Skin pathology is the description of the clinical appearance of the skin at gross and microscopic examination, its structure and functional changes in the presence of ailments.
Skin pathology includes:
- Infections of the skin
- Disorders of epidermal appendages
- Disorders of epidermal maturation
- Acute inflammatory dermatoses
- Chronic inflammatory dermatoses
- Panniculitis
- Premalignant and malignant epidermal tumors
- Disorders of pigmentation and melanocytes
- Benign epithelial tumors
- Adnexal tumors
- Tumors of the dermis
- Bullous diseases
- Tumors of cellular migrants to the skin
- Familial cancer syndromes with skin manifestations
What is Skin?
Skin is technically the largest organ in your body that functions as sensory and mechanical barrier organs with vitamin D synthesis capabilities. The cells that make up the skin include keratinocytes, melanocytes, dendritic dells, and inflammatory cells like lymphocytes. The skin contains adnexal components that aid with homeostasis that including apocrine sweat glands, eccrine sweat glands, and hair follicles. The skin also contains sensory nerve fibers.
How Do I Describe Skin Lesions?
For macroscopic descriptions of skin lesions:
- Blister: A a vesicle or bulla.
- Bulla: A fluid-filled raised lesion greater than 5 mm across.
- Excoriation: A traumatic lesion characterized by breakage of the epidermis, leading to a raw linear area often self-induced.
- Lichenification: Prominent skin markings as a result of repeated rubbing in susceptible persons, the skin is thickened and rough.
- Macule: Flatness and usually distinguished from surrounding skin by its coloration circumscribed lesion of up to 5 mm in diameter.
- Nodule: A raised lesion with a spherical contour greater than 5 mm across.
- Onycholysis: Parting of the nail plate from the nail bed.
- Patch: A circumscribed lesion of more than 5 mm in diameter considered by its evenness and usually illustrious from surrounding skin by its coloring.
- Papule: Raised flat-topped or dome-shaped lesion measuring 5 mm or less across.
- Plaque: Elevated, greater than 5 mm across and flat-topped lesion.
- Pustule: A separate, pus-filled, elevated lesion.
- Scale: A result of imperfect cornification characterized by dry, horny, platelike excrescence.
- Vesicle: A fluid-filled raised lesion 5 mm or less across.
For microscopic descriptions of skin lesions:
- Acanthosis: A diffuse epidermal hyperplasia.
- Dyskeratosis: An atypical keratinization happening prematurely within individual cells or groups of cells below the stratum granulosum.
- Erosion: The discontinuity to the skin showing incomplete loss of the epidermis.
- Exocytosis: The penetration of the epidermis by inflammatory or circulating blood cells.
- Hydropic Swelling: Intracellular edema of keratinocytes, frequently in viral contagions.
- Hypergranulosis: Stratum granulosum hyperplasia, frequently due to concentrated rubbing.
- Hyperkeratosis: Stratum corneum thickening, linked to a qualitative abnormality of the keratin.
- Lentiginous: A linear pattern of melanocyte proliferation within the epidermal basal cell layer.
- Papillomatosis: The surface raise triggered by hyperplasia and amplification of contiguous dermal papillae.
- Parakeratosis: The means of keratinization branded by the retaining of the nuclei in the stratum corneum, normal on mucous membranes.
- Spongiosus: The intercellular edema of the epidermis.
- Ulceration: The discontinuity of the skin unveiling complete loss of the epidermis and frequently of portions of the dermis and subcutaneous fat.
- Vacuolization: The development of vacuoles in or next to cells, usually referring to the basal cell-basement membrane zone area.
What are Infections of the Skin?
Infections of the skin are disorders caused by the attack by microorganisms, parasites, and insects.
Examples of infections of the skin include:
- Impetigo
- Molluscum contagiosum
- Verrucae
- Scabies
- Tinea
- Lice
What is Impetigo?
Impetigo is a common superficial bacterial infection of the skin.
What is the Pathology of Impetigo?
The pathology of impetigo is:
-Etiology: The cause of impetigo is staphylococcus aureus most common and/or, streptococcus pyogenes.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to impetigo skin usually inhabited by opportunistic bacteria such as S. aureus and S. pyogenes which penetrate the skin, proliferate locally.
-Morphology: The morphology associated with impetigo shows a sub corneal pustule.
-Histology: The histology associated with impetigo shows the buildup of neutrophils beneath the stratum corneum.
How does Impetigo Present?
Patients with impetigo are typically more common in male children present at the age range of 2 to 5 years. The symptoms, features, and clinical findings associated with impetigo include erythematous macule, dry crusted, eczema, fatigue, fever, and diarrhea.
How is impetigo Diagnosed?
Impetigo is diagnosed through history and clinical appearance. Laboratory studies, bacterial culture, and sensitivity, and biopsy.
How Is Impetigo Treated?
Impetigo is treated through medical care, topical/ systemic antibiotic therapy.
What is the Prognosis of Impetigo?
The prognosis of impetigo is good. Has self-limiting of 2 to 3 weeks.
What is Molluscum Contagiosum?
Molluscum contagiosum is a typical, self-limited viral illness of the skin instigated by a pox virus.
What is the Pathology of Molluscum Contagiosum?
The pathology of molluscum contagiosum is the study of an illness caused by a poxvirus, usually spread through direct contact, amongst children and young adults.
-Etiology: The cause of molluscum contagiosum is the molluscum poxvirus.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to molluscum contagiosum involves direct contact.
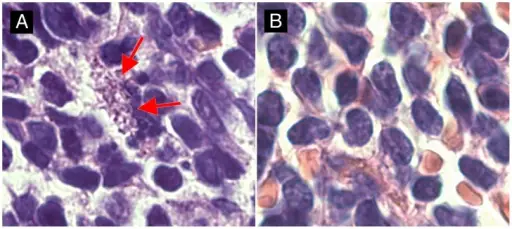
-Morphology: The morphology associated with molluscum contagiosum shows cup-shaped epidermis indentation into the dermis, acanthosis.
-Histology: The histology associated with molluscum contagiosum shows ellipsoid, homogeneous, cytoplasmic inclusion in cells eosinophilic and numerous virions.
How does Molluscum Contagiosum Present?
Patients with molluscum contagiosum typically affect more males than females present at an age range of 5 to 25 years. The symptoms, features, and clinical findings associated with molluscum contagiosum include tender or pruritic lesion, fever, malaise or nausea, atopic dermatitis.
How is Molluscum Contagiosum Diagnosed?
Molluscum contagiosum is diagnosed thorough medical history and physical examination, biopsy, laboratory work serum antibodies measure, tissue cultures neutralization. PRC detect molluscum contagiosum on the skin.
How is Molluscum Contagiosum Treated?
Molluscum contagiosum is treated by treating clinical presentations, curettage therapy, topical agents (cantharidin and tretinoin).
What is the Prognosis of Molluscum Contagiosum?
The prognosis of molluscum contagiosum is good. The condition is usually self-limited.
What is Verrucae Vulgaris?
Verrucae is a common lesion of children and adolescents, although they may be encountered at any age.
What is the Pathology of Verrucae?
The pathology of verrucae is:
-Etiology: The cause of verrucae is human papillomaviruses.
-Genes involved:
-Pathogenesis: The sequence of events that lead to verrucae; caused by various types of HPV viruses, different types of HPV not only have different morphologic lesions but also have variable oncogenic potential. Acquired through direct contact or autoinoculation. Usually undergo spontaneous regression.
-Morphology: The morphology associated with verrucae shows that it defers according to the type. gray white to tan, flat to convex for Verruca vulgaris. Flat, smooth, tan macules for verruca plana.
