Red blood cell pathology is the anomalies associated with the structure, volume, and alterations of the red blood cells normal functioning, oxygen transportation.
Red blood cell pathology includes:
- Anemias
- Bleeding disorders
- Polycythemia
- Transfusion complications
What is Anemia?
Anemia is a reduction in circulating red blood cells below normal limits. Anemia is clinically defined as the reduction hemoglobin (Hb) concentration of the blood, measured by the hematocrit.
Anemias are subdivided into the following categories:
- Anemia of blood loss
- Anemias of diminished erythropoiesis
- Hemolytic anemia
What are Anemias due to Blood Loss?
Anemias due to blood loss are the reductions of circulating hemoglobin due to hemorrhagic.
Examples of anemias due to blood loss include:
- Anemia due to acute blood loss
- Anemia due to chronic blood loss
What is Anemia due to Acute blood loss?
Anemia due to acute blood loss is the reduction of circulating hemoglobin due to hemorrhagic resulting from trauma.
What is the Pathology of Anemia Due to Acute Blood Loss?
The pathology of anemia due to:
-Etiology: The cause of anemia due to acute blood loss is acute trauma.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anemia due to acute blood loss trauma causes hemorrhagic, leading to low hemoglobin level in hematocrit. Which eventually produce the signs and symptoms. The oxygenation reduction to the renal juxtaglomerular cells triggers increased production of erythropoietin.
-Morphology: The morphology associated with anemia due to acute blood loss shows cyanosis of tissues.
-Histology: The histology associated with anemia due to acute blood loss shows reduced red cells count, leukocytosis.
How does Anemia Due to Acute Blood Loss Present?
Patients with anemia due to acute blood loss typically vary depending on the underlying cause. The symptoms, features, and clinical findings associated with anemia due to acute blood loss include pallor, fatigue, and signs of hypovolemia.
How is Anemia Due to Acute Blood Loss Diagnosed?
Anemia due to acute blood loss is diagnosed through clinical presentations, laboratory studies, full hemogram (HB level decreased). Imaging studies to certify internal bleeding or endoscopy may be helpful.
How is Anemia Due to Acute Blood Loss Treated?
Anemia due to acute blood loss is treated by treating the underlying cause through medical care including antifibrinolytic (tranexamic acid), vasopressors, histamine (H2) antagonists, and glucocorticosteroids. Fluid replacement therapy, blood and blood products transfusion may be useful. Surgical intervention to stop active bleeding may be necessary.
What is the Prognosis of Anemia Due to Acute Blood Loss?
The prognosis of anemia due to acute blood loss is good with effective blood transfusion and cessation of bleeding.
What is Anemia due to Chronic blood loss?
Anemia due to chronic blood loss is when the rate of hemorrhage depletes the iron reserves, and bleeding surpasses regenerative capability of the marrow.
What is the Pathology of Anemia Due to Chronic Blood Loss?
The pathology of anemia due to chronic blood loss is:
-Etiology: The cause of anemia due to chronic blood loss is prolonged hemorrhage internal/external, vitamin B-12 deficiency, and folate deficiency.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anemia due to chronic blood loss is the result of hemorrhage that exceed the iron reserves and regenerative capacity of the marrow leading to reduced blood volume and reduced hemoglobin level. When hemorrhage exceeds the capacity of the bone marrow regenerative and also causes the depletion of iron reserves with feature of prolonged bleeding more than two weeks.
-Morphology: The morphology associated with anemia due to chronic blood loss shows tissue pallor.
-Histology: The histology associated with anemia due to chronic blood loss shows reduced hematocrit level, (reduced red cells count), leukocytosis.
How does Anemia Due to Chronic Blood Loss Present?
Patients with anemia due to chronic blood loss typically vary depending on the underlying cause among males and females present at an age range of any age. The symptoms, features, and clinical findings associated with anemia due to chronic blood loss include signs of hypovolemia.
How is Anemia Due to Chronic Blood Loss Diagnosed?
Anemia due to chronic blood loss is diagnosed through the clinical presentation; Laboratory studies full hemogram (reduced below normal Hb levels). Imaging studies to certify internal bleedings- radiological studies and endoscopy.
How is Anemia Due to Chronic Blood Loss Treated?
Anemia due to chronic blood loss is treated by treating the underlying cause through medical care- antifibrinolytic therapy, vasopressors, histamine (H2) antagonists, and glucocorticosteroids. Fluid replacement therapy, blood and blood products transfusion. Surgical intervention to stop active bleeding.
What is the Prognosis of Anemia Due to Chronic Blood Loss?
The prognosis of anemia due to chronic blood loss is fair, depending on underlying medical, severity of the blood loss, associated with complications such as tenacious tissue hypoxia.
What are Anemias of Diminished Erythropoiesis?
Anemias of diminished erythropoiesis are reduction of the blood volume, hematocrit level, or reduced hemoglobin level due to inadequate production of the red cells and incapacity of the marrow regeneration.
Examples of anemias of diminished erythropoiesis include:
- Aplastic anemia
- Anemia of chronic disease
- Anemia of folate deficiency
- Iron deficiency anemia
- Megaloblastic anemia
- Pure red cell aplasia
What is Aplastic Anemia?
Aplastic anemia is a disorder of marrow failure related to marrow hypoplasia and pancytopenia.
What is the Pathology of Aplastic Anemia?
The pathology of aplastic anemia is:
-Etiology: The cause of aplastic anemia is acquired or idiopathic.
-Genes involved: RMRP gene, TERC, and TERT genes
-Pathogenesis: The sequence of events that lead to aplastic anemia is not fully understood and is believed to result commonly from suppression of stem cell role through the activated T cells.
-Morphology: Possible rashes.
-Histology: The histology associated with aplastic anemia shows devoid of hematopoietic cells.
How does Aplastic Anemia Present?
Patients with aplastic anemia typically either gender present at an age range of any age. The symptoms, features, and clinical findings associated with aplastic anemia include weakness, pallor, dyspnea, petechiae, ecchymoses, chills, and fever.
How is Aplastic Anemia Diagnosed?
Aplastic anemia is diagnosed through the clinical presentation, laboratory studies- scrutiny of bone marrow biopsy and peripheral blood indicates hypocellular.
How is Aplastic Anemia Treated?
Aplastic anemia is treated through supportive care, blood transfusion, hematopoietic cell transplantation (HCT), or immunosuppressive therapy.
What is the Prognosis of Aplastic Anemia?
The prognosis of aplastic anemia is fair. It is unpredictable with spontaneous remission in idiopathic causes.
What is Anemia of Chronic Disease?
Anemia of chronic disease is the disorder of the red cell linked to chronic diseases, mostly among hospitalized patient.
What is the Pathology of Anemia of Chronic Disease?
The pathology of anemia of chronic disease is:
-Etiology: The cause of anemia of chronic disease is depends on the underlying disease which may include chronic immune disorders, chronic microbial infections, and neoplasms.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anemia of chronic disease may involve the decrease in renal erythropoietin generation is instigated by the act of tumor necrosis factor (TNF), interleukin-1, and interferon-γ, secretion triggered by the underlying neoplastic or chronic inflammatory disease. Cytokines also arouse hepcidin synthesis in the liver, inhibiting iron release from the storage reserves.
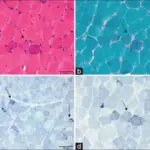
-Morphology: The morphology associated with anemia of chronic disease shows normocytic and normochromic or hypochromic and microcytic red cells.
-Histology: The histology associated with anemia of chronic disease shows incidence of nucleated RBC precursors and/or immature myeloid cells.
How does Anemia of Chronic Disease Present?
Patients with anemia of chronic disease typically more common in females than males resent at an age range of 20 to 45 years. The symptoms, features, and clinical findings associated with anemia of chronic disease include; the symptom of the underlying condition.
How is Anemia of Chronic Disease Diagnosed?
Anemia of chronic disease is diagnosed through the clinical presentation, laboratory studies- RBC indices, Full hemogram, reduced reticulocyte count, peripheral blood smear.
How is Anemia of Chronic Disease Treated?
Anemia of chronic disease is treated through the management of the underlying disease. Medical care such as erythropoiesis-stimulating agents, or oral iron products may be helpful.
What is the Prognosis of Anemia of Chronic Disease?
The prognosis of anemia of chronic disease is good. Improve with the administration of erythropoietin and treatment of the underlying condition.
What is Anemia of Folate Deficiency?
Anemia of folate deficiency is red cells anomaly resulting from deficit of folate also known as vitamin B9.
What is the Pathology of Anemia of Folate Deficiency?
The pathology of anemia of folate deficiency is:
-Etiology: The cause of anemia of folate deficiency is decreased intake, increased requirements, and impaired use of folate.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anemia of folate deficiency is decreased folate intake either through nutritionally insufficient or diminish intestinal uptake, augmented folate requirement in conditions such as pregnancy and disseminated cancer. Impaired use of folate leads deficiency of folic acid necessary in the erythropoiesis process producing the features of megaloblastic anemia.
