Sepsis is a potentially life-threatening condition that occurs when the body’s response to an infection damages its own tissues which cause organs to function poorly and abnormally.
What is the Pathology of Sepsis?
The pathology of sepsis is:
-Etiology: The cause of sepsis is inflammation, edema, erythema, discharge of pus, with positive Gram stain and culture results from incision and drainage or deep cultures.
-Pathogenesis: The sequence of events that lead to sepsis is from the effects of circulating bacterial products, mediated by cytokine release and caused by sustained bacteremia. The clinically observable effects of bacteremia in the host are occurring because of cytokines.
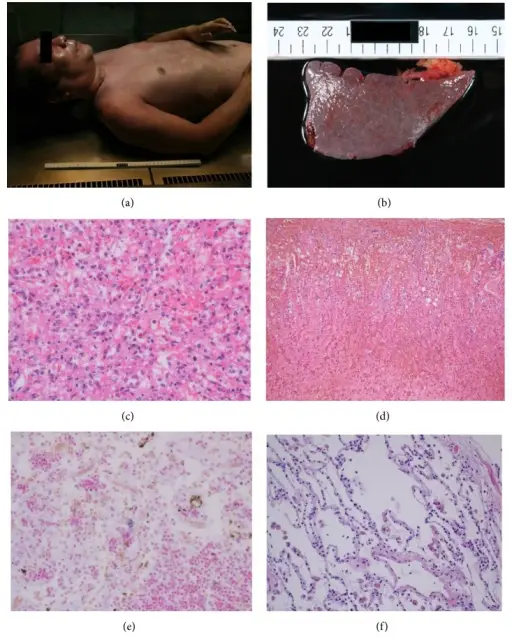
-Morphology: The morphology associated with sepsis shows that Gram-positive bacteria are the most common etiologic pathogens, although the incidence of gram-negative sepsis remains substantial, the incidence of fungal sepsis has been rising with more patients on immunosuppressive therapies and more cases of HIV infection.
How does Sepsis Present?
Patients with sepsis typically are males present at the age range of older than 65-years-old. The symptoms, features, and clinical findings associated with sepsis include fever or chills, confusion or disorientation, difficulty breathing, fast heart rate, or low blood pressure (hypotension), extreme pain, and sweaty skin. The signs of sepsis include a change in mental status, systolic blood pressure less than or equal to 100 mm Hg, and respiratory rate higher than or equal to 22 breaths per minute.
How is Sepsis Diagnosed?
Sepsis is diagnosed with multiple clinical, laboratory, radiologic, and microbiologic data. The diagnosis of sepsis may include blood culture and urine analysis and culture; chemistry studies that can suggest organ dysfunction, such as liver or kidney function tests; chest radiology; diagnostic imaging of the chest and abdomen or pelvis; cardiac studies such as ECG and troponins, as indicated; interventions such as paracentesis, thoracentesis, lumbar puncture, or aspiration of an abscess, as clinically indicated, and; measurement of biomarkers of sepsis such as procalcitonin levels.
How is Sepsis Treated?
Sepsis is treated with intravenous (IV) antibiotics to fight the infection, medications to increase blood pressure, insulin to stabilize blood sugar, corticosteroids to reduce inflammation, and pain relievers to help with discomfort.
What is the Prognosis of Sepsis?
The prognosis of sepsis is fair. It depends on underlying health status and host defenses, prompt and adequate surgical drainage of abscesses, relief of any obstruction of the intestinal or urinary tract, and appropriate and early empiric antimicrobial therapy. If it’s treated in a timely manner and with appropriate therapy, the prognosis is usually good, except in those with intra-abdominal or pelvic abscesses due to organ perforation.