
| Community-Acquired Viral Pneumonia | Human Metapneumovirus, Influenza Infections, Severe Acute Respiratory Syndrome |
| Health Care-Associated Pneumonia | Pneumonia associated with being hospitalized at least two days in recent past, presenting from a health care facility. The most common bacteria are MRSA and Pseudomonas. |
| Hospital-Acquired Pneumonia | Pneumonia obtained while hospitalized |
| Aspiration Pneumonia | Pneumonia due to aspirating gastric contents. Stroke, vomiting patients. |
| Lung Abscess | Local suppurative necrotizing process of lung tissue |
| Chronic Pneumonia | Blastomycosis, Coccidioidomycosis, Histoplasmosis |
| Pneumonia in the Immunocompromised | Typically, due to opportunistic infections. Cytomegalovirus, Pneumocystis jiroveci |
| Pulmonary Disease in Human Immunodeficiency Virus Infection | Typically, due to opportunistic infections. Cytomegalovirus, Pnemocystis jiroveci. |
Table showing pulmonary infections and the examples.
What are Pulmonary Tumors?
Pulmonary tumors are tumors that arise in the lungs.
Examples of pulmonary tumors include:
- Hamartomas of the lung
- Adenocarcinoma of the lung
- Adenosquamous carcinoma of the lung
- Large cell carcinoma of the lung
- Squamous cell carcinoma of the lung
- Small cell carcinoma of the lung
- Neuroendocrine tumors of the lung aka carcinoid tumors
What are Hamartomas of the Lung?
Hamartomas of the lung are noncancerous tumors that are formed after an abnormal mixture of normal cells and normal tissues e.g. cartilages, fat, muscle, or epithelium in the lungs.
What is the Pathology of Hamartomas of the Lung?
The pathology of hamartomas is:
-Etiology: The cause of hamartoma of the lung is not well defined but can be seen to be predisposed by other conditions.
-Genes involved: BMPR1A, SMAD4, PTEN, STK11.
-Pathogenesis: The sequence of events that lead to hamartoma of the lung is continuous abnormal replication of the normal tissue cells of the lungs.
-Histology: The histology associated with hamartoma of the lung shows a mixture of mature tissue of the mesenchyme which includes cartilages, adipose tissue, and smooth muscle tissues.
How does Hamartoma of the Lung Present?
Patients with hamartoma of the lung typically is higher in males than females with a mean age range of 20-77 years. The symptoms, features, and clinical findings associated with hamartoma of the lung include dyspnea, wheezing, coughing, productive cough, fever, and hemoptysis.
How is Hamartoma of the Lung Diagnosed?
The hamartoma of the lung is diagnosed radiologically using MR, CT-scan, chest x-ray.
How is Hamartomas of the Lung Treated?
The hamartoma of the lung is treated mostly by a surgical procedure that is known as the sleeve resection lobectomy.
What is the Prognosis of Hamartoma of the Lung?
The prognosis of hamartoma of the lung is good. This is because this tumor is slow-growing and even when it is fully grown it occurs in small sizes making the survival rate after resection good
What is Adenocarcinoma of the Lung?
Adenocarcinoma of the lung is cancer that arises from the mucosal glands of the bronchial and it is the most common type of non-small cell lung carcinomas.
What is the Pathology of Adenocarcinoma of the Lung?
The pathology of adenocarcinoma is:
-Etiology: The cause of adenocarcinoma is mostly noted to be the use of tobacco. Other causes are toxins exposure at home or in the workplaces.
-Genes involved: EGFR and KRAS are the main genes involved.
-Pathogenesis: The sequence of events that lead to adenocarcinoma exposure of the lung tissue to toxic substances, mutation of the genes occurs, which leads to increased growth of the abnormal cells.
-Histology: The histology associated with adenocarcinoma shows 5, patterns; acinar, papillary, micropapillary, solid, and lepidic patterns.
How does Adenocarcinoma Present?
Patients with adenocarcinoma are typically female but it also affects males who are non-smokers. It presents at an age range of 60-70 years. The symptoms, features, and clinical findings associated with adenocarcinoma include; Productive cough and dyspnea, Hemoptysis, Weight loss, and chest pain, and in a very rare case and the presence of paraneoplastic syndromes which include finger clubbing.
How is Adenocarcinoma Diagnosed?
Adenocarcinoma is diagnosed by use of a CT scan after a session of history taking and also a physical examination. Blood tests to confirm any presence of increased enzymes and CT scan, radiologic imaging using MRI shows well-defined lobulated air bronchograms with solid or acinar patterns.