-Morphology: The morphology associated with anemia of folate deficiency shows megaloblastic red cells.
-Histology: The histology associated with anemia of folate deficiency shows enlarged RBCs and multi-lobated neutrophils.
How does Anemia of Folate Deficiency Present?
Patients with anemia of folate deficiency typically common in females than males present at an age range of 40 years. The symptoms, features, and clinical findings associated with anemia of folate deficiency include palpitations, lethargy, fatigue, feeling faint, pallor, weight loss, and headaches.
How is Anemia of Folate Deficiency Diagnosed?
Anemia of folate deficiency is diagnosed through medical presentation, laboratory studies- reduced folate levels in the serum, and increased serum homocysteine levels.
How is Anemia of Folate Deficiency Treated?
Anemia of folate deficiency is treated through folate therapy.
What is the Prognosis of Anemia of Folate Deficiency?
The prognosis of anemia of folate deficiency is good with the management of folic acid administration.
What is Iron Deficiency Anemia?
Iron deficiency anemia is condition in which the there is severe enough to diminish erythropoiesis and cause the development of anemia.
What is the Pathology of Iron Deficiency Anemia?
The pathology of iron deficiency anemia is:
-Etiology: The cause of iron deficiency anemia is dietary factors, bleeding, hemoglobinuria, pulmonary hemosiderosis, and hemosiderinuria.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to iron deficiency anemia is as a result of either dietary lack, impaired absorption, increased requirement, or chronic blood loss causing depletion of iron-containing enzymes. This persuades a hypochromic microcytic anemia. At initial stage iron reserve may maintain typical hematocrit and hemoglobin levels. Advanced depletion lowers transferrin saturation and serum iron levels, without causing anemia. Anemia occurs after complete depletion of the reserves.
-Morphology: The morphology associated with iron deficiency anemia shows microcytic and hypochromic red cells.
-Histology: The histology associated with iron deficiency anemia shows slight to modest upsurge in erythroid normoblasts.
How does Iron Deficiency Anemia Present?
Patients with iron deficiency anemia typically higher in females present at an age range of below 10 years and during the child bearing age. The symptoms, features, and clinical findings associated with iron deficiency anemia include palpitations, lethargy, fatigue, feeling faint, pallor, weight loss, reduced capillary refill, and headaches.
How is Iron Deficiency Anemia Diagnosed?
Iron deficiency anemia is diagnosed clinical presentation, laboratory studies such as CBC count shows microcytic and hypochromic erythropoiesis, elevated platelet count. Peripheral smear, low serum ferritin and iron. Hemoglobin (A2) studies, reticulocyte hemoglobin content, and bone marrow aspiration.
How is Iron Deficiency Anemia Treated?
Iron deficiency anemia is treated through medical care which include parenteral/oral ferrous iron therapy, dietary measures and activity restrictions.
What is the Prognosis of Iron Deficiency Anemia?
The prognosis of iron deficiency anemia is good as it is an easily managed illness with an exceptional outcome.
What is Megaloblastic Anemia?
Megaloblastic anemia is the reduction of hematocrit and hemoglobin levels as a result of deficiencies of vital nutrients necessary for red cell formation. Megaloblastic anemia may be due to pernicious anemia, vitamin B12 deficiency. It may also be due to vitamin B9 deficiency.
What is the Pathology of Megaloblastic Anemia?
The pathology of megaloblastic anemia is:
-Etiology: The cause of megaloblastic anaemia is Pernicious anaemia, bacterial overgrowth in the intestine, folic acid deficiency, and certain drugs.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to megaloblastic anemia may be due to deficiency of vitamin B12 causes pernicious anemia, while deficiency of folic acid leads to folate deficiency anemia (featured by defective DNA synthesis), and iron deficiency anemias characterized by impaired heme production.
-Morphology: The morphology associated with megaloblastic anemia shows red cells are macrocytic and oval.
-Histology: The histology associated with megaloblastic anemia shows a six-lobed hyper nucleus segmented neutrophil.
How does Megaloblastic Anemia Present?
Patients with megaloblastic anemia are typically higher in females than males present at the age range of 40 years. The symptoms, features, and clinical findings associated with megaloblastic anemia include abdominal discomfort, hyperpigmentation, lethargy, fatigue, faintness, pallor, weight loss, abnormal gait, loss of balance, and headaches.
How is Megaloblastic Anemia Diagnosed?
Megaloblastic anemia is diagnosed through the clinical presentation, laboratory studies- red blood cell (RBC) indices, complete blood count, peripheral blood smear reticulocyte, count, Iron and ferritin level, serum folate, and bone marrow aspiration.
How is Megaloblastic Anemia Treated?
Megaloblastic anemia is treated through medical care such as cobalamin therapy, folate therapy, management of other linked conditions. Dietary measures and consultations may be helpful.
What is the Prognosis of Megaloblastic Anemia?
The prognosis of megaloblastic anemia is good when the etiology is identified and managed appropriately.
What is Pernicious Anemia?
Pernicious anemia is a specific form of megaloblastic anemia related to the deficiency of the vitamin B12.
What is the Pathology of Pernicious Anemia?
The pathology of pernicious anemia is:
-Etiology: The cause of pernicious anemia is insufficient dietary intake, intestinal bacterial overgrowth, ileal mucosa disorders, disarrays of cobalamin plasma transport, intrinsic factor deficiency, tapeworm infestation, pregnancy, and hyperthyroidism
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pernicious anemia allegedly results from immunologically mediated. Failure of intrinsic factor production that leads to vitamin B12 deficiency triggers a specific type of megaloblastic anemia.
-Morphology: The morphology associated with pernicious anemia shows atrophic glossitis tongue.
-Histology: The histology associated with pernicious anemia shows atrophy of the fundic glands, megaloblastic cells.
How does Pernicious Anemia Present?
Patients with pernicious anemia typically have female predominance present at an age range of 50 to 80 years. The symptoms, features, and clinical findings associated with pernicious anemia include neurologic symptoms, irritability, memory loss, personality changes, retention, impaired micturition gastrointestinal symptoms, smooth tongue, palpable splenic tip, and retinal hemorrhages.
How is Pernicious Anemia Diagnosed?
Pernicious anemia is diagnosed clinical presentation, laboratory studies such as peripheral blood usually indicates macrocytic anemia, elevated indirect bilirubin level, increased serum lactate dehydrogenase concentration. Serum folic acid, and cobalamin levels. Intrinsic factor antibodies type 1 and 2. Schilling test.
How is Pernicious Anemia Treated?
Pernicious anemia is treated through medical care such as vitamin B12 therapy, blood transfusion, activity restriction and dietary measures.
What is the Prognosis of Pernicious Anemia?
The prognosis of pernicious anemia is fair.
What is Pure Red Cell Aplasia?
Pure red cell aplasia is an erratic type of marrow failure featured by a marked marrow erythroid elements hypoplasia in the setting of typical granulopoiesis and thrombopoiesis
What is the Pathology of Pure Red Cell Aplasia?
The pathology of pure red cell aplasia is:
-Etiology: The cause of pure red cell aplasia is idiopathic, secondarily to infections, neoplasms, drug exposures, or autoimmune disorders.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pure red cell aplasia due to a discerning injury, often immunologic, affecting the initial phase of erythrocyte maturation.
-Morphology: The morphology associated with pure red cell aplasia shows erythrocytosis.
-Histology: The histology associated with pure red cell aplasia shows normocytic cells.
How does Pure Red Cell Aplasia Present?
Patients with pure red cell aplasia typically have no gender prevalence present at an age range of childhood and adulthood. The symptoms, features, and clinical findings associated with pure red cell aplasia include uncompensated anemia, bruising, enlarged parotid glands, and altered growth.
How is Pure Red Cell Aplasia Diagnosed?
Pure red cell aplasia is diagnosed through laboratory studies-CBC count, reticulocyte count, (WBC) differential analysis of WBCs and bone marrow histology. Imaging studies- Positron emission tomography, CT scans detect thymomas.
How is Pure Red Cell Aplasia Treated?
Pure red cell aplasia is treated through transfusion, treating the underlying condition, and surgical care.
What is the Prognosis of Pure Red Cell Aplasia?
The prognosis of pure red cell aplasia is fair.
What is Hemolytic Anemia?
Hemolytic anemia is bone marrow disorder in which its activity cannot compensate for the erythrocyte loss leading to anemia.
Examples of conditions that may cause hemolytic anemia include:
- Hereditary spherocytosis
- Glucose-6-phosphate dehydrogenase deficiency
- Hemolytic anemia due to red blood cell trauma
- Immunohemolytic anemia
- Paroxysmal nocturnal hemoglobinuria
- Sickle cell disease
- Thalassemia syndromes
What is Hereditary Spherocytosis?