-Histology: The histology associated with verrucae shows epidermal hyperplasia, cytoplasmic vacuolization, numerous viral particles within nuclei, keratohyalin granules, and jagged eosinophilic intracytoplasmic keratin aggregates.
How does Verrucae Present?
Patients with verrucae typically has no gender prevalence, present at the age range of any age. The symptoms, features, and clinical findings associated with verrucae include multiple nodules, scaly lesions.
How is Verrucae Diagnosed?
Verrucae are diagnosed through clinical examination and physical findings. Laboratory studies; immunohistochemical detection for HPV structural proteins, PRC for viral DNA testing.
How is Verrucae Vulgaris Treated?
Verrucae are treated through treatment for symptoms, medical care topical agents, systemic antiviral, vitamin A derivatives, immunotherapy.
What is the Prognosis of Verrucae?
The prognosis is verrucae good.
What Is Scabies?
Scabies is a pruritic skin infestation caused by the host-specific mite Sarcoptes scabiei hominis.
What is the Pathology of Scabies?
The pathology of scabies is:
-Etiology: The cause of scabies is the mite Sarcoptes scabiei hominis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to scabies, caused by a mite. Mite does not penetrate more than stratum corneum layer. Transmission is by direct skin-to-skin contact.
-Morphology: The morphology associated with scabies shows nodular scabies, mites, ova, larvae, feces when burrow is executed.
-Histology: The histology associated with scabies shows dermal infiltrate by histiocytes, mast cells lymphocytes, and eosinophils.
How does Scabies Present?
Patients with scabies are typically more common in females present at the age range of 18 years and below. The symptoms, features, and clinical findings associated with scabies include rubbing and scratching grayish, threadlike elevations, erythematous vesicles, and papules.
How is Scabies Diagnosed?
Scabies is diagnosed is made clinically through history and physical examination, biopsy to rule out other dermatoses.
How is Scabies Treated?
Scabies is treated through medical therapy scabicidal agent (permethrin), antimicrobial agent, and proper hygiene for prevention.
What is the Prognosis of Scabies?
The prognosis of scabies is good owing to proper treatment and diagnosis with rare complications.
What is Tinea?
Tinea is a superficial fungal condition of the skin is limited to the stratum corneum, caused chiefly by dermatophytes Tinea capitis.
What is the Pathology of Tinea?
The pathology of tinea is:
-Etiology: The cause of tinea is dermatophytes.
-Genes involved:
-Pathogenesis: The sequence of events that lead to tinea involve invasion into keratinized tissue. They, persist and infect the stratum corneum of the epidermis, and hardly do they penetrate below beyond the epidermis.
-Morphology: The morphology associated with tinea shows variable features reliant on the organism antigenic properties, and the grade of bacterial superinfection.
-Histology: The histology associated with tinea shows eczematous dermatitis, stain bright pink to red mucopolysaccharides fungal cell walls.
How does Tinea Present?
Patients with tinea are typically more common in males present at an age range of any age. The symptoms, features, and clinical findings associated with tinea include symptomless, frequently hairless patches of skin, mild erythema, scale, crust formation.
How is Tinea Diagnosed?
Tinea is diagnosed through examination, microscopic examination, wood light (UV light) examination skin scraping, fungal culture, and biopsy.
How is Tinea Treated?
Tinea is treated through medical therapy antifungals, proper hygiene for prevention.
What is the Prognosis of Tinea?
The prognosis of tinea is good. Resolves without sequelae in 1-2 weeks of treatment.
What is Lice?
Lice is a skin infestation caused by a type of anthropods the louse.
What is the Pathology of Lice?
The pathology of lice is:
-Etiology: The cause of lice is P humanus capitis, P pubis, and P humanus corporis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to lice; bite from anthropoids cause lesion by the direct irritant effect of arthropods section, delayed or immediate hypersensitivity responses to retained/injected parts or secretions.
-Morphology: The morphology associated with lice shows urticarial or inflamed papules and nodules, with/without ulceration. May also serve as vectors for secondary invaders.
-Histology: The histology associated with lice shows infiltrate of lymphocytes, histiocytes, and eosinophils.
How does Lice Present?
Patients with lice are typically common in females than males present at an age range of 3 to 11. The symptoms, features, and clinical findings associated with lice include pruritus, louse, or its eggs, attached to hair shafts, trouble sleeping, and scratching.
How is Lice Diagnosed?
Lice is diagnosed through history and physical examination. Laboratory studies involve scrapings and fungal culture.
How is Lice Treated?
Lice is treated through medical care such as ovicidal pediculicides, environmental control, and hygiene for prevention.
What is the Prognosis of Lice?
The prognosis of lice is fair as treatment effective in killing the mature and nymphs lice but does not affect eggs associated with other comorbidities and social embarrassment.
What are Disorders of Epidermal Appendages?
Disorders of epidermal appendages are abnormalities of the skin epidermal layer and its components.
Examples of disorders of epidermal appendages include:
- Acne vulgaris
- Rosacea
What is Acne Vulgaris?
Acne vulgaris is a common chronic skin illness involving impasse or inflammation of pilosebaceous components.
What is the Pathology of Acne Vulgaris?
The pathology of acne vulgaris is:
-Etiology: The cause of acne vulgaris is a genetic predisposition, some cosmetic agents.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acne vulgaris is incompletely understood.
-Morphology: The morphology associated with acne vulgaris shows plug dense keratin dilated follicle, fibrosis, and scarring.
-Histology: The histology associated with acne vulgaris shows dense inflammatory infiltrate.
How does Acne Vulgaris Present?
Patients with acne vulgaris typically tend to be more in males than females present at an age range of 12 to 24. The symptoms, features, and clinical findings associated with acne vulgaris include open/closed noninflammatory comedones, nodules, and pustules.
How is Acne Vulgaris Diagnosed?
Acne vulgaris is diagnosed through physical examination, laboratory studies.
How is Acne Vulgaris Treated?
Acne vulgaris is treated through medical care include androgen receptor antagonists, retinoid, antimicrobial therapy, hormonal therapies. Surgical care intralesional steroid injections, light, and laser therapy.
What is the Prognosis of Acne Vulgaris?
The prognosis of acne vulgaris is good. Though may lead to long-lasting and detrimental psychosocial and physical effects
What is Rosacea?
Rosacea is the condition of the skin characterized by a spectrum of clinical signs and facial flushing.
What is the Pathology of Rosacea?
The pathology of rosacea is:
-Etiology: The cause of rosacea is corticosteroids uses, UV light exposure
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to rosacea are unknown.
-Morphology: The morphology associated with rosacea shows course skin, pustule, erythema.
-Histology: The histology associated with rosacea shows granulomatous inflammation, lymphohistiocytic infiltrate, and multinucleated cells.
How does Rosacea Present?
Patients with rosacea are typically common in males than females present at an age range of 12 to 24. The symptoms, features, and clinical findings associated with rosacea include facial flushing, erythema and telangiectasia, inflamed papules, and pustules.
How is Rosacea Diagnosed?
Rosacea is diagnosed through clinical examination and biopsy to role out cutaneous diseases.
How is Rosacea Treated?
Rosacea is treated through laser treatment, surgery, identification of deterrence.
What is the Prognosis of Rosacea?
The prognosis of rosacea is fair. Has chronic progressive course in some patients.
What are Disorders of Epidermal Maturation?
Disorders of epidermal maturation are disorders involving the development of the epidermal component.
Examples of disorders of epidermal maturation include:
- Ichthyosis
- Palmoplantar keratoderma
What is Ichthyosis?
Ichthyosis is a group of genetically inherited ailments associated with hyperkeratosis that result in clinically fishlike scales.
What is the Pathology of Ichthyosis?
The pathology of ichthyosis is:
-Etiology: The cause of ichthyosis is a genetic predisposition, connotation to lymphoid and visceral malignant.