How is Adenocarcinoma Treated?
The adenocarcinoma is treated depending on the location, size of the adenocarcinoma. surgery is the first option to remove the affected tissue. Chemotherapy and radiation therapy can also be used.
What is the Prognosis of Adenocarcinoma?
The prognosis of adenocarcinoma is dependent on the stage of the adenocarcinoma. Those in the early stage have a good prognosis with a survival rate of 85% and those with the advanced stage have a poor prognosis with a survival rate of 5%.
What is Adenosquamous Carcinoma of the Lung?
Adenosquamous carcinoma of the lung is a combination of both squamous cell carcinoma and adenocarcinoma of the lungs and falls under the category of non-small cell carcinoma.
What is the Pathology of Adenosquamous Carcinoma of the Lung?
The pathology of adenosquamous carcinoma is:
-Etiology: The cause of adenosquamous carcinoma is smoke from an either cigarette, car exhaust fumes asbestos and silica, and air pollution.
-Genes involved: EGFR and KRAS.
-Pathogenesis: The sequence of events that lead to adenosquamous carcinoma of the lungs is, carcinogenic binding to cell’s DNA and damage the cell, abnormal cell growth occur malignant pulmonary epithelial transformation, abnormal proliferation of the lung cells, to non-specific inflammatory changes leading to lesion formation.
-Histology: The histology associated with adenosquamous shows glandular elements to papillary lesions, also shows bronchioloalveolar growth pattern.
How does Adenosquamous Carcinoma of the Lung?
Patients with adenosquamous carcinoma typically have been marked increases female, linked to smoking, present at age mean range of 71 years. The symptoms, features, and clinical findings associated with adenosquamous include asymptomatic having nodules, hemoptysis, cough, or inadvertent weight loss.
How is Adenosquamous Carcinoma of the Lung Diagnosed?
The adenosquamous carcinoma is diagnosed specifically using the pathology presentation. However, other means of diagnosis are lung biopsy and also chest x-ray.
How is Adenosquamous Carcinoma of the Lung?
In treatment, adenocarcinoma is treated mostly using surgical resection of the affected lung or lobe(lobectomy) and lymph nodes (lymphadenectomy). Others are chemotherapy and radiotherapy.
What is the Prognosis of Adenosquamous Carcinoma of the Lung?
The prognosis of adenosquamous carcinoma is poor.
What Is Large Cell Carcinoma of the Lung?
Large cell carcinoma of the lung is lung cancer that is fast growing and occurs all around the lungs but mostly in the periphery due to the increased spreading rate.
What is the Pathology of Large Cell Carcinoma of the Lung?
The pathology of large cell carcinoma is:
-Etiology: The cause of large cell carcinoma is smoking (90%), exposure to carcinogens, and air pollution.
-Genes involved: TP53 and RB1.
-Pathogenesis: The sequence of events that lead to large cell carcinoma is neoplastic cellular growth.
-Histology: The histology associated with large cell carcinoma shows nests and sheets of large cells with large prominent nucleoli, abundant cytoplasm, and a vesicular nucleus.
How does Large Cell Carcinoma Present?
Patients with large cell carcinoma of the lung typically affect men who smoke with a percentage of 80 and they range between ages 50-70. The symptoms, features, and clinical findings associated with large cell carcinoma of include dyspnea, cough blood, weight loss due to loss of appetite fatigue.
How is Large Cell Carcinoma Diagnosed?
The Large Cell Carcinoma is diagnosed through history taking and physical examination, X-rays, CT scan, radiological imaging MRI and bone scans.
How is Large Cell Carcinoma Treated?
Large cell carcinoma is treated through surgery.
What is the Prognosis of Large Cell Carcinoma?
The prognosis of large cell carcinoma varies according to the stage the patient presents with. If the disease has not spread a lot the prognosis is good but if it has extended in stage the prognosis is poor.
What is Squamous Cell Carcinoma of the Lung?
Squamous cell carcinoma of the lung is a type of lung cancer seen in the central parts of the lungs or the main airway and falls under the category of non-small cell lung cancers.
What is the Pathology of Squamous Cell Carcinoma of the Lung?
The pathology of squamous cell carcinoma is:
-Etiology: The cause of squamous cell carcinoma of the lung is tobacco smoking is the main. Others include age, inactive smokers, or asbestos.