Hereditary spherocytosis is a ailment is instigated by intrinsic defects of the red cell membrane rendering them less deformable, spheroid, and defenseless to splenic sequestration and destruction.
What is the Pathology of Hereditary Spherocytosis?
The pathology of hereditary spherocytosis is:
-Etiology: The cause of hereditary spherocytosis is the mutations leading to defects in red blood cell (RBC). Hereditary spherocytosis is caused by diverse mutations affecting ankyrin, band 3, spectrin, or band 4.2, the proteins involved in the tethering interactions.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to hereditary spherocytosis erythrocyte membrane proteins intrinsic defects consequence the RBC cytoskeleton unsteadiness. Forfeiture of erythrocyte surface area chiefs the production of spherocytes, which are discarded quickly from the circulation by the action of the spleen. Hemolysis confined to the spleen triggers splenomegaly.
-Morphology: The morphology associated with hereditary spherocytosis shows trivial, hyperchromic red cells without the normal central zone of pallor.
-Histology: The histology associated with hereditary spherocytosis shows anisocytosis
How does Hereditary Spherocytosis Present?
Patients with hereditary spherocytosis typically higher in females than males present at an age range of any age. The symptoms, features, and clinical findings associated with hereditary spherocytosis include splenomegaly, jaundice icterus, and darker urine.
How is Hereditary Spherocytosis Diagnosed?
Hereditary spherocytosis is diagnosed through clinical presentation, laboratory studies like MCV, complete blood cell count, reticulocyte count, peripheral blood smear, Coombs testing, and fractionated bilirubin.
How is Hereditary Spherocytosis Treated?
Hereditary spherocytosis is treated through medical care folic acid therapy, and possibly a splenectomy.
What is the Prognosis of Hereditary Spherocytosis?
The prognosis of hereditary spherocytosis is fair.
What is Glucose-6-Phosphate Dehydrogenase Deficiency?
Glucose-6-phosphate dehydrogenase deficiency is a genetic condition subsequent from a structural flaw in G6PD, enzyme that is predominantly significant for the endurance of RBCs and their aptitude to respond to oxidative stress.
What is the Pathology of Glucose-6-Phosphate Dehydrogenase Deficiency?
The pathology of glucose-6-phosphate dehydrogenase deficiency is:
-Etiology: The cause of glucose-6-phosphate dehydrogenase deficiency is G6PD gene mutations.
-Genes involved: G6PD gene.
-Pathogenesis: The sequence of events that lead to glucose-6-phosphate dehydrogenase deficiency is inability to convert NADP to NADPH and oxidizing glucose-6-phosphate.
-Morphology: The morphology associated with glucose-6-phosphate dehydrogenase deficiency shows
-Histology: The histology associated with glucose-6-phosphate dehydrogenase deficiency shows Heinz bodies
How does Glucose-6-Phosphate Dehydrogenase Deficiency Present?
Patients with glucose-6-phosphate dehydrogenase deficiency typically higher in males present at an age range of any age. The symptoms, features, and clinical findings associated with glucose-6-phosphate dehydrogenase deficiency include Neonatal jaundice, intravascular hemolysis and chronic hemolytic anemia.
How is Glucose-6-Phosphate Dehydrogenase Deficiency Diagnosed?
Glucose-6-phosphate dehydrogenase deficiency is diagnosed through laboratory test for G6PD deficiency which includes Beutler test and a quantitative assay of GPD activity, other lab works include CBC count, serum haptoglobin level, urinalysis for hematuria, bilirubin level, lactate dehydrogenase (LDH) level, and peripheral blood smear.
How is Glucose-6-Phosphate Dehydrogenase Deficiency Treated?
Glucose-6-phosphate dehydrogenase deficiency is treated through counselling to avoid chemicals and drugs that may cause oxidant stress.
What is the Prognosis of Glucose-6-Phosphate Dehydrogenase Deficiency?
The prognosis of glucose-6-phosphate dehydrogenase deficiency is fair as most are asymptomatic.
What is Hemolytic Anemia Due to Red Blood Cell Trauma?
Hemolytic anemia due to red blood cell trauma is disorder of the red cells caused by circumstances involving trauma, cardiac valve prostheses, or narrowing or obstruction.
What is the Pathology of Anemia Due to Red Blood Cell Trauma?
The pathology of anemia due to red blood cell trauma is:
-Etiology: The cause of anemia due to red blood cell trauma is narrowing of vessels due to fibrin deposition, other conditions such as malignant hypertension, thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndrome (HUS), disseminated cancer.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anemia due to red blood cell trauma; When red cells are squeeze through abnormally narrowing of vessels due to fibrin deposition causing microangiopathic hemolytic anemia. Hemolysis as a results of shear stresses due to turbulent blood flow and irregular pressure gradients.
-Morphology: The morphology associated with anemia due to red blood cell trauma shows vessels narrowing, fibrin deposit on blood vessels.
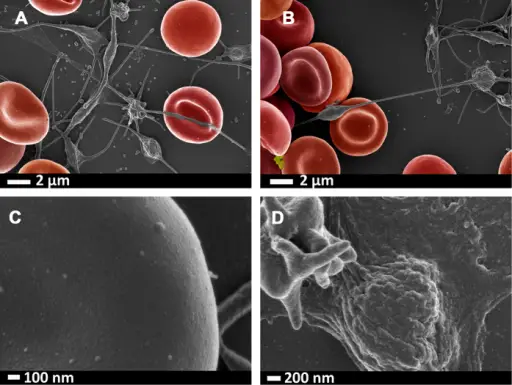
-Histology: The histology associated with anemia due to red blood cell trauma shows burr cells, helmet cells, and triangle cells.
How does Anemia Due to Red Blood Cell Trauma Present?
Patients with anemia due to red blood cell trauma typically common in females than males present at an age range of childhood and adulthood. The symptoms, features, and clinical findings associated with anemia due to red blood cell trauma include tachycardia, abdominal pain, dyspnea, dark urine angina, weakness.
How is Anemia Due to Red Blood Cell Trauma Diagnosed?
Anemia due to red blood cell trauma is diagnosed through medical presentation, laboratory studies-CBC count, peripheral blood smear, indirect bilirubin, LDH levels, and serum haptoglobin.
How is Anemia Due to Red Blood Cell Trauma Treated?
Anemia due to red blood cell trauma is treated through managing underlying conditions, medical care-iron therapy, erythropoietin therapy, and transfusion.
What is the Prognosis of Anemia Due to Red Blood Cell Trauma?
The prognosis of anemia due to red blood cell trauma is fair depending on the management of the underlying cause.
What is Immunohemolytic Anemia?
Immunohemolytic anemia is hemolytic anemia caused by extracorpuscular mechanisms.
What is the Pathology of Immunohemolytic Anemia?
The pathology of immunohemolytic anemia is: an anomaly in which the body’s immune system halts red blood cells formation and causes them to clump together.
-Etiology: The cause of immunohemolytic anemia is drugs, toxins, infections, transfusion, and certain cancers.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to immunohemolytic anemia is not well understood.
-Morphology: Rashes.
-Histology: Acanthocytes.
How does Immunohemolytic Anemia Present?
Patients with immunohemolytic anemia typically have no gender prevalence present at an age range of any age.The symptoms, features, and clinical findings associated with immunohemolytic anemia include jaundice, pallor, weakness, chest pain, tachycardia, and dark urine.
How is Immunohemolytic Anemia Diagnosed?
Immunohemolytic anemia is diagnosed through laboratory studies including Coombs antiglobulin test to detect antibodies and complement on red cells.
How is Immunohemolytic Anemia Treated?
Immunohemolytic anemia is treated through medical care including corticosteroid therapy, blood transfusions, blood and marrow stem cell transplants, and lifestyle modification.
What is the Prognosis of Immunohemolytic Anemia?
The prognosis of immunohemolytic anemia is fair depending on the underlying causes.
What is Paroxysmal Nocturnal Hemoglobinuria?
Paroxysmal nocturnal hemoglobinuria is a disorder resulting from acquired mutations in phosphatidylinositol glycan A (PIGA).
What is the Pathology of Paroxysmal Nocturnal Hemoglobinuria?
The pathology of paroxysmal nocturnal hemoglobinuria is:
-Etiology: The cause of paroxysmal nocturnal hemoglobinuria is gene PIGA mutation
-Genes involved: PIGA
-Pathogenesis: The sequence of events that lead to paroxysmal nocturnal hemoglobinuria result from somatic mutations occurring in pluripotent stem cells, with all its clonal progeny lacking in proteins attached to the cell membrane via GPI. Mutations in phosphatidylinositol glycan A (PIGA) vital for synthesizing the phospholipid glycosylphosphatidylinositol (GPI) anchor.
-Morphology: Rashes.
-Histology: Abnormal red blood cells.
How does Paroxysmal Nocturnal Hemoglobinuria Present?
Patients with paroxysmal nocturnal hemoglobinuria typically have no gender prevalence present at age range of childhood and adulthood. The symptoms, features, and clinical findings associated with paroxysmal nocturnal hemoglobinuria include esophageal spasms, raised painful red nodules in the skin, headache, and abdominal pain.
How is Paroxysmal Nocturnal Hemoglobinuria Diagnosed?
Paroxysmal nocturnal hemoglobinuria is diagnosed through laboratory studies- Flow cytometry to detect CD59, a glycoprotein, and CD55. Acidified serum lysis and Ham test, immunotyping, complement lysis sensitivity test, sucrose lysis test. Serum lactate dehydrogenase levels may also be useful.
How is Paroxysmal Nocturnal Hemoglobinuria Treated?
Paroxysmal nocturnal hemoglobinuria is treated through monoclonal antibodies therapy (eculizumab, ravulizumab), corticosteroids therapy, managing underlying causes, and bone marrow transplant.
What is the Prognosis of Paroxysmal Nocturnal Hemoglobinuria?
The prognosis of paroxysmal nocturnal hemoglobinuria is fair with proper management.
What is Sickle Cell Disease?
Sickle cell disease is an inborn hemoglobinopathy, a disease characterized by the production of defective hemoglobin.
What is the Pathology of Sickle Cell Disease?
The pathology of sickle cell disease is:
-Etiology: The cause of sickle cell disease is a point alteration at the 6th position of the β-globin chain causing the switch of a valine residue for a glutamic acid residue.
-Genes involved: β-globin gene.
-Pathogenesis: The sequence of events that lead to sickle cell disease due to deoxygenated sickle hemoglobin molecules undergoing aggregation and polymerization. Prolonged deoxygenation produces a slanted sickle or holly-leaf shape.
-Morphology: The morphology associated with sickle cell disease shows small vessel stasis and thrombosis.
-Histology: The histology associated with sickle cell disease shows sickle cells, anisocytosis, and poikilocytosis.
How does Sickle Cell Disease Present?
Patients with sickle cell disease typically have no sex prevalence present at age range of. 2.5 years. The symptoms, features, and clinical findings associated with sickle cell disease include Vaso-occlusive crisis, pain crisis, chest pain, cough, fever, stroke, convulsions, tachypnea, leukocytosis, growth retardation, late sexual maturation, underweight. Cholelithiasis in children, hypertension, cataracts, meningitis, and para orbital facial infarction.
How is Sickle Cell Disease Diagnosed?
Sickle cell disease is diagnosed through the clinical presentation, screening for HbS at birth, hemoglobin electrophoresis, serum electrolytes, peripheral blood smear, creatinine, BUN, Urinalysis, CSF examination, and hemoglobin solubility testing.
How is Sickle Cell Disease Treated?
Sickle cell disease is treated through symptom control, management of illness complications, antimetabolites, opioid analgesics, antibiotics, and antiemetics.
What is the Prognosis of Sickle Cell Disease?
The prognosis of sickle cell disease is fair as it is a lifelong disease, morbidity also highly variable.
What are Thalassemia Syndromes?
Thalassemia syndromes is are a mixed group of hereditary disorders instigated by genetic lesions causing the reduced synthesis of α- or β-globin chain of HbA (α2β2).
Examples of thalassemia syndromes include:
- B thalassemia major
- B thalassemia minor
- A thalasemia
- Hydrops fetalis
What is B Thalassemia Major?
B thalassemia major is a severe transfusion dependent anemia with homozygous for β-thalassemia genes (β+/β+ or β0/β0).
What is the Pathology of B Thalassemia Major?
The pathology of β- thalassemia major is:
-Etiology: The cause of β- thalassemia major is gene mutation.
-Genes involved: for β-thalassemia gene.
Pathogenesis: The sequence of events that lead to β- thalassemia major result from promoter region mutations, preventing RNA polymerase from binding normally. Chain terminator mutations, causes premature termination of mRNA translation. Splicing mutations, aberrant splicing affecting the introns and exons. Diminished β-globin synthesis consequences in anemia, by fabricating under-hemoglobinized, hypochromic, microcytic red cells that have diminished survival.
-Morphology: The morphology associated with β- thalassemia major shows microcytosis, hypochromia.
Histology: The histology associated with β- thalassemia major shows anisocytosis, poikilocytosis, and basophilic stippling present.
How does B Thalassemia Major Present?
Patients with β- thalassemia major typically have no gender prevalence present at age range of 6 to 9 months of age. The symptoms, features, and clinical findings associated with β- thalassemia major include growth retardation, has a brief clinical course.
How is B Thalassemia Major Diagnosed?
B thalassemia major is diagnosed via prenatal molecular analysis of DNA.
How is B Thalassemia Major Treated?
B thalassemia major is treated mainly through bone marrow transplantation and blood transfusion or iron chelators.
What is the Prognosis of B Thalassemia Major?
The prognosis of β- thalassemia major is fair. With transfusions and iron chelation, survival into the third decade is likely.
What is B Thalassemia Minor?
B Thalassemia minor is asymptomatic with mild or absent anemia.
What is the Pathology of B Thalassemia Minor?
The pathology of β- thalassemia minor is:
-Etiology: The cause of β- thalassemia minor is a genetic mutation.
-Genes involved: β-thalassemia gene.Heterozygotes having one β-thalassemia gene and one normal gene (β+/β or β0/β) usually have mild microcytic anemia that causes no symptoms.
Pathogenesis: The sequence of events that lead to β- thalassemia minor result from promoter region mutations, preventing RNA polymerase from binding normally. Chain terminator mutations causes premature termination of mRNA translation: Splicing mutations, aberrant splicing affecting the introns and exons. Diminished β-globin synthesis consequences in anemia, by fabricating under-hemoglobinized, hypochromic, microcytic red cells that have diminished survival.
-Morphology: The morphology associated with β- thalassemia minor shows hypochromia, microcytosis.
-Histology: The histology associated with β- thalassemia minor shows basophilic stippling and target cells.
How does B Thalassemia Minor Present?
Patients with β- thalassemia minor typicallyhave no sex prevalrence present at age range of childhood and adulthood. The symptoms, features, and clinical findings associated with β- thalassemia minor include mild anemias, and asymptomatic.
How is B Thalassemia Minor Diagnosed?
β- thalassemia minor is diagnosed through lab works peripheral blood smear- abnormal red cells, hypochromia, microcytosis basophilic stippling, and target cells. Hemoglobin electrophoresis shows increase in HbA2.
How is B Thalassemia Minor Treated?
β- thalassemia minor is treated via management of symptoms, if any.
What is the Prognosis of B Thalassemia Minor?
The prognosis of β- thalassemia minor is good. Patients are asymptomatic with little or no anemia.
What is A Thalasemia?
A thalasemia is a syndromes group of genetic anemias of varying clinical severity.
What is the Pathology of A Thalasemia?
The pathology of α thalasemia is:
-Etiology: The cause of α thalasemia is gene mutation.
-Genes involved: α-globin genes
-Pathogenesis: The sequence of events that lead to α thalassemia are as the results from variety of molecular lesions result, but the most commonly deletion of α-globin.
-Morphology: The morphology associated with α thalasemia shows abnormal rashes.
-Histology: The histology associated with α thalasemia shows abnormal red blood cells.
How does A Thalasemia Present?
Patients with α thalasemia typically have no sex prevarence present at age range of infancy. The symptoms, features, and clinical findings associated with α thalasemia include, anamia, severe pallor, and hydrops fetalis.
How is A Thalasemia Diagnosed?
A thalasemia is diagnosed through laboratory evaluation such as hemoglobin electrophoresis, and genetic testing.
How is A Thalasemia Treated?
A thalasemia is treated through managing symptoms if any, iron and folic acid supplementation.
What is the Prognosis of A Thalasemia?
The prognosis of α thalasemia is good for silent carriers, poor for hydrops fetalis.
What is Hydrops Fetalis?
Hydrops fetalis is a solemn fetal disorder defined as atypical buildup of fluid in two/more fetal compartments.
What is the Pathology of Hydrops Fetalis?
The pathology of hydrops fetalis is:
-Etiology: The cause of hydrops fetalis is genetic factor.
-Genes involved: α-globin genes.
-Pathogenesis: The sequence of events that lead to hydrops fetalis are as the result of deletion of all four α-globin genes, γ-globin chains form hemoglobin Barts with high affinity for oxygen hence severe tissue anoxia.
-Morphology: The morphology associated with hydrops fetalis shows pallor and edema.
-Histology: Red blood cell changes.
How does Hydrops Fetalis Present?
Patients with hydrops fetalis typically slightly higher in males than females present at age range of infancy. The symptoms, features, and clinical findings associated with hydrops fetalis include severe pallor, generalized edema, and massive hepatosplenomegaly.
How is Hydrops Fetalis Diagnosed?
Hydrops fetalis is diagnosed through prenatal ultrasonography,
How is Hydrops Fetalis Treated?
Hydrops fetalis is treated via intrauterine transfusion.