-Genes involved: STS gene
-Pathogenesis: The sequence of events that lead to ichthyosis, abnormality resides in defective mechanisms of desquamation, causing the retention of abnormally formed scale.
-Morphology: The morphology associated with ichthyosis shows the prominent fishlike scales.
-Histology: The histology associated with ichthyosis shows the subtle build-up of compacted stratum corneum.
How does Ichthyosis Present?
Patients with ichthyosis are typically common in males than females present at an age range of 10 to 40 years. The symptoms, features, and clinical findings associated with ichthyosis include ocular/periocular manifestations, fine scales, varying degrees of skin dryness, scaling of trunk, legs, abdomen, and buttocks.
How is Ichthyosis Diagnosed?
Ichthyosis is diagnosed through laboratory studies-skin biopsy, CBC count, TFTs.
How is Ichthyosis Treated?
Ichthyosis is treated through medical care which includes systemic therapy oral retinoids, ocular therapy, topical therapy cyclosporine.
What is the Prognosis of Ichthyosis?
The prognosis of ichthyosis is fair.
What is Palmoplantar keratoderma?
Palmoplantar keratoderma is an assorted group of ailments branded by persistent epidermal thickening to the palms and soles skin.
What is the Pathology of Palmoplantar keratoderma?
The pathology of palmoplantar keratoderma is:
-Etiology: The cause of palmoplantar keratoderma is inherited or acquired allied to internal malignancy.
-Genes involved: AAGAB gene
-Pathogenesis: The sequence of events that lead to palmoplantar keratoderma is unknown.
-Morphology: The morphology associated with palmoplantar keratoderma shows epidermal thickening to the palms and soles skin.
-Histology: Acanthosis.
How does Palmoplantar Keratoderma Present?
Patients with palmoplantar keratoderma typically have unknown prevalence The symptoms, features, and clinical findings associated with palmoplantar keratoderma include multiple hyperkeratotic papules, lesions on the palm and soles, pain pressure point.
How is Palmoplantar Keratoderma Diagnosed?
Palmoplantar keratoderma is diagnosed based on a grouping of clinical and histopathologic features and also genetic testing.
How is Palmoplantar Keratoderma Treated?
Palmoplantar keratoderma is treated through the management of the underlying conditions and stopping likely triggers.
What is the Prognosis of Palmoplantar Keratoderma?
The prognosis of palmoplantar keratoderma is good.
What are Acute Inflammatory Dermatoses?
Acute inflammatory dermatoses is the sudden onset swelling, pain, redness, and hotness or the skin dermis mediated by local or systemic immunologic factors, although the causes for many remain a mystery.
Examples of acute inflammatory dermatoses include:
- Acute eczematous dermatitis
- Erythema multiforme
- Urticaria
What is Acute Eczematous Dermatitis?
Acute eczematous dermatitis is the pathogenetically different conditions branded by red, oozing, papulovesicular, and crusted lesions early, with persistence, developing into elevated, scaling plaque.
What is the Pathology of Eczematous Dermatitis?
The pathology of eczematous dermatitis is:
-Etiology: The cause of eczematous dermatitis is inherited other factors illness from contact with an external antigen.
-Genes involved: CARD11 gene
-Pathogenesis: The sequence of events that lead to eczematous dermatitis, antigens at the epidermal surface, are taken by dendritic Langerhans cells, which then migrate via dermal lymphatics to draining lymph nodes.
-Morphology: The morphology associated with eczematous dermatitis shows numerous vesicles appearing at the spot of antigen exposure.
-Histology: The histology associated with eczematous dermatitis shows widened intercellular spaces in the epidermis, ultimately leading to small, fluid-filled vesicles.
How does Eczematous Dermatitis Present?
Patients with eczematous dermatitis are typically more common in females than males present at an age range of 5 years. The symptoms, features, and clinical findings associated with eczematous dermatitis include itchy, edematous, oozing plaques, frequently containing vesicles and bullae.
How is Eczematous Dermatitis Diagnosed?
Eczematous dermatitis is diagnosed through a medical history, physical examination, laboratory studies.
How is Eczematous Dermatitis Treated?
Eczematous dermatitis is treated through medical care with topical steroids.
What is the Prognosis of Eczematous Dermatitis?
The prognosis of eczematous dermatitis is good.
What is Erythema Multiforme?
Erythema multiforme is an uncommon, usually self-limited disorder that appears to be a hypersensitivity response to certain infections and drugs.
What is the Pathology of Erythema Multiforme?
The pathology of erythema multiforme is:
-Etiology: The cause of erythema multiforme is herpes virus (HSV), drug hypersensitivity, contact exposure.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to erythema multiforme are multifactorial.
-Morphology: The morphology associated with erythema multiforme shows a characteristic “targetoid” or “bulls eye”appearance.
-Histology: The histology associated with erythema multiforme shows superficial perivascular, lymphocytic infiltrate.
How does Erythema Multiforme Present?
Erythema multiforme typically affects more males than females present at an age range of 5 to 45 years. The symptoms, features, and clinical findings associated with erythema multiforme include nonspecific URTI, and sudden onset of a rash.
How is Erythema Multiforme Diagnosed?
Erythema multiforme is diagnosed with clinical examination and history taking. Laboratory studies- CBC count with moderate leukocytosis, BUN, and creatinine test, immunofluorescence, PCR, biopsy.
How is Erythema Multiforme Treated?
Erythema multiforme is treated through medical care- symptomatic management, oral, analgesics, antihistamines local skincare, soothing mouthwashes, rehydration, and nutrition support. Pulmonary support according to severity.
What is the Prognosis of Erythema Multiforme?
The prognosis of erythema multiforme is good the condition is self-limiting.
What is Urticaria?
Urticaria is a common ailment of the skin localized mast cell degranulation and subsequent dermal microvascular hyperpermeability, ending in pruritic edematous plaques (wheals).
What is the Pathology of Urticaria?
The pathology of urticaria is:
-Etiology: The cause of urticaria is an infection, allergen, some drugs, exposure to latex, pregnancy, idiopathic.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to urticaria; results from the antigen-induced release of vasoactive mediators from mast cell granules via sensitization with specific immunoglobulin E (IgE) antibodies following the exposure.
-Morphology: The morphology associated with urticaria shows lesions varying from trivial, pruritic papules to big edematous plaques.
-Histology: The histology associated with urticaria shows sparse superficial perivenular infiltrate of mononuclear cells rare neutrophils and eosinophils.
How does Urticaria Present?
Patients with urticaria typically slightly more common in males than females present at an age range of 20 to 40 years. The symptoms, features, and clinical findings associated with urticaria include usually lesions fading within hours, palpable wheals small, pruritic papules, and large erythematous plaques.
How is Urticaria Diagnosed?
Urticaria is diagnosed through the clinical presentation, laboratory studies, CBC count, ESR, antinuclear antibody (ANA), and thyroid-stimulating hormone (TSH), and biopsy.
How is Urticaria Treated?
Urticaria is treated through the systemic management of symptoms.
What is the Prognosis of Urticaria?
The prognosis of urticaria is good for acute urticaria as it is self-limiting.
What are Chronic Inflammatory Dermatoses?
Chronic inflammatory dermatoses are tenacious skin conditions that exhibit their most characteristic features for a long time months to years.
Examples of chronic inflammatory dermatoses include:
- Lichen planus
- Psoriasis
- Seborrheic dermatitis
- Hidradenitis suppurativa
What is Lichen Planus?
Lichen planus is a disorder of the skin and mucous membrane characterized by pruritic, purple, polygonal papules.
What is the Pathology of Lichen Planus?
The pathology of lichen planus is:
-Etiology: The cause of lichen planus is idiopathic, immunologically mediated.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to lichen planus is unknown.
-Morphology: The morphology associated with lichen planus shows a flat-topped pink-purple, polygonal papule.
-Histology: The histology associated with lichen planus shows a bandlike infiltrate of lymphocytes at the dermo-epidermal junction.
How does Lichen Planus Present?
Patients with lichen planus typically have no gender prevalence present at an age range of 30 to 60 years. The symptoms, features, and clinical findings associated with lichen planus include pruritus, oral lesions, lesions on flexural surfaces.
How is Lichen Planus Diagnosed?
Lichen planus is diagnosed through the clinical presentation, laboratory studies- direct immunofluorescence study reveals globular deposits of IgM and biopsy.
How is Lichen Planus Treated?
Lichen planus is treated through medical care for symptoms, fluorinated topical steroids, antimicrobial.
What is the Prognosis of Lichen Planus?
The prognosis of lichen planus is good most symptoms regress in 2 years period.
What is Psoriasis?
Psoriasis is a complex, chronic, inflammatory, multifactorial disease involving keratinocytes’ hyperproliferation of the epidermis, with an upsurge in the epidermal cell turnover rate.
What is the Pathology of Psoriasis?
The pathology of psoriasis is:
-Etiology: The cause of psoriasis is a genetic predisposition, immunologic factors.
-Genes involved: HLA-Cw*0602 allele, LCE3C, and LCE3B, genes.
-Pathogenesis: The sequence of events that lead to psoriasis: CD4+ T cells pledge the illness in cooperating with the skin antigen-presenting cells, signaling activation of CD8+ T cells at the epidermis. Interactions amid CD4+ T cells, CD8+ T cells, dendritic cells, and keratinocytes result in a cytokine “soup” dominated by TH1 type cytokines IL-12, IFN-γ, and TNF. Infiltrated lymphocytes too produce growth factors for keratinocytes.
-Morphology: The morphology associated with psoriasis shows a noticeable epidermal thickening, with downward elongation of the rete ridges.
-Histology: The histology associated with psoriasis shows parakeratosis, regular acanthosis to the epidermis.
How does Psoriasis Present?
Patients with psoriasis are typically more common in females than males present at an age range of 20 to 30 years. The symptoms, features, and clinical findings associated with psoriasis include pain, afebrile, pruritus rash, silvery raised inflamed lesions, salmon-pink papules. Blepharitis ocular manifestation.
How is Psoriasis Diagnosed?
Psoriasis is diagnosed through the clinical presentation, laboratory studies, rheumatoid factor test usually negative, ESR, uric acid levels.
How is Psoriasis Treated?
Psoriasis is treated through medical care- topical and systemic medication, climatotherapy, stress reduction, phototherapy, and moisturizers, ocular lubricants, and surgical treatment.
What is the Prognosis of Psoriasis?
The prognosis of psoriasis is fair. It is a benign, lifelong ailment with remissions and aggravations and at times refractory to management.
What is Seborrheic Dermatitis?
Seborrheic dermatitis is a disorder of papulosquamous patterned on the areas of the scalp, face, and trunk with sebum-rich.
What is the Pathology of Seborrheic Dermatitis?
The pathology of seborrheic dermatitis is:
-Etiology: The cause of seborrheic dermatitis is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to seborrheic dermatitis is unknown.
-Morphology: The morphology associated with seborrheic dermatitis shows scaling over red, inflamed skin.
-Histology: The histology associated with seborrheic dermatitis shows parakeratosis containing neutrophils and serum.
How does Seborrheic Dermatitis Present?
Patients with seborrheic dermatitis are typically more common in males than females present at an age range of 40 years. The symptoms, features, and clinical findings associated with seborrheic dermatitis include burning, scaling, itching, candidal overgrowth, and blepharitis.
How is Seborrheic Dermatitis Diagnosed?
Seborrheic dermatitis is diagnosed based on clinical presentations, laboratory studies of the skin biopsy.
How is Seborrheic Dermatitis Treated?
Seborrheic dermatitis is treated through with topical corticosteroids, antifungal, and shampooing.
What is the Prognosis of Seborrheic Dermatitis?
The prognosis of seborrheic dermatitis is good.
What is Hidradenitis Suppurativa?
Hidradenitis suppurativa is an ailment of the terminal follicular epithelium in the skin.
What is the Pathology of Hidradenitis Suppurativa?
The pathology of hidradenitis suppurativa is:
-Etiology: The cause of hidradenitis suppurativa is idiopathic.
-Genes involved: Gamma-secretase genes PSENEN, PSEN1, and NCSTN.
-Pathogenesis: The sequence of events that lead to hidradenitis suppurativa is not clearly understood.
-Morphology: The morphology associated with hidradenitis suppurativa shows the incidence of typical skin microbiota.
-Histology: The histology associated with hidradenitis suppurativa shows infundibulum hyperkeratosis.
How does Hidradenitis Suppurativa Present?
Patients with hidradenitis suppurativa typically more in females than males present at an age range of 11 to 50 years. The symptoms, features, and clinical findings associated with hidradenitis suppurativa include chronic inflammation, follicular occlusion, progressive scarring, and mucopurulent discharge.
How is Hidradenitis Suppurativa Diagnosed?
Hidradenitis suppurativa is diagnosed through the clinical presentation. Laboratory studies- CBC count, C-reactive protein assay, serum multiphasic analysis. Imaging studies- dermal and hair follicles ultrasonography.
How is Hidradenitis Suppurativa Treated?
Hidradenitis suppurativa is treated through medical care anti-inflammatory/antiandrogen therapy, biological therapy, smoking cessation, and warm compresses.
What is the Prognosis of Hidradenitis Suppurativa?
The prognosis of hidradenitis suppurativa is fair.
What is Panniculitis?
Panniculitis is the inflammatory response in the subcutaneous fat affecting.
Examples of panniculitis include:
- Erythema induratum
- Erythema nodosum
What is Erythema Induratum?
Erythema Induratum is an uncommon type of panniculitis affecting principally menopausal women and adolescents.
What is the Pathology of Erythema Induratum?
The pathology of erythema induratum is:
-Etiology: The cause of erythema induratum is unknown though associated with vasculitis affecting deep vessels.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to erythema induratum not well understood.
-Morphology: The morphology associated with erythema induratum shows necrotizing vasculitis affecting the deep dermis and subcutis arteries and veins.
-Histology: The histology associated with erythema induratum shows granulomatous inflammation, zones of caseous necrosis involving fat lobule.
How does Erythema Induratum Present?
Patients with erythema induratum typically common in females than males present at age range of 13 to 60 years. The symptoms, features, and clinical findings associated with erythema induratum include tender, erythematous nodules on lower limbs.
How is Erythema Induratum Diagnosed?
Erythema Induratum is diagnosed through the clinical presentation, laboratory studies-such as LFTs, ESR, Hepatitis C virus serology, CBC count, PCR for detection of M tuberculosis.
How is Erythema Induratum Treated?
Erythema induratum is treated through medical management of underlying symptoms nonsteroidal anti-inflammatory, potassium iodide, and tetracyclines.
What is the Prognosis of Erythema Induratum?
The prognosis of erythema induratum is good under proper treatment and management.
What is Erythema Nodosum?
Erythema nodosum is an acute, nodular, erythematous eruption typically limited to the lower legs extensor surfaces.
What is the Pathology of Erythema Nodosum?
The pathology of erythema nodosum is:
-Etiology: The cause of erythema nodosum is associated with infections tuberculosis, beta-hemolytic streptococcal infection, coccidioidomycosis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to erythema nodosum is not well understood, believed to result from a delayed hypersensitivity response to antigens.
-Morphology: The morphology associated with erythema nodosum shows edema, fibrin exudation.