-Genes involved: TP53, GRM8, BAI3, ERBB4, KEAP1, KRAS.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma mutation of the squamous cell lining the airway were they thin and flatten. later keratinization occurs preventing the lining of the lung to perform its work normally.
-Histology: The histology associated with squamous cell carcinoma of the lung shows keratin pearls when imaging is done cytologically and nests of squamous cells.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically (determine and pick the gender that this affects (male, female, either male or female) present at an age range of (determine the age range of people typically affected). The symptoms, features, and clinical findings associated with squamous cell carcinoma Present include present hematemesis, wheezing, chronic cough, weight loss.
How is Squamous Cell Carcinoma Present Diagnosed?
Squamous cell carcinoma is diagnosed by physical examination, chest x-ray, complete blood count, CT scan, and MRI.
How is Squamous Cell Carcinoma Treated?
Squamous cell carcinoma is treated according to the stage presenting. for the early stages, resection is the best priority. In stages, 1B chemotherapy plus resection is advised. Stage 2 is treated by chemotherapy. Once it has advanced more resection is not possible hence chemotherapy and radiotherapy are advised.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of squamous cell carcinoma is poor. This is because by the time the symptoms present the disease would have advanced in a stage.
What is Small Cell Carcinoma of the Lung?
Small cell carcinoma of the lung is a poorly differentiated, rapidly growing cancer of the lungs, a neuroendocrine cancer.
What is the Pathology of Small Cell Carcinoma of the Lung?
The pathology of small cell carcinoma is:
-Etiology: The cause of small cell carcinoma is mostly tobacco smoking since all those who are diagnosed have a history of smoking.
-Genes involved: tumor suppressor genes P53, EGFR, and KRAS genes.
-Pathogenesis: The sequence of events that lead to small cell carcinoma of the lung include chromosomal changes causing dysregulation of tumor suppressor genes.
-Histology: The histology associated with small cell carcinoma shows a distinctive round shape with a blue color upon staining.
How does Small Cell Carcinoma Present?
Patients with small cell carcinoma typically present with shortness of breath, fatigue, weight loss cough, and bone pain. Occurs in those aged between 60-80 years old. It affects both genders but now mostly young women and equally to all races and ethnic groups.
How is Small Cell Carcinoma Diagnosed?
Small cell carcinoma is diagnosed through lung cancer screening, using the MRI which creates a clear image compared to chest x-ray or CT scans. for laboratory tests, a biopsy is taken for sampling to give clear results.
How is Small Cell Carcinoma Treated?
Small cell carcinoma is treated by pulmonary lobectomy to remove the affected lobe of the lung. Antineoplastics and alkylating agents may also be needed.
What is the Prognosis of Small Cell Carcinoma is?
The prognosis of is small cell carcinoma is poor.
What are Neuroendocrine Tumors of the Lung?
Neuroendocrine tumors of the lung aka carcinoid tumors are lung tumors that present with an aggressive form.
What is the Pathology of Neuroendocrine Tumors of the Lung?
The pathology of carcinoid tumors is:
-Etiology: The cause of carcinoid tumors is mostly by mutation of the oncogenes
-Genes involved: MEN1, RET, and MEN2 genes.
-Pathogenesis: The sequence of events that lead to carcinoid tumors is malignant proliferation.
-Histology: The histology associated with carcinoid tumors shows different patterns under the microscope. It shows solid, nodular, and insular cords, ribbons with anastomosing features, tubules and glands, poorly differentiated patterns, and lastly the mixed type.
How does Carcinoid Tumors Present?
Patients with carcinoid tumors typically present equally in women mostly that are older. The symptoms, features, and clinical findings associated with carcinoid tumors include hemoptysis and secondary infection, cough, atelectasis.
How are Carcinoid Tumors Diagnosed?
These Carcinoid Tumors are diagnosed by Octreoscan a special scan used to identify the carcinoid tumor by injecting a radioactive substance in the affected area X-ray and scans, biopsy, urine tests, and blood tests.
How is Carcinoid Tumor Treated?
The Carcinoid Tumor is treated by surgery if they are not too big. Octreotide medication is given to minimize the spread.
What is the Prognosis of Carcinoid Tumors?
