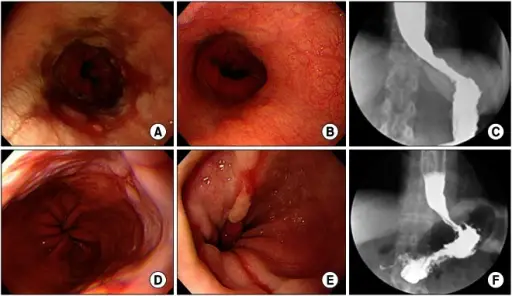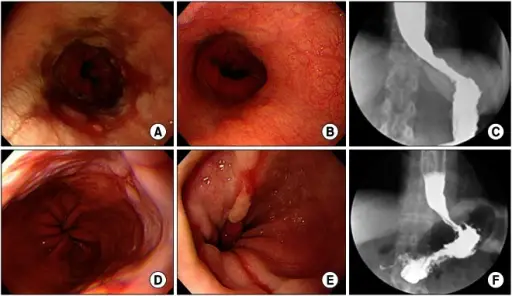
(A-C) A 42-year-old female patient was administered 30 mg lansoprazole QD for 17 months, but was hospitalized due to the lack of improvement in dysphagia. (A) Preoperative upper gatrointestinal (GI) endoscopy. Semicircular erosions (occupying about 75% of the lumen) are noted on the lower esophagus, including multiple linear mucosal breaks. Focal upward projection of the Z-line with salmon-colored mucosal changes is also noted. (B) Fourteen months later, postoperative upper GI endoscopy was performed, demonstrating that the erosion of the Z-line was alleviated and reflux esophagitis was resolved. (C) Seven months later, postoperative barium esophagography was performed, demonstrating no evidence of extraluminal contrast leakage or significant contrast passage disturbances at the gastroesophageal junction. Proximal esophageal dilatation improved but still remained. Symptoms were alleviated after surgery, so the patient stopped taking lansoprazole. (D-F) A 67-year-old female patient was administered 40 mg esomeprazole QD for 8 months, but was hospitalized due to the lack of improvement in regurgitation. (D) Preoperative upper GI endoscopy. Reflux esophagitis is noted on the lower esophagus, including two 6 mm mucosal breaks. (E) After 28 months, postoperative upper GI endoscopy was performed, demonstrating reflux esophagitis with recurrent mucosal breaks and ulcerations. (F) After three months, a postoperative barium esophagography was performed, demonstrating mild luminal narrowing at the anastomotic site and no significant passage disturbances. Eight months after surgery, the patient is still being administered the same dose of esomeprazole for five months due to the lack of symptom improvement. Early experiences of minimally invasive surgery to treat gastroesophageal reflux disease. Lee SB, Jeon KM, Kim BS, Kim KC, Jung HY, Choi YB - Journal of the Korean Surgical Society (2013). Not Altered. CC.
Reflux esophagitis is an esophageal mucosal injury that occurs secondary to retrograde flux of gastric contents into the esophagus. Clinically, this is referred to as gastroesophageal reflux disease or GERD.
What is the Pathology of Reflux Esophagitis?
The pathology of reflux esophagitis is:
-Etiology: The cause of reflux esophagitis is acid reflux also called gastroesophageal reflux disease or GERD. It is a backflow of digestive acid from the stomach, resulting in a chemical burn of the esophagus.
-Genes involved: FOXF1, MHC, CCND1.
-Pathogenesis: The sequence of events that lead to reflux esophagitis indicate that reflux esophagitis is the result of the failure of the lower esophageal sphincter to prevent the regurgitation of gastroduodenal secretions with subsequent esophageal mucosal injury.
-Histology: The histology associated with reflux esophagitis shows basal cell hyperplasia, elongation of vascular papillae, intercellular edema, presence of intraepithelial eosinophils, intraepithelial lymphocytosis, ballooning degeneration of squamous cells.
How does Reflux Esophagitis Present?
Patients with reflux esophagitis typically more in women and present at after 50s. The symptoms, features, and clinical findings associated with reflux esophagitis include heartburn, dysphagia, pain may be mistaken for myocardial infarction.
How is Reflux Esophagitis Diagnosed?
Reflux esophagitis is diagnosed by clinical heartburn, regurgitation, and intraesophageal pH monitoring to detect acid.
How is Reflux Esophagitis Treated?
Reflux esophagitis is treated by proton pump inhibitor therpay.
What is the Prognosis of Reflux Esophagitis?
The prognosis of reflux esophagitis is good. Chronic cases often respond to prescription drugs, and severe cases may require surgery to avoid serious complications.