-Histology: The histology associated with erythema nodosum shows infiltration by, multinucleated giant cells, lymphocytes, eosinophils, histiocytes, and septal fibrosis.
How does Erythema Nodosum Present?
Patients with erythema nodosum are typically more common in females than males present at an age range of 18 to 34 years. The symptoms, features, and clinical findings associated with erythema nodosum include exquisitely tender, nodules, and erythematous plaques of the lower limbs.
How is Erythema Nodosum Diagnosed?
Erythema nodosum is diagnosed through the clinical presentation, and laboratory studies.
How is Erythema Nodosum Treated?
Erythema nodosum is treated through medical management of the symptoms, nonsteroidal anti-inflammatory drugs, wet compresses.
What is the Prognosis of Erythema Nodosum?
The prognosis of erythema nodosum is good.
What are Premalignant and Malignant Epidermal Tumors?
Premalignant and malignant epidermal tumors:
- Actinic keratosis
- Basal cell carcinoma
- Squamous cell carcinoma
What is Actinic Keratosis?
Actinic keratosis is a UV light-induced anomaly of the skin capable of progressing to invasive squamous cell carcinoma.
What is the Pathology of Actinic Keratosis?
The pathology of actinic keratosis is:
-Etiology: The cause of actinic keratosis is chronic exposure to sunlight.
-Genes involved: TP53 gene.
-Pathogenesis: The sequence of events that lead to actinic keratosis relates to collective UV exposure. Consequently, the incidence of actinic keratosis surges with each decade of life.
-Morphology: The morphology associated with actinic keratosis shows < 1 cm in diameter, tan-brown, red, or skin-colored, a rough, sandpaper-like consistency.
-Histology: The histology associated with actinic keratosis shows atypia epidermis, hyperplasia of basal cells, dyskeratosis with pink cytoplasm.
How does Actinic Keratosis Present?
Patients with actinic keratosis are typically common in males than females present at an age range of 20 to 30 years. The symptoms, features, and clinical findings associated with actinic keratosis include red and scaly rough spots.
How is Actinic Keratosis Diagnosed?
Actinic keratosis is diagnosed through a skin biopsy, corfim diagnosis and used to rule out squamous cell carcinoma. Fluorescence, with a photosensitizing drug.
How is Actinic Keratosis Treated?
Actinic keratosis is treated through medical therapy such as imiquimod cream.
What is the Prognosis of Actinic Keratosis?
The prognosis of actinic keratosis is good. With proper treatment, it can be successfully managed.
What is Basal Cell Carcinoma?
Basal cell carcinoma is a nonmelanocytic skin tumor arising from basal cells.
What is the Pathology of Basal Cell Carcinoma?
The pathology of basal cell carcinoma is:
-Etiology: The cause of basal cell carcinoma is radiation exposure, gene mutations, immunosuppression, idiopathic.
-Genes involved: TP53 gene.
-Pathogenesis: The sequence of events that lead to basal cell carcinoma are due to pluripotential cells of the basal layer of the epidermis/follicular that are abnormal.
-Morphology: The morphology associated with basal cell carcinoma shows a scale, erythema, and a threadlike raised border.
-Histology: The histology associated with basal cell carcinoma shows large, hyperchromatic, little cytoplasm, and oval nuclei basalioma cells.
How does Basal Cell Carcinoma Present?
Patients with basal cell carcinoma typically common in males present at an age range of 55-70 years. The symptoms, features, and clinical findings associated with basal cell carcinoma include slowly widening lesions, waxy papules, ulceration, with crusting that bleed when injured.
How is Basal Cell Carcinoma Diagnosed?
Basal cell carcinoma is diagnosed through the clinical presentation.
How is Basal Cell Carcinoma Treated?
Basal cell carcinoma is treated through surgery, chemotherapeutic.
What is the Prognosis of Basal Cell Carcinoma?
The prognosis of basal cell carcinoma is good with a 100% survival rate for those that have not spread.
What is Squamous Cell Carcinoma?
Squamous cell carcinoma is the 2nd most common type of cancer that arises from the skin that is caused by fast-growing squamous cells.
What is the Pathology of Squamous Cell Carcinoma?
The pathology of squamous cell carcinoma is the study of the cancerous tumor that arises from the skin of the squamous cells.
-Etiology: The cause of squamous cell carcinoma is: exposure to sunlight, altered immune system,
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma are caused by alteration of the normal gene structure by exposure to UV light. Alteration of this gene cause build-up of cells instead of the normal process of apoptosis. This accumulation causes squamous cell carcinoma.
-Morphology: The morphology associated with squamous cell carcinoma shows rough, scaly red patches, open sores with wart-like patterns, and has irregular borders.
-Histology: The histology associated with squamous cell carcinoma shows nests of squamous cells extending to the dermis from the epidermis. Large abundant eosinophilic cytoplasm and a large vesicular nucleus.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically are male than female. The symptoms, features, and clinical findings associated with squamous cell carcinoma include easily bleeding to touch, has irregular borders, has rapid growth, dome-shaped bump,
How is Squamous Cell Carcinoma Diagnosed?
The small cell carcinoma is diagnosed through history taking and physical examination.
How is Squamous Cell Carcinoma Treated?
The squamous cell carcinoma is treated by surgery depending on where it has spread to then curettage and electro dissection, laser therapy, photodynamic therapy, and cryosurgery.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of squamous cell carcinoma is good since it can be treated through the necessary surgery and it can be detected early.
What are Disorders of Pigmentation and Melanocytes?
Examples of Disorders of Pigmentation and Melanocytes include:
- Freckles
- Lentigo
- Melanocytic nevi
- Melanoma
What are Freckles?
Freckles are also known as ephelis this are groups of pigmented cells found on the skin.
What is the Pathology of Freckles?
The pathology of freckles is:
-Etiology: The cause of ephelis exposure to the sun.
-Genes involved: MC1R gene.
-Pathogenesis: The sequence of events that lead to freckles is due to the increased production of melanin that is caused by UV-B radiation. This makes the areas affected become darker and more visible.
-Morphology: The morphology associated with freckles shows small dark brown patches in cluster form.
-Histology: The histology associated with freckles shows increased melanin pigments within the basilar epidermis but the melanocytes are not increased.
How does Freckles Present?
Patients with freckles typically present in childhood adolescence and young adulthood age and are mostly female than males. The symptoms, features, and clinical findings associated with freckles include itching, redness, swelling, peeling, and at times infection.
How is Freckles Diagnosed?
Freckles are diagnosed by physical exam and history taking.
How are Freckles Treated?
The Freckles are treated by avoiding direct sunlight, and topical medication, light cryosurgery.
What is the Prognosis of Freckles?
The prognosis of freckles is good since they often respond to medication and they are not malignant.
What is Lentigo?
Lentigo is a small sharply circumscribed pigmented macule surrounded by normal appearing skin.
What is the Pathology of Lentigo?
The pathology of lentigo is:
-Etiology: The cause of lentigo is dependent on the cause it can be solar lentigo, radiation lentigo and can be caused by genetic factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to lentigo is dependent on the cause in the solar lentigo. The UV light causes overproduction of melanin and the production of abnormal pigment retention.
-Morphology: The morphology associated with lentigo shows irregular or regular shaped macule that is darker in color than the normal skin color.
-Histology: The histology associated with lentigo shows increased basal melanin, increased number of melanocytes elongation of the rete ridges.
How does Lentigo Present?
Patients with lentigo are typically more common in males than in females and can be found in both children and adults. The symptoms, features, and clinical findings associated with lentigo include painless, redness at times.
How is Lentigo Diagnosed?
The lentigo is diagnosed physical exam and history taking examination with a wood lamp.
How is Lentigo Treated?
The lentigo is treated topical medication, cryosurgery, laser surgery.