The prognosis of carcinoid tumors is good with a survival rate of 5 years 78-95% and a 10-year survival rate of 77-90%.
| TUMORS | |
| Carcinomas | Adenocarcinoma, Adenosquamous Carcinoma, Carcinomas with other features, Carcinoid Tumor, Large Cell Carcinoma, Squamous Cell Carcinoma, Small Cell Carcinoma. |
| Hamartomas | Common benign lung tumor |
| Neuroendocrine Proliferations and Tumors | Carcinoid Tumors |
| Uncommon Pulmonary Tumors | Fibroma, Fibrosarcoma, Hemangioma, Inflammatory Myofibroblast Tumor, Leiomyoma, Leiomyosarcoma, Lipoma, Lymphangioleiomyomatosis.Metastatic Tumors: Lungs are the most common sites of metastatic neoplasms. |
What are Mediastinal Tumors?
Mediastinal tumors include growths that are found in the part of the chest that divides the lung into two separate organs.
Anterior mediastinal tumors and masses include:
- Lymphoma
- Metastatic carcinoma
- Parathyroid tumors
- Teratoma
- Thymoma
Middle mediastinal tumors and masses include:
- Bronchogenic cyst
- Lymphoma
- Pericardial cyst
Posterior mediastinal tumors and masses include:
- Bronchogenic cyst
- Gastroenteric hernia
- Lymphoma
- Metastatic tumor
- Neurogenic tumors (neurofibromas, schwannoma).
The table below shows the classification of mediastinal tumors and their examples.
| MEDIASTINAL TUMORS | |
| Anterior Mediastinal Tumors and Masses: | Lymphoma, Metastatic Carcinoma, Parathyroid Tumors, Teratoma, Thymoma. |
| Middle Mediastinal Tumors and Masses | Bronchogenic Cyst, Lymphoma, Pericardial Cyst |
| Posterior Mediastinal Tumors and Masses | Bronchogenic Cyst, Gastroenteric Hernia, Lymphoma, Metastatic Tumor, Neurogenic Tumors (Neurofibromas, Schwannoma). |
What are Pleural Lesions?
Pleural lesions are pathologic involvement of the pleura secondary to complications of other underlying illnesses.
Examples of pleural lesions include:
- Pleural effusions
- Pneumothorax
- Pleural tumors
What are Pleural Effusions?
Pleural effusions are an accumulation of excess fluid in the pleura cavity of the lungs.
Types of Pleural Effusion: Inflammatory Pleural Effusions, Noninflammatory Pleural Effusions.
What is the Pathology of Pleural Effusion?
The pathology of pleural effusion is the gross and microscopic study of the factors like heart failure that lead to the accumulation of fluid in the pleura and how to manage them.
-Etiology: The cause of the pleural effusion is mostly congestive heart disease, pulmonary embolism, and pneumonia.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pleural effusion are pleural inflammation altering the permeability of the membranes with impaired lymphatic drainage in the pleural space that leads to accumulation of excess fluid which can be in form of exudate or transudates.
-Histology: The histology associated with pleural effusion shows clear layers of simple cuboidal mesothelium cells found on top of connective tissues.
How does Pleural Effusion Present?
Patients with pleural effusion are typically male, female, and children with an age range of determining age. The symptoms, features, and clinical findings associated with pleural effusion include chest pain, shortness of breath, cyanosis, cough, edema, and orthopnea.
How is Pleural Effusion Diagnosed?
Pleural effusion is diagnosed mostly by use of CT scan since it clearly shows the area with the excess fluid. Other ways include a physical exam and history taking.
How is Pleural Effusion Treated?
A patient with pleural effusion is treated through a pleural tap, therapeutic thoracocentesis, tube thoracostomy, and pleurodesis to remove the excess fluid.
What is the Prognosis of Pleural Effusion?
The prognosis of pleural effusion is poor in the malignant form since it has a survival rate of only 4 months.
What is a Pneumothorax?
Pneumothorax is a condition characterized by the presence of air in the pleural cavity.
What is the Pathology of Pneumothorax?
The pathology of pneumothorax is:
-Etiology: The cause of pneumothorax is trauma to the chest wall cavity, certain disease progression
-Genes involved: FLCN gene mutation.
-Pathogenesis: The sequence of events that lead to pneumothorax is the entry of air in the pleural cavity that leads to increased pressure if the amount is too much to be reabsorbed to the lungs making it collapse. once it has collapsed the mediastinum is pulled to the unaffected area.
-Histology: The histology associated with pneumothorax shows collapsed air spaces.
How does Pneumothorax Present?