What is the Prognosis of Hydrops Fetalis?
The prognosis of hydrops fetalis is poor with a high mortality.
What are bleeding disorders?
Bleeding disorders are condition with uncontrolled bleeding characterized with defect in the blood clotting process.
Examples of bleeding disorders include:
- Acute immune thrombocytopenic purpura
- Chronic immune thrombocytopenic purpura
- Drug-induced thrombocytopenia
- HIV-associated thrombocytopenia
- Thrombocytopenic purpura
- Uremic syndrome
- Bernard-Soulier syndrome
- Glanzmann thrombasthenia
- Clotting factor abnormalities
What is Acute immune Thrombocytopenic Purpura?
Acute immune thrombocytopenic purpura is an acute childhood syndrome where platelets coated with autoantibodies to platelet membrane antigens results in splenic sequestration and mononuclear macrophages phagocytosis.
What is the Pathology of Acute immune Thrombocytopenic Purpura?
The pathology of acute immune thrombocytopenic purpura is:
-Etiology: The cause of acute immune thrombocytopenic purpura is viral illness and drug therapy complications
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to acute immune thrombocytopenic purpura are as the result of the creation of autoantibodies against IIb-IIIa or Ib-IX platelet membrane glycoproteins. Opsonized platelets are considered vulnerable to phagocytosis by the cells of the mononuclear phagocyte system.
-Morphology: The morphology associated with acute immune thrombocytopenic purpura shows megathrombocytes and clumps of platelets.
-Histology: The histology associated with acute immune thrombocytopenic purpura shows increased megakaryocytes.
How does Acute immune Thrombocytopenic Purpura Present?
Patients with acute immune thrombocytopenic purpura typically affect both sexes present at an age range of childhood. The symptoms, features, and clinical findings associated with acute immune thrombocytopenic purpura include prolonged bleeding time, petechiae melena, hematuria.
How is Acute immune Thrombocytopenic Purpura Diagnosed?
Acute immune thrombocytopenic purpura is diagnosed through laboratory studies such as CBC count, peripheral blood smear, bone marrow aspirate shows megakaryocytes number increased. Other tests include bone marrow biopsy, and splenic evaluation.
How is Acute immune Thrombocytopenic Purpura Treated?
Acute immune thrombocytopenic purpura is treated through steroid therapy,
What is the Prognosis of Acute immune Thrombocytopenic Purpura?
The prognosis of acute immune thrombocytopenic purpura is good. The disease is self-limited.
What is Chronic Immune Thrombocytopenic Purpura?
Chronic immune thrombocytopenic purpura is syndrome associated platelets coated with autoantibodies to platelet membrane antigens results in splenic sequestration and mononuclear macrophages phagocytosis commonly in adults.
What is the Pathology of Chronic Immune Thrombocytopenic Purpura?
The pathology of chronic immune thrombocytopenic purpura is:
-Etiology: The cause of chronic immune thrombocytopenic purpura is autoimmune factors
-Genes involved: Unknown.
Pathogenesis: The sequence of events that lead to chronic immune thrombocytopenic purpura results from the creation of autoantibodies against IIb-IIIa or Ib-IX platelet membrane glycoproteins. Opsonized platelets are considered vulnerable to phagocytosis by the mononuclear phagocyte system cells.
-Morphology: The morphology associated with chronic immune thrombocytopenic purpura shows megathrombocytes and clumps of platelets.
-Histology: The histology associated with chronic immune thrombocytopenic purpura shows increased megakaryocytes.
How does Chronic Immune Thrombocytopenic Purpura Present?
Patients with chronic immune thrombocytopenic purpura typically have a female-to-male ratio is 3:1. Present at an age range of 40 years. The symptoms, features, and clinical findings associated with chronic immune thrombocytopenic purpura include bleeding in the skin, ecchymoses, bruising, gum bleeding, nose bleeding, soft tissue bleeding, splenomegaly and lymphadenopathy.
How is Chronic Immune Thrombocytopenic Purpura Diagnosed?
Chronic immune thrombocytopenic purpura is diagnosed through laboratory studies- CBC count, peripheral blood smear, bone marrow aspirate shows megakaryocytes number increased. Other tests include bone marrow biopsy, and splenic evaluation.
How is Chronic Immune Thrombocytopenic Purpura Treated?
Chronic immune thrombocytopenic purpura is treated through medical care steroid therapy. Splenectomy may be needed.
What is the Prognosis of Chronic Immune Thrombocytopenic Purpura?
The prognosis of chronic immune thrombocytopenic purpura is poor associated with relapse.
What is Drug Induced Thrombocytopenia?
Drug induced thrombocytopenia is a disorder linked to immunologically mediated destruction of platelets after drug ingestion.
What is the Pathology of Drug Induced Thrombocytopenia?
The pathology of drug induced thrombocytopenia is:
-Etiology: The cause of drug induced thrombocytopenia is certain drugs, e.g., heparin heparin-induced thrombocytopenia (HIT).
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to drug induced thrombocytopenia are the result of an immune reaction directed against a complex of heparin and platelet factor 4, which that binds firmly to heparin. The binding modifies the form of platelet factor 4, rendering it vulnerable to immune recognition. The binding yields immune complexes activating platelets and promoting thrombosis.
-Morphology: The morphology associated with drug induced thrombocytopenia shows thrombosis in large blood vessels
-Histology: Hemolysis.
How does Drug Induced Thrombocytopenia Present?
Patients with drug induced thrombocytopenia, typically common in females, present at an age range of 40 to 60 years. The symptoms, features, and clinical findings associated with drug induced thrombocytopenia include skin lesions at injection sites, an acute systemic reaction, fever, flushing, chest pain, and dyspnea.
How is Drug Induced Thrombocytopenia Diagnosed?
Drug induced thrombocytopenia is diagnosed through immunoassays ELISA test and functional assays HIPA and SRA. Imaging studies ultrasonography detect DVT.
How is Drug Induced Thrombocytopenia Treated?
Drug induced thrombocytopenia is treated through discontinuation of the drug and long-term monitoring.
What is the Prognosis of Drug Induced Thrombocytopenia?
The prognosis of drug induced thrombocytopenia is fair, with mortality and complications of HIT of 6-10%.
What is HIV-Associated Thrombocytopenia?
HIV-associated thrombocytopenia is rarely a serious clinical problem associated with impaired platelet production and increased obliteration in HIV infection.
What is the Pathology of HIV-Associated Thrombocytopenia?
The pathology of HIV-associated thrombocytopenia is:
-Etiology: The cause of HIV-associated thrombocytopenia is HIV infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to HIV-associated thrombocytopenia are as the result of diseased megakaryocytes prone to apoptosis, and diminished in terms of platelet production. HIV infection may cause dysregulation, and hyperplasia of B cells, which influence the advance of immune-mediated thrombocytopenia.
-Morphology: Rashes.
-Histology: Low platelet count.
How does HIV-Associated Thrombocytopenia Present?
Patients with HIV-associated thrombocytopenia typically have no gender prevalence present at an age range of childhood and adulthood. The symptoms, features, and clinical findings associated with HIV-associated thrombocytopenia include platelet counts of less than 150,000/µL in clinical presentation, fever, hemolytic anemia, and neurologic and renal dysfunction.
How is HIV-Associated Thrombocytopenia Diagnosed?
HIV-associated thrombocytopenia is diagnosed through platelet count.
How is HIV-Associated Thrombocytopenia Treated?
HIV-associated thrombocytopenia is treated through immune-based therapy.
What is the Prognosis of HIV-Associated Thrombocytopenia?
The prognosis of HIV-associated thrombocytopenia is fair. Respond fairly to immune-based therapy though associated with relapse.
What is Thrombocytopenic Purpura?
Thrombocytopenic purpura is a range of clinical conditions, including thrombocytopenic purpura (TTP) and hemolytic-uremic syndrome (HUS).
What is the Pathology of Thrombocytopenic Purpura?
The pathology of thrombocytopenic purpura is:
-Etiology: The cause of thrombocytopenic purpura is unknown, associated with deficiency of ADAMTS13 enzyme.
-Genes involved: Gene that codes for ADAMTS13.
-Pathogenesis: The sequence of events that lead to thrombocytopenic purpura is unknown, believed to be associated with deficiency of ADAMTS13 enzyme.
-Morphology: The morphology associated with thrombocytopenic purpura shows lesions prominent in the CNS and kidneys.
-Histology: The histology associated with thrombocytopenic purpura shows thrombi platelet-rich and fibrin-poor.
How does Thrombocytopenic Purpura Present?
Patients with thrombocytopenic purpura typically have a female predominance present at an age range of 40 years. The symptoms, features, and clinical findings associated with thrombocytopenic purpura include fever, seizures, hemiplegia, paresthesias, visual disturbance, fatigue, severe bleeding and aphasia.
How is Thrombocytopenic Purpura Diagnosed?
Thrombocytopenic purpura is diagnosed through laboratory studies-platelet count, CBC count, blood smears, coagulation studies, serum bilirubin and lactate dehydrogenase levels.
How is Thrombocytopenic Purpura Treated?
Thrombocytopenic purpura is treated through plasma exchange with fresh frozen plasma. Medical care such as Caplacizumab and Octaplas.
What is the Prognosis of Thrombocytopenic Purpura?
The prognosis of thrombocytopenic purpura is good with ideal diagnosis and treatment.
What is Uremic Syndrome?
Uremic syndrome is a clinical condition characterized by advanced kidney failure allied to thrombocytopenia and microangiopathic hemolytic anemia.
What is the Pathology of Uremic Syndrome?
The pathology of the uremic syndrome is: disorder classified into two core categories, dependent on whether it is linked with Shiga toxin (Stx) or not. Typical (Stx–associated) HUS and atypical (non–Stx-associated) HUS.
-Etiology: The cause of uremic syndrome is infections, pregnancy, and puerperium.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to uremic syndrome as the result of damage to endothelial cells.
-Morphology: The morphology associated with uremic syndrome shows diffuse thickening of the glomerular capillary wall.
-Histology: The histology associated with uremic syndrome shows fibrin thrombi.
How does Uremic Syndrome Present?
Patients with uremic syndrome typically have no sex prevalence present at an age range of childhood to adulthood. The symptoms, features, and clinical findings associated with uremic syndrome include hypertension, edema, fluid overload, severe pallor, seizures, anuria, irritability, and lethargy.
How is Uremic Syndrome Diagnosed?
Uremic syndrome is diagnosed through laboratory Studies- BUN, serum creatinine, serum electrolyte levels, and urinalysis. Peripheral smear decreased platelet counts, ADAMTS-13 activity: imaging studies- kidney ultrasonography.
How is Uremic Syndrome Treated?
Uremic syndrome is treated through medical care including monoclonal antibodies (eculizumab and ravulizumab) corticosteroids, and antioxidants. Plasma therapy, immunoglobulin (IgG), antiplatelet agent, fibrinolytic agents.
What is the Prognosis of Uremic Syndrome?
The uremic syndrome prognosis is fair. Uremic syndrome is associated with recurrence, progressing to end stage renal disease.
What is Bernard-Soulier Syndrome?
Bernard-Soulier syndrome is a condition caused by an inherited deficiency of the platelet membrane glycoprotein complex Ib-IX.
What is the Pathology of Bernard-Soulier Syndrome?
The pathology of Bernard-Soulier syndrome is:
-Etiology: The cause of Bernard-Soulier syndrome is reduced expression of the GPIb/IX/V complex.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to bernard-soulier syndrome results from the reduced expression of the GPIb/IX/V complex on the surface of the platelets, the receptor for von Willebrand factor (vWF). The diminished expression is the deficient binding of vWF to the platelet membrane at vascular injury sites, subsequent to faulty platelet adhesion.
-Morphology: The morphology associated with Bernard-Soulier syndrome shows giant platelets.
-Histology: The histology associated with Bernard-Soulier syndrome shows thrombocytopenia.
How does Bernard-Soulier Syndrome Present?
Patients with bernard-soulier syndrome typically have no gender prevalence present at an age range of any age. The symptoms, features, and clinical findings associated with bernard-soulier syndrome include easy bruising, petechial rash, gastrointestinal bleeding, nosebleeds, purpura, and menorrhagia.
How is Bernard-Soulier Syndrome Diagnosed?
Bernard-soulier syndrome is diagnosed through CBC count, peripheral smear indicates giant platelets and thrombocytopenia, bleeding time- prolonged. Flow cytometry and platelet aggregation studies may be helpful.
How is Bernard-Soulier Syndrome Treated?
Bernard-soulier syndrome is treated through supportive care, broad-based treatment-desmopressin acetate, antifibrinolytic agents for episodic bleeding. Platelet transfusion may be needed.
What is the Prognosis of Bernard-Soulier Syndrome?
The prognosis of Bernard-soulier syndrome is poor.
What is Glanzmann Thrombasthenia?
Glanzmann thrombasthenia is an erratic platelet ailment characterized by plate.lets that have qualitative/quantitative shortages of the fibrinogen receptor αIIbβ3.
What is the Pathology of Glanzmann Thrombasthenia?
The pathology of glanzmann thrombasthenia is:
-Etiology: The cause of glanzmann thrombasthenia is genetic factors.
-Genes involved: ITGA2B or ITGB3 genes
-Pathogenesis: The sequence of events that lead to glanzmann thrombasthenia results from thrombasthenic platelets failing to aggregate in retort to ADP, epinephrine, collagen, or thrombin due to deficit or disfunction of glycoprotein IIb-IIIa, required in the establishment of bonds amid platelets thru binding fibrinogen and vWF.
-Morphology: Rashes.
-Histology: Red blood cell changes.
How does Glanzmann Thrombasthenia Present?
Patients with Glanzmann thrombasthenia typically have a female predominance present at age range of childhood. The symptoms, features, and clinical findings associated with glanzmann thrombasthenia include mucosal haemorrhage, gingival haemorrhage, petechiae and ecchymoses, menorrhagia, and gastrointestinal haemorrhage.
How is Glanzmann Thrombasthenia Diagnosed?
Glanzmann thrombasthenia is diagnosed through laboratory evaluation such as prothrombin time, complete blood cell count, activated partial thromboplastin time, monoclonal antibodies test, and flow cytometry.
How is Glanzmann Thrombasthenia Treated?
Glanzmann thrombasthenia is treated preventive measures, avoidance of antiplatelet agents, and platelet transfusion.
What is the Prognosis of Glanzmann Thrombasthenia?
The prognosis of glanzmann thrombasthenia is good with appropriate supportive care.
What are Clotting Factor Abnormalities?
Clotting factor abnormalities are prolonged bleeding time due to hereditary/acquired deficiency disorders associated with the cloting factors.
Examples of clotting factor abnormalities include:
- Hemophilia A
- Hemophilia B
- Von Willebrand disease
What is Hemophilia A?
Hemophilia A is a recessive syndrome of bleeding triggered by qualitative/quantitative defects relating to the factor VIII-vWF complex.
What is the Pathology of Hemophilia A?
The pathology of hemophilia A is:
-Etiology: The cause of hemophilia A is inherited or acquired genomic mutation X-linked recessive pattern, a factor VIII deficiency.
-Genes involved: multiple coagulation factor deficiencies 2 (MCFD2, lectin mannose binding protein 1 (LMAN1)
-Pathogenesis: The sequence of events that lead to hemophilia A results from a decrease in the amount and activity of factor VIII that obliges as a cofactor for factor IX in the activation of factor X in the coagulation cascade.
-Morphology: Clinical feature correlates with the level of factor VIII activity,< 1% leads to severe disease, 2 to 5% moderate disease, 6 to 50% causes mild disease.
-Histology: Red blood cell changes.
How does Hemophilia A Present?
Patients with hemophilia A typically occurs predominantly in males present at an age range of childhood and adulthood. The symptoms, features, and clinical findings associated with hemophilia A include hematemesis, melena pain, stiffness of the joint, weakness, orthostasis, tachycardia, tachypnea. Renal colic, epistaxis, and hemoptysis may also be present.
How is Hemophilia A Diagnosed?
Hemophilia A is diagnosed through CBC count, prothrombin time, activated partial thromboplastin time, FVIII assay tests, and FVIII inhibitor assay tests.
How is Hemophilia A Treated?
Hemophilia A is treated through prophylaxis, managing hemostasis, managing factor VIII (FVIII) inhibitors with plasma-based FVIII concentrates. Pain medications and monoclonal antibody therapy- emicizumab. I.V recombinant activated factor VII.
What is the Prognosis of Hemophilia A?
The prognosis of hemophilia A is good with appropriate education and treatment.
What is Hemophilia B?
Hemophilia B is is an inherited, X-linked, recessive syndrome that results from the deficiency of plasma coagulation factor IX.
What is the Pathology of Hemophilia B?
The pathology of hemophilia b is:
-Etiology: The cause of hemophilia b is the mutation in the factor IX gene.
-Genes involved: Factor IX gene.
-Pathogenesis: The sequence of events that lead to hemophilia b results from a wide range of alterations linking the factor IX gene.
-Morphology: Rash.
-Histology: Red blood cell changes.
How does Hemophilia B Present?
Patients with hemophilia b are typically predominant in males present at an age range of childhood to adulthood. The symptoms, features, and clinical findings associated with hemophilia b include T Prolonged bleeding, soft-tissue haemorrhage, tachycardia, hypotension, orthostasis.
How is Hemophilia B Diagnosed?
Hemophilia b is diagnosed by CBC count, prothrombin time(normal), partial thromboplastin time (prolonged). FVIII assay tests and FVIII inhibitor assay tests are also helpful.
How is Hemophilia B Treated?
Hemophilia b is treated through medical care- coagulation therapy, recombinant factor IX, factor IX complex, factor IX. Recombinant coagulation factor IX. Antifibrinolytics, antihemophilic agent analgesics, and monoclonal antibodies.
What is the Prognosis of Hemophilia B?
The prognosis of hemophilia B is good. Patients can live long and productive with proper management and education.
What is Von Willebrand Disease?
Von Willebrand disease is a common hereditary ailment of bleeding, are instigated by quantitative/qualitative faults relating to the factor VIII-vWF complex.
What is the Pathology of Von Willebrand Disease?
The pathology of von willebrand disease is:
-Etiology: The cause of von willebrand disease is a genetic mutation.
-Genes involved: MCFD2 and LMAN1 and vWF gene
-Pathogenesis: The sequence of events that lead to von willebrand disease as the result of decrease in the amount and activity of factor VIII that obliges as a cofactor for factor IX in the activation of factor X in the coagulation cascade.
-Morphology: Clinically, it is featured by extreme hemorrhage from wounds, spontaneous bleeding of mucous membranes, menorrhagia, and a lengthy bleeding time.
-Histology: Red blood cell changes.
How does Von Willebrand Disease Present?
Patients with von willebrand disease typically have no gender prevalence present at an age range of infancy. The symptoms, features, and clinical findings associated with von willebrand disease include extreme hemorrhage from wounds, unprompted bleeding of mucous membranes, menorrhagia, and a lengthy bleeding time. Though have a normal platelet count.
How is Von Willebrand Disease Diagnosed?
Von Willebrand disease is diagnosed through laboratory studies- Prothrombin time (PT), factor VIII (FVIII) coagulant activity, concentration of vWF antigen (vWF:Ag), ristocetin cofactor (RCoF) activity, and activated partial thromboplastin time (aPTT) tests.
How is Von Willebrand Disease Treated?
Von Willebrand disease is treated through antidiuretic hormone vasopressin synthetic analogue (Desmopressin), von willebrand factor/factor VIII (vWF/FVIII) concentrates, and recombinant von Willebrand factor (rVWF).
What is the Prognosis of Von Willebrand Disease?
The prognosis of Von Willebrand disease is fair.
What is Polycythemia?
Polycythemia is an abnormality with high red cells and haemoglobin concentrations levels
Examples of polycythemia include:
- Polycythemia Vera
What is Polycythemia Vera?
Polycythemia Vera is a stem cell syndrome characterized as a panhyperplastic, malignant, and neoplastic marrow disorder.
What is the Pathology of Polycythemia Vera?
The pathology of polycythemia vera is:
-Etiology: The cause of polycythemia vera is the tolerant neoplastic proliferation.
-Genes involved: JAK2V617F, JAK2 exon.
-Pathogenesis: The sequence of events that lead to polycythemia vera results from transmutations of the erythropoietin receptor leading to hyperresponsiveness to erythropoietin.
-Morphology: Platelet changes.
-Histology: The histology associated with polycythemia vera shows increased red cells
How does Polycythemia Vera Present?
Patients with polycythemia vera typically higher in males present at an age range of 50 to 70 years. The symptoms, features, and clinical findings associated with polycythemia vera include vertigo, headache, tinnitus, visual disturbances, dizziness, and angina pectoris.
How is Polycythemia Vera Diagnosed?
Polycythemia vera is diagnosed through laboratory studies- hematocrit and Hb level, serum erythropoietin level, and bone marrow biopsy indicating hypercellularity.
How is Polycythemia Vera Treated?
Polycythemia vera is treated through aspirin, and cytoreductive therapy. Surgical intervention such as splenectomy may be useful. Phlebotomy may be needed.
What is the Prognosis of Polycythemia Vera?
The prognosis of polycythemia vera is good with proper management of symptoms.
What are Transfusion Reactions?
Transfusion reactions are the type of reactions that are antibody-mediated and occur after blood transfusion.
Transfusion reactions include:
- Febrile non-hemolytic transfusion reaction
- Mild allergic transfusion reaction
- Acute hemolytic transfusion reaction
- Anaphylactic transfusion reaction
- Transfusion related acute lung injury
- Transfusion associated circulatory overload
- Delayed hemolytic transfusion reaction
- Transfusion associated graft versus host disease
What is Febrile Non-hemolytic Transfusion Reaction?
Febrile non-hemolytic transfusion reaction is a reaction that occurs as a result of antibodies attacking the white blood cells and is characterized by increased body temperature.
What is the Pathology of Febrile Non-Hemolytic Transfusion Reaction?
The pathology of febrile non-hemolytic transfusion reaction is:
-Etiology: The cause of febrile non-hemolytic transfusion reaction is the accumulation of cytokines in the blood.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to febrile non-hemolytic transfusion reaction during blood storage is the development of antibodies against the leukocytes. These antibodies fight the white blood cells, causing a reaction once transfusion is done.
-Morphology: NA
-Histology: NA
How does Febrile Non-Hemolytic Transfusion Reaction Present?
Patients with febrile non-hemolytic transfusion reaction typically affect males and females present at an age range of childhood to adulthood. The symptoms, features, and clinical findings associated with include fever, chills, and malaise.
How is Febrile Non-Hemolytic Transfusion Reaction Diagnosed?
Febrile non-hemolytic transfusion reaction is diagnosed physical examination, vital signs monitoring.
How is Febrile Non-Hemolytic Transfusion Reaction Treated?
Febrile non-hemolytic transfusion reaction is treated by management of the symptoms which include antipyretics and leukocytes therapy, steroids and stopping the blood transfusion.
What is the Prognosis of Febrile Non-Hemolytic Transfusion Reaction?
The prognosis of febrile non-hemolytic transfusion traction is good.
What is Mild Allergic Transfusion Reaction?
Mild allergic transfusion reaction is reaction that occur during or after a blood transfusion and have a low degree of emergency compared to the rest and is characterized by pruritis, flushing or urticaria.
What is the Pathology of Mild Allergic Reaction?
The pathology of mild allergic transfusion reaction is:
-Etiology: The cause of mild allergic transfusion reaction is administration of the wrong blood, hypersensitivity, presence of histamines and bradykinins.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mild allergic transfusion reaction is when that antibodies are formed against the components of the donor’s blood and are mediated to attack them.
-Morphology: NA
-Histology: NA
How does Mild Allergic Transfusion Reaction Present?
Patients with mild allergic transfusion reaction typically female present at age range of from 3 years. The symptoms, features, and clinical findings associated with mild allergic transfusion reaction include urticaria, pruritis, flushing and wheezing at times.
How is Mild Allergic Transfusion Reaction Diagnosed?
Mild allergic transfusion reaction is diagnosed mostly by physical examination.
How is Mild Allergic Transfusion Reaction Treated?
Mild allergic transfusion reaction is treated by cessation of blood transfusion, antihistamines administration.
What is the Prognosis of Mild Allergic Transfusion Reaction?
The prognosis of mild allergic transfusion reaction is good since it has a higher chance of survival rate, and one can re-initiate the transfusion again.
What is Acute Hemolytic Transfusion Reaction?
Acute hemolytic transfusion reaction is an immune-mediated or a non- immune-mediated transfusion reaction that leads to blood hemolysis and it fatal and life-threatening.
What is the Pathology of Acute Hemolytic Transfusion Reaction?
The pathology of acute hemolytic transfusion reaction is:
-Etiology: The cause of acute hemolytic transfusion reaction is ABO incompatibility, administration of the wrong type of blood.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acute hemolytic transfusion reaction is when on is given the wrong type of blood the recipient’s antibodies destroy the donors’ blood, and the coagulation cascade is activated, which at the end it leads to blood hemolysis
-Morphology: NA
-Histology: NA
How does Acute Hemolytic Transfusion Reaction Present?
Patients with acute hemolytic transfusion reaction typically both male and female present at an age range of childhood. The symptoms, features, and clinical findings associated with acute hemolytic transfusion reaction include fever, chills, chest pain, back pain, dyspnea, low blood pressure.
How is Acute Hemolytic Transfusion Reaction Diagnosed?
Acute hemolytic transfusion reaction is diagnosed by blood grouping and crossmatching, direct antiglobulin test and blood microscopy.
How is Acute Hemolytic Transfusion Reaction Treated?
Acute hemolytic transfusion reaction is treated by immediate cessation of the blood transfusion, diuretics furosemide, fluid replacement therapy, close monitoring of the vital signs and vasodilators to improve the cardiac output.
What is the Prognosis of Acute Hemolytic Transfusion Reaction?
The prognosis of acute hemolytic transfusion reaction poor since the reaction can be fatal even with the smallest millimeter of blood.
What is Anaphylactic Transfusion Reaction?
Anaphylactic transfusion reaction is a reaction of the blood that occurs to patient who lack the IgA antibody and occurs mostly during transfusion of platelets.
What is the Pathology of Anaphylactic Transfusion Reaction?
The pathology of anaphylactic transfusion reaction is the study of the reaction that occurs in blood of those lacking the IgA antibodies.
-Etiology: The cause of anaphylactic transfusion reaction is hypersensitivity to the allogenic proteins in the plasma.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anaphylactic transfusion reaction the formation of the IgA antibodies in a patient who lack the IgA. Leading to the formation of a reaction since it will be considered as foreign and a response will be triggered.
-Morphology: NA
-Histology: NA
How does Anaphylactic Transfusion Reaction Present?
Patients with anaphylactic transfusion reaction typically are female present at age range of from 9 years. The symptoms, features, and clinical findings associated with anaphylactic transfusion reaction include cough, dyspnea, hypotension, urticaria and skin flushing, nausea, vomiting and diarrhea cyanosis, dyspnea.
How is Anaphylactic Transfusion Reaction Diagnosed?
Anaphylactic transfusion reaction is diagnosed by physical examination of the symptoms presenting immediately transfusion is commenced.
How is Anaphylactic Transfusion Reaction Treated?
Anaphylactic transfusion reaction is treated antihistamines, epinephrine, oxygen therapy and fluid replacement therapy and supportive care.
What is the Prognosis of Anaphylactic Transfusion Reaction?
The prognosis of anaphylactic transfusion reaction is fair since once the allergen is noted the reaction can be avoidable.
What is Transfusion Related Acute Lung Injury?
Transfusion related acute lung injury is a disease that occurs on the lungs after a blood transfusion is done.
What is the Pathology of Transfusion Related Acute Lung Injury?
The pathology of transfusion related acute lung injury is the study of disease that affect the lung after a transfusion process has occurred.
-Etiology: The cause of transfusion related acute lung injury is not fully understood but it is immune mediated, underlying condition, massive transfusion.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to transfusion related acute lung injury are: plasma containing high levels of anti-HLA antibodies which bind to leucocytes of recipient. These leucocytes then aggregate in pulmonary micro-mutation and release mediators of increased vascular permeability resulting in acute pulmonary oedema and signs and symptoms of respiratory failure.
-Morphology: NA
-Histology: NA
How does Transfusion Related Acute Lung Injury Present?
Patients with transfusion related acute lung injury typically affect male more than female present at age range of less than 20 years. The symptoms, features, and clinical findings associated with transfusion related acute lung injury include cyanosis, fever, hypoxemia, dyspnea and hypotension.
How is Transfusion Related Acute Lung Injury Diagnosed?
Transfusion related acute lung injury is diagnosed by plasma levels of the brain natriuretic peptide, blood culture.
How is Transfusion Related Acute Lung Injury Treated?
Transfusion related acute lung injury is treated by immediate discontinuation of the blood transfusion, oxygen therapy and treat the symptoms as they occur.
What is the Prognosis of Transfusion Related Acute Lung Injury?
The prognosis of transfusion related acute lung injury is good.
What is Transfusion Associated Circulatory Overload?
Transfusion associated circulatory overload is when transfusion as caused fluid overload in the circulatory system and characterized by pulmonary edema.
What is the Pathology of Transfusion Associated Circulatory Overload?
The pathology of transfusion associated circulatory overload is: the disease that occurs after or during blood transfusion that lead to fluid overload in the pulmonary system.
-Etiology: The cause of transfusion associated circulatory overload is excess blood transfusion, underlying cardiogenic disease and renal disease.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to transfusion associated circulatory overload is wen the patient has ana underlying condition that predisposes them to fluid overload. Also when the transfusion rate is not well monitored and the amount being transfused is excess.
-Morphology: NA
-Histology: NA
How does Transfusion Associated Circulatory Overload Present?
Patients with transfusion associated circulatory overload typically all gender present at age range of the most elderly. The symptoms, features, and clinical findings associated with transfusion associated circulatory overload include acute respiratory distress, increased blood pressure, chest pain, tachycardia, acute pulmonary edema.
How is Transfusion Associated Circulatory Overload Diagnosed?
Transfusion associated circulatory overload is diagnosed by physical examination of the symptoms, ranges of the brain natriuretic peptide, chest X-ray and history taking.
How is Transfusion Associated Circulatory Overload Treated?
Transfusion associated circulatory overload is treated by cessation of the transfusion, upright positioning of the patient, intubation,, oxygenation, splitting of the blood into tolerable portions.
What is the Prognosis of Transfusion Associated Circulatory Overload?
The prognosis of transfusion associated circulatory overload is poor since the reaction if very fatal and can lead to death immediately.
What is Delayed Hemolytic Transfusion Reaction?
Delayed hemolytic transfusion reaction is a type of reaction that occurs 2 to several months later after blood transfusion and is characterized by hemolysis.
What is the Pathology of Delayed Hemolytic Transfusion Reaction?
The pathology of delayed hemolytic transfusion reaction is:
-Etiology: The cause of delayed hemolytic transfusion reaction is development of antibodies to red blood cells antigens.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to delayed hemolytic transfusion reaction occurs later after transfusion due to the amnestic response if the immune system to a foreign red blood cell.
-Morphology: NA
-Histology: NA
How does Delayed Hemolytic Transfusion Reaction Present?
Patients with delayed hemolytic transfusion reaction typically female present at age range of adulthood. The symptoms, features, and clinical findings associated with delayed hemolytic transfusion reaction include fever, mild jaundice, drop in the Hb levels.
How is Delayed Hemolytic Transfusion Reaction Diagnosed?
Delayed hemolytic transfusion reaction is diagnosed history taking, Hb levels, direct antiglobulin test.
How is Delayed Hemolytic Transfusion Reaction Treated?
Delayed hemolytic transfusion reaction is treated avoid red blood cells transfusion again, high dosage of steroids is recommended, pain medication.
What is the Prognosis of Delayed Hemolytic Transfusion Reaction?
The prognosis of delayed hemolytic transfusion reaction is fair if diagnosed and noted early.
What is Transfusion Associated Graft Versus Host Disease?
Transfusion associated graft versus host disease is a reaction that occurs when transfusion of the bone marrow or other blood components is used is rejected by the host cells.
What is the Pathology of Transfusion Associated Graft Versus Host Disease?
The pathology of transfusion associated graft versus host disease is:
-Etiology: The cause of transfusion associated graft versus host is idiopathic
-Genes involved: NA
-Pathogenesis: The sequence of events that lead to transfusion associated graft versus host disease occurs when the donated components in the body of the host are viewed as foreign, and they begin to be attacked by the host cells
-Morphology: NA
-Histology: NA
How does Transfusion Associated Graft Versus Host Disease Present?
Patients with transfusion associated graft versus host disease typically more in male present at age range of the elderly. The symptoms, features, and clinical findings associated with transfusion associated graft versus host disease include fever, rash, diarrhea, bone marrow suppression, hepatitis, pruritic and painful rash.
How is Transfusion Associated Graft Versus Host Disease Diagnosed?
Transfusion associated graft versus host disease is diagnosed physical examination, complete blood count, liver function tests, Schirmer test, barium swallow meal.
How is Transfusion Associated Graft Versus Host Disease Treated?
Transfusion associated graft versus host disease is treated by immunosuppressors.
What is the Prognosis of Transfusion Associated Graft Versus Host Disease?
The prognosis of transfusion associated graft versus host disease poor since it is very fatal.
Table showing the transfusion reactions and the treatment, symptoms, and prognosis.
| Reaction | Time frame of occurrence | Symptoms | Treatment | Prognosis |
| Febrile Non-hemolytic Transfusion Reaction | During transfusion or the first 1-2 hours after. | Fever, chills, dyspnea | Antipyretics, stop transfusion. | good |
| Mild Allergic Transfusion Reaction | During transfusion | Urticaria, pruritis, flushing mild wheezing | Antihistamines, stop the transfusion | good |
| Acute Hemolytic Transfusion Reaction | Fever, chills, chest pain, hypotension | Stop transfusion, oxygen therapy, fluid replacement | Poor | |
| Anaphylactic transfusion reaction | Immediately, seconds after initiation of transfusion | Rash, pruritis, edema, hypotension, vomiting, diarrhea | Stop transfusion, fluid therapy, epinephrine | |
| Transfusion related acute lung injury | Withing 4-6 hours after | Tachypnea, dyspnea, fever, hypotension | Stop transfusion, oxygen therapy, intubation | Poor due to increased chances of fatality |
| Transfusion associate circulatory overload | 4-6 hours post transfusion. | Dyspnea, tachypnea, cough, chest pain, | Stop transfusion, diuretics, | Poor due to high fatality rate |
| Delayed Hemolytic Transfusion Reaction | 2days to several months | Drop in the Hb, fever, jaundice | Avoid transfusion, high dose of steroids and pain medication | Fair |
| Transfusion Associated Graft Versus Host Disease | 3-30 days after transfusion | Fever, diarrhea, erythematous rash | Immunosuppressors | Poor prognosis |