What is the Prognosis of Lentigo?
The prognosis of lentigo is good.
What are Melanocytic Nevi?
Melanocytic nevi are the cancer of the melanocytes either congenital or acquired.
Examples of melanocytic nevi include:
- Congenital nevus
- Blue nevus
- Spitz nevus
- Halo nevus
- Dysplastic nevus
What is Congenital Nevus?
Congenital Nevus is a benign neoplasm of the melanocytes which one is born with aka birthmark
What is the Pathology of Congenital Nevus?
The pathology of congenital nevus is: the study of the diseases of the melanocyte that are not cancerous in nature.
-Etiology: The cause of congenital nevus is a genetic mutation.
-Genes involved: NRAS, BRAF genes.
-Pathogenesis: The sequence of events that lead to congenital nevus is as conception is taking place there is the proliferation of the melanocytes which are benign either from the dermis, epidermis, or both. They may be present after birth or can be seen during the 1st 2years of life.
-Morphology: The morphology associated with congenital nevus shows either round or oval with well-marked boundaries and can be smooth. Texture can be rugose, cerebriform of popular.
-Histology: The histology associated with congenital nevus show an extension of naevus cells around nerves, vessels, and adnexa. There is a diffusely infiltrative pattern between collagen.
How does Congenital Nevus Present?
Patients with congenital nevus typically are of both genders occurring at birth. The symptoms, features, and clinical findings associated with congenital nevus include hypopigmentation.
How is Congenital Nevus Diagnosed?
This congenital nevus is diagnosed by shave biopsy, punch biopsy, or excisional biopsy.
How is Congenital Nevus Treated?
This congenital nevus is treated if only it is suspected to be cancerous. Shave biopsy is recommended if one does not accept how it looks.
What is the Prognosis of Congenital Nevus?
The prognosis of congenital nevus is good since it is rarely found to be cancerous.
What is Blue Nevus?
Blue nevus is a type of mole that is blue and can be congenital or acquired.
What is the Pathology of Blue Nevus?
The pathology of blue nevus is the study of the pathology and the histology of the proliferation of melanocytes.
-Etiology: The cause of blue nevus is not so clear but is believed to be caused by a lack of melanocytes to reach the dermis.
-Genes involved: BRAF and NRAS genes.
-Pathogenesis: The sequence of events that lead to blue nevus is believed that during development the melanocytes fail to reach the epidermis and get stuck below the epidermis.
-Morphology: The morphology associated with blue nevus shows a uniform nucleus, large and round pale cytoplasm.
-Histology: The histology associated with blue nevus shows melanocytes that have a reduced amount of melanin, thickened collagen that is found in the dendritic spindles.
How does Blue Nevus Present?
Patients with blue nevus typically are common in women than in males and can occur at any stage of life but mostly in the second decade. The symptoms, features, and clinical findings associated with blue nevus include small, round raised blue-colored and can be from 1-5 millimeters.
How is Blue Nevus Diagnosed?
This blue nevus is diagnosed by physical examination since it can be seen on the skin due to its blue appearance. Dermatoscopy is done in case one wants more information.
How is Blue Nevus Treated?
The blue nevus may be surgically removed.
What is the Prognosis of Blue Nevus?
The prognosis of blue nevus is good because the rarely becomes cancerous.
What is Spitz Nevus?
Spitz nevus is a skin lesion that mostly affects children and the young generation.
What is the Pathology of Spitz Nevus?
The pathology of the study of skin disease with the aim to identify the cause of the pathology and the histology of the disease.
-Etiology: The cause of spitz nevus is currently unknown.
-Genes involved: BAP1 and BRAF.
-Pathogenesis: The sequence of events that lead to spitz nevus is melanoocytic proliferation.
-Morphology: The morphology associated with spitz nevus shows pigmented bands symmetrically spread at the lesion margin.
-Histology: The histology associated with spitz nevus shows nests containing spindle-shaped and epithelioid cells. Have abundant cytoplasm with conspicuous nucleoli.
How does Spitz Nevus Present?
Patients with spitz nevus are typically more female than the male with a mean age of 22 years and mostly in the lower extremity. The symptoms, features, and clinical findings associated with spitz nevus include solitary symmetrical well-circumscribed, pink pigmented dome-shaped papule.
How is Spitz Nevus Diagnosed?
The spitz nevus is diagnosed by physical examination and by the use of a dermatoscope.
How is Spitz Nevus Treated?
The spitz nevus is treated by surgical removal or excision but the doctors recommends frequent monitoring before removal.
What is the Prognosis of Spitz Nevus?
The prognosis of spitz nevus is good. His is because the lesion is mostly benign.
What is Halo Nevus?
Halo nevus is a skin lesion or papule surrounded by a white ring aka sutton’s nevus.
What is the Pathology of Halo Nevus?
The pathology of halo nevus is:
-Etiology: The cause of halo nevus is not clearly stated but it is believed to have been caused by an autoimmune response against the melanocytes.
-Genes involved: HLA-DBR1.
-Pathogenesis: The sequence of events that lead to halo nevus starts first by the presence of a pink papule which later the immune system recognizes as foreign and is attacked by the defense system of the body hence the presence of the white appearance.
-Morphology: The morphology associated with halo nevus shows a region of depigmentation surrounding the nevus.
-Histology: The histology associated with halo nevus shows papillary dermis is infiltrated by the dense lymphoid infiltrates.
How does Halo Nevus Present?
Patients with halo nevus typically are of both gender with an average age of 15 years.
The symptoms, features, and clinical findings associated with halo nevus include uniform color, evenly shaped with hypopigmentation, with clear boundaries. The central nevus is pink, or brown.
How is Halo Nevus Diagnosed?
The halo nevus is diagnosed through physical examination, shave biopsy, and punch biopsy.
How is Halo Nevus Treated?
The halo nevus is treated by application of sunscreen if that is the cause but in general, it does not need any treatment.
What is the Prognosis of Halo Nevus?
The prognosis of halo nevus is good since in most cases all are benign.
What is Dysplastic Nevus?
Dysplastic Nevus is a form of atypical nevi that is larger and has an irregular shape than the other moles.
What is the Pathology of Dysplastic Nevus?
The pathology of halo nevi is the study of the lesion of the skin and how to manage it and its diagnosis.
-Etiology: The cause of dysplastic nevus is not well understood but those with the FAMMM syndrome are at a higher risk of having this condition.
-Genes involved: IRF4, MTAP, PLA2G6, CDK2NA, CDK4.
-Pathogenesis: The sequence of events that lead to dysplastic nevus: can be hereditary or sporadic. A prescribed genetic study has proposed an autosomal dominant mode of heirloom.
-Morphology: The morphology associated with dysplastic nevus shows asymmetry with irregular borders, varying in color and more than 5 mm.
-Histology: The histology associated with dysplastic nevus shows cytologic atypia, nevi cells are enlarged, nests are adjacent to each other.
How does Dysplastic Nevus Present?
Patients with dysplastic nevus typically do not vary in gender but in age, it occurs mostly in childhood but the latest ii can be seen is at the end of puberty. The symptoms, features, and clinical findings associated with dysplastic nevus include large pigmented lesions which are asymmetrical with irregular borders and can arrange from tan to dark color.
How is Dysplastic Nevus Diagnosed?
The dysplastic nevus is diagnosed dermoscopy and biopsy.
How is Dysplastic Nevus Treated?
The dysplastic nevus is treated due to the high risk of becoming g cancerous surgical removal, use of broad-spectrum sunscreen.
What is the Prognosis of Dysplastic Nevus?
The prognosis of dysplastic nevus is good but there is a need for continuous monitoring mostly in those who have the FAMMM syndrome to avoid chances of it becoming malignant.
What is Melanoma?
Melanoma is a tumor or a mass on the skin that occurs as a result of an increase or change in the proliferation of the melanocytes.
What is the Pathology of Melanoma?
The pathology of melanoma is the scientific study of the factors that lead to the formation of skin lesions and how to manage the abnormality.
-Etiology: The cause of melanoma is hereditary factors, extreme exposure to the sun, personal factors like blue eyes, socioeconomic status.
-Genes involved: CDKN2A, MC1R.
-Pathogenesis: The sequence of events that lead to melanoma occurs when the normal pathway the case new cells to regrow and the old ones to die if affected. The actors that damage this process include exposure to UV light, hereditary factors, and environmental factors.
-Morphology: The morphology associated with melanoma shows the presence of malignant cells, atypia, increased mitoses, and nucleoli in an increased amount.
-Histology: The histology associated with melanoma shows localized nodular proliferation of benign-appearing fibroblasts within the dermis.
How does Melanoma Present?
Patients with melanoma typically are those in their fourth decade of life and can affect any gender. The symptoms, features, and clinical findings associated with melanoma include asymmetrical, irregular borders, color variation esp. white, the red and blue larger diameter of more than 6 mm, and elevated surface.
How is Melanoma Diagnosed?
The melanoma is diagnosed by a biopsy, physical examination.
How is Melanoma Treated?
The melanoma is treated will depend on the size of the melanoma. It can be immunotherapy, targeted therapy and surgical removal.
What is the Prognosis of Melanoma?
The prognosis of melanoma is good only if detected early since the melanomas are highly cancerous.
What are Benign Epithelial Tumors?
Benign Epithelial Tumors are non-cancerous tumors arising from the epithelium.
Examples of Benign Epithelial Tumors include:
- Acanthosis nigricans
- Follicular Inclusion Cyst (Wen)
What is Acanthosis Nigricans?
Acanthosis nigricans is an example of a cutaneous syndrome characterized by the presence of dark discoloration in the body fold and in the body creases and skin thickening.
What is the Pathology of Acanthosis Nigricans?
The pathology of acanthosis nigricans is:
-Etiology: The cause of acanthosis nigricans is due to dysfunction of the growth factors mostly those of the endocrine system, which can be obesity-associated, hormonal changes, medication, genetics.
-Genes involved: FGFR3 gene.
-Pathogenesis: The sequence of events that lead to acanthosis nigricans is due to the increased activation of growth factors receptor proteins
-Morphology: The morphology associated with acanthosis nigricans shows thick skin that is dark in color.
-Histology: The histology associated with acanthosis nigricans shows an increased number of squamous cells upon microscopy viewing.
How does Acanthosis Nigricans Present?
Patients with acanthosis nigricans typically are both male and female. The age range is general but may occur mostly at the adult age and can occur in children with underlying conditions. The symptoms, features, and clinical findings associated with acanthosis nigricans include hyperpigmentation, hyperkeratosis, excessive roughness, dryness, and itching.
How is Acanthosis Nigricans Diagnosed?
The acanthosis nigricans is diagnosed mainly by physical examination and at some point, a sale of the blood is taken to the ab for further exploration.
How is Acanthosis Nigricans Treated?
Acanthosis nigricans is treated by managing the underlying causes e.g. weight loss, hormonal stabilization, management of diabetes, and treatment of cancer.
What is the Prognosis of Acanthosis Nigricans?
The prognosis of acanthosis nigricans is poor if it is a malignant form with an average survival rate of 2 years.
What is Epithelial or Follicular Inclusion Cyst (Wen)?
Epithelial or follicular inclusion cyst (Wen) is a type of non-cancerous growth that occurs on parts of the skin with minimal hair and occurs as a result of the epidermis embedding itself into the dermis.
What is the Pathology of Follicular Inclusion Cyst?
The pathology of follicular inclusion cyst is: the study of the conditions of the skin mostly the squamous epithelium and outlining the histology and the pathology of the disease.
-Etiology: follicular inclusion cyst is trauma, infection, blockage leading to misplacement of the epidermis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to follicular inclusion cyst occurs as a result of the increased production of the epidermal cells in the location of the dermis.
-Morphology: The morphology associated with follicular inclusion cyst shows dome-shaped lumps filled with keratin, mobile, and a size ranging from 0.5 cm.
-Histology: The histology associated with follicular inclusion cyst shows a thin layer of squamous epithelium.
How does Follicular Inclusion Cyst Present?
Patients with follicular inclusion cysts are typically more common in males than females, present at an age range of 20-60 years. The symptoms, features, and clinical findings associated with follicular inclusion cyst include small round swelling under the skin, redness, and tenderness if infected, thick foul-smelling yellow discharge may be seen.
How is Follicular Inclusion Cyst Diagnosed?
The follicular inclusion cyst is diagnosed palpation, physical examination, and needle biopsy.
How is Follicular Inclusion Cyst Treated?
The follicular inclusion cyst is treated by incision and drainage of the cyst to remove the contents inside and also to some extent there is the injection of steroid medication.
What is the Prognosis of Follicular Inclusion Cyst?
The prognosis of follicular inclusion cyst is good.
What are Adnexal Tumors?
Adnexal Tumors are tumors that arise from the structures that hold main organs in place.
Examples of adnexal tumors include:
- Cylindroma
- Eccrine Poroma
- Pilomatricoma
- Sebaceous Adenoma
- Syringomas
What is a Cylindroma?
Cylindroma is also known as the turban tumor. It is a tumor arising from the apocrine sweat gland of the skin and is benign.
What is the Pathology of Cylindroma?
The pathology of cylindroma is the study of the disease that affects the apocrine sweat glands found in the human skin.
-Etiology: The cause of cylindroma is lack of the CYLD gene.
-Genes involved: MYB-NFIB, CYLD genes.
-Pathogenesis: The sequence of events that lead to cylindroma; cellular cause of cylindromas is unknown.
-Morphology: The morphology associated with cylindroma shows around like shape hence the name cylindroma, pink in color.
-Histology: The histology associated with cylindroma shows ductal cells with large pale nuclei and also undifferentiated peripheral epithelial cells with small dark nuclei, hyaline droplets, and tumor lobule nests.
How does Cylindroma Present?
Patients with cylindroma typically are more common in females than in males and affect the middle-aged and the elderly persons and can increase in number as one grows older. The symptoms, features, and clinical findings associated with cylindroma include slow-growing, painful and may be multiple or single.
How is Cylindroma Diagnosed?
The cylindroma is diagnosed by physical examination, use of a dermatoscope, skin biopsy, and genetic test to test the mutation of the CYLD gene.
How is Cylindroma Treated?
The cylindroma is treated by signal inhibition to the CYLD gene, surgical excision, curettage and cryotherapy, and electrodesiccation.
What is the Prognosis of Cylindroma?
The prognosis of cylindroma is good if it is not cancerous but if it is the prognosis is poor.
What is an Eccrine Poroma?
Eccrine poroma is a benign tumor of the sweat gland arising from the intraepidermal section.
What is the Pathology of Eccrine Poroma?
The pathology of eccrine poroma is:
-Etiology: The cause of eccrine poroma is not well understood but can be caused by hereditary factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to eccrine poroma is not clearly stated but is known to have begun from the epidermal section of the skin.
-Morphology: The morphology associated with eccrine poroma shows a surface that can be smooth or ulcerated, can be oink white or blue, and can be dome-shaped or nodule.
-Histology: The histology associated with eccrine poroma shows cells that are small in size, cuboidal, and have a deeply basophilic nucleus, well-circumscribed.
How does Eccrine Poroma Present?
Patients with eccrine poroma typically affect all gender equally and are mostly found to be occurring in the 4th -8th decade of life. The symptoms, features, and clinical findings associated with eccrine poroma include rapid growing masses, dome-shaped very painful, easily bleeding when touched, and can have a clear discharge and are pink or white or blue.
How is Eccrine Poroma Diagnosed?
The eccrine poroma is diagnosed by physical examination, history taking, and skin biopsy.
How is Eccrine Poroma Treated?
The eccrine poroma is treated mostly by excision and also cryosurgery can be recommended.
What is the Prognosis of Eccrine Poroma?
The prognosis of eccrine poroma is good since it rarely has any need for clinical attention.
What is a Pilomatricoma?
Pilomatricoma is also known as calcifying epithelioma of Malherbe is a benign tumor of the appendages in the hair follicles mainly on the face and the upper extremities.
What is the Pathology of Pilomatricoma?
The pathology of pilomatricoma is the scientific study of the conditions affecting the hair follicles.
-Etiology: The cause of pilomatricoma is genetic mutation mostly found in the hair matrix.
-Genes involved: CTNNB1 gene.
-Pathogenesis: The sequence of events that lead to pilomatricoma is due to the genetic change of the CTNNB1 gene which causes suppression of the normal process of cell death.
-Morphology: The morphology associated with pilomatricoma shows a purple-colored lesion that is slow-growing found on the head and neck.
-Histology: The histology associated with pilomatricoma shows three features, the areas of calcification, outer basophilic cells, and inner shadow cells.
How does Pilomatricoma Present?
Patients with pilomatricoma typically affect mostly children but may also be seen in adults according to recent studies. It is commonly seen in females than in males. The symptoms, features, and clinical findings associated with pilomatricoma include a solitary nodule, highly asymptomatic, non-tender to touch, and slow-growing can become painful only when there is formation of an ulcer.
How is Pilomatricoma Diagnosed?
The pilomatricoma is diagnosed by physical examination, x-rays, ultrasound and at some point, biopsy is done.
How is Pilomatricoma Treated?
The pilomatricoma is treated the main treatment option is total surgical excision of the nodule and if the immediate skin is involved it may be scraped off too.
What is the Prognosis of Pilomatricoma?
The prognosis of pilomatricoma is good with proper management and care.
What is a Sebaceous Adenoma?
Sebaceous adenoma is a small benign nodule that occurs mostly at the face and arises from the sebaceous gland.
What is the Pathology of Sebaceous Adenoma?
The pathology of sebaceous adenoma is the study of the abnormality of the sebaceous gland.
-Etiology: The cause of sebaceous adenoma is genetic predisposition.
-Genes involved: MLH1, MSH2, MSH6.
-Pathogenesis: The sequence of events that lead to sebaceous adenoma; the mismatch repair proteins, expression of PMS2, MSH2, MLH1, and MSH6, has been advocated as a first-line.
-Morphology: The morphology associated with sebaceous adenoma shows yellow papules mostly located at the head or face and can range from 0.5 – 9.0 centimeters.
-Histology: The histology associated with sebaceous adenoma shows sebaceous glands that are incompletely differentiated and have irregular lobes.
How does Sebaceous Adenoma Present?
Patients with sebaceous adenoma typically occur equally to both men and women with a mean age of 60 years. The symptoms, features, and clinical findings associated with sebaceous adenoma include slow-growing and are mostly asymptomatic.
How is Sebaceous Adenoma Diagnosed?
The sebaceous adenoma is diagnosed with blood work-ups, skin biopsy, CT scan, and MRI.
How is Sebaceous Adenoma Treated?
The sebaceous adenoma is treated by surgical, removal of the adenoma and long term monitoring.
What is the Prognosis of Sebaceous Adenoma?
The prognosis of sebaceous adenoma is good.
What are Syringomas?
Syringomas are mostly non-cancerous growths of the sweat glands.
What is the Pathology of Syringomas?
The pathology of syringomas is: the study of the tumors that arise from the sweat glands.
-Etiology: The cause of syringomas is increased multiplication of the cells in the sweat glands and can be genetic and diabetes mellitus.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to syringomas is the overgrowth of the cells found in the sweat glands.
-Morphology: The morphology associated with syringomas shows clusters that are either brown, pink, or yellow, found mostly near the eyes. They are around 1-4 mm.
-Histology: The histology associated with syringomas shows numerous small ducts embedded in a stroma that is sclerotic with a margin that can be cuboidal to the flattened epithelial lining.
How does Syringomas Present?
Patients with syringomas typically affect females more than males and appear mostly during puberty. The symptoms, features, and clinical findings associated with syringomas are very rare but some may have itchiness and pain.
How is Syringomas Diagnosed?
The syringomas are diagnosed mainly by physical examination but a biopsy may be done to exclude it from other tumors.
How is Syringomas Treated?
The syringomas are treated using trichloroacetic acid which makes them fall off and surgery, laser removal, and electric cauterization.
What is the Prognosis of Syringomas?
The prognosis of syringomas is good since they can be treated and if they recur it is also easy to treat them.
What are Tumors of the Dermis?
Tumors of the dermis are tumors arising from the inner layer of the skin sweat glands.
Examples of tumors of the dermis include:
- Dermatofibroma
- Dermatofibrosarcoma protuberans
What is a Dermatofibroma?
Dermatofibroma is a nodule of cutaneous origin and is also known as the cutaneous fibrous histiocytoma.
What is the Pathology of Dermatofibroma?
The pathology of dermatofibroma is the scientific study of the dermis and the conditions arising from the dermis.
-Etiology: The cause of dermatofibroma can be trauma e.g. insect bite, change in immunity, and genetic predisposition.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to dermatofibroma is the continuous excessive growth of the fibrous tissue of the dermis, is not known.
-Morphology: The morphology associated with dermatofibroma shows painless pink firm nodule with some itchiness and may vary in color as time goes by.
-Histology: The histology associated with dermatofibroma shows acanthotic epithelium with basilar hyperpigmentation and collagen trapping by dermal fibrohystiocytic infiltrates and are well circumscribed.
How does Dermatofibroma Present?
Patients with dermatofibroma typically occur in females and present at the age range of teenagers to adults. The symptoms, features, and clinical findings associated with dermatofibroma include itchiness and tenderness but are painless redness.
How is Dermatofibroma Diagnosed?
The dermatofibroma is diagnosed by physical examination, biopsy, and sonography.
How is Dermatofibroma Treated?
The dermatofibroma is treated by cryotherapy, steroid injection, surgical excision.
What is the Prognosis of Dermatofibroma?
The prognosis of dermatofibroma is good since they are slow-growing and are noncancerous.
What is Dermatofibrosarcoma Protuberans?
Dermatofibrosarcoma protuberans is a neoplasm that can be intermediate to low-grade malignancy and invades other tissues like the muscles and bones.
What is the Pathology of Dermatofibrosarcoma Protuberans?
The pathology of dermatofibrosarcoma protuberans is the study of the soft tissue of the skin that are cancerous.
-Etiology: The cause of dermatofibrosarcoma protuberans is a chromosomal deviation from the normal,
-Genes involved: COL1A, PDGFB.
-Pathogenesis: The sequence of events that lead to dermatofibrosarcoma protuberans is a result of increased proliferation of one of the types of cells found in the human body.
-Morphology: The morphology associated with dermatofibrosarcoma protuberans shows irregular nodules that vary in size and color (pink to red to brownish) and are very firm on touch.
-Histology: The histology associated with dermatofibrosarcoma protuberans shows irregular high cellularity, spindle-shaped cells, has a storiform growth pattern, and a diffuse infiltrative pattern.
How does Dermatofibrosarcoma Protuberans Present?
Patients with dermatofibrosarcoma protuberans are typically male with a 57% rate and occur mostly in adults with a mean age of 20-50 years. The symptoms, features