Patients with pneumothorax are typically men with a higher risk than females and although it can occur in all ages then peak age is 16-64 years and also relatively higher in the neonatal stages. The symptoms, features, and clinical findings associated with pneumothorax include dyspnea, cyanosis, chest pain, increase heart rate, and shortness of breath.
How is Pneumothorax Diagnosed?
Pneumothorax is diagnosed by use of a chest x-ray since it clearly shows the pathology but also a CT scan can be used together with history taking and also physical exam.
How is Pneumothorax Treated?
a patient with pneumothorax is treated by preventing or managing the underlying cause of increased pleural pressure, getting rid of excess air through chest tube insertion, and later by preventing recurrence of the cause.
What is the Prognosis of Pneumothorax?
The prognosis of pneumothorax is dependent on the extent of the pressure.it has a good prognosis if the pressure is minimal and a poor prognosis if the pressure is a lot.
What are Pleural Tumors?
Pleural tumors are benign or malignant growths that arise from the pleural space a cavity between the lungs and the chest wall.
Examples of pleural tumors include:
- Solitary fibrous tumor
- Malignant mesothelioma
What is a Solitary Fibrous Tumor?
Solitary fibrous tumor is a rare combination of growth of the soft tissue that can occur anywhere in the body.
What is the Pathology of Solitary Fibrous Tumor?
The pathology of solitary fibrous tumor is:
-Etiology: The cause of solitary fibrous tumors is unknown.
-Genes involved: NGFI-A binding protein 2 and STAT6.
-Pathogenesis: The sequence of events that lead to solitary fibrous tumor occurs as a result of hematogenous spread to the lung from the place of origin.
-Histology: The histology associated with solitary fibrous tumors shows an Increased mitotic rate than the normal, necrotic tissues are observed, ovoid spindle cells with indistinct cell borders arranged in a disorganized manner, and the nuclei have overwrapped on each other evidence of increased multiplication and disorganization.
How does Solitary Fibrous Tumors Present?
Patients with solitary fibrous tumors typically are both men 42% and women58% with the same rate of being affected with a median age arrange of 52 years. The symptoms, features, and clinical findings associated with solitary fibrous tumors include a large painless mass on the affected area.
How are Solitary Fibrous Tumors Diagnosed?
Mostly Solitary Fibrous Tumors are diagnosed through x-ray, Computerized tomography (CT scan), Magnetic resonance imaging (MRI), positron emission tomography (PET), a biopsy of part of the affected area.
How are Solitary Fibrous Tumors Treated?
The solitary fibrous tumors are treated mostly only through the resection of the affected part of the lung. If the tumor cannot be removed one is recommended to attend a couple of sessions of radiotherapy. Use of medication that targets only the affected area is also used but in rare cases.
What is the Prognosis of Solitary Fibrous Tumors?
The prognosis of solitary fibrous tumors is fair for the malignant case but the benign case is good. This is because the patients have a median survival rate ranging from 1-5 years old.
What is Malignant Mesothelioma?
Malignant mesothelioma is a cancer of the lung mesothelium associated with the inhalation of asbestos and is rare.
What is the Pathology of Malignant Mesothelioma?
The pathology of malignant mesothelioma is:
-Etiology: The cause of malignant mesothelioma is prolonged inhalation of asbestos.
-Genes involved: mutation of BAP1 gene.
-Pathogenesis: The sequence of events that lead to malignant mesothelioma is followed by prolonged accumulation of asbestos bodies through inhalation or being close to those who have been exposed.
-Histology: The histology associated with malignant mesothelioma shows the presence of asbestos bodies.
How does Malignant Mesothelioma Present?
Patients with malignant mesothelioma typically are mostly male with a present age range of 25-94 years. The symptoms, features, and clinical findings associated with malignant mesothelioma include remaining asymptomatic for some period but due to ling term fibrosis they present with dyspnea, pulmonary hypertension and other cancers of the lung may arise
How is Malignant Mesothelioma Diagnosed?
Diagnosis of malignant mesothelioma is done through imaging the use of an MRI is the most common imaging done together with a CT scan.
How is Malignant Mesothelioma Treated?
The treatment of malignant mesothelioma is done through surgery only when it is noted in the early stages but in advanced stages, the doctor recommends chemotherapy and radiotherapy. medical treatment options include the use of immunosuppressors and targeted therapy.
What is the Prognosis of Malignant Mesothelioma?
The prognosis of malignant mesothelioma is dependent on the stage of the disease. It has a poor prognosis if-then disease has advanced in stage with a survival rate of less than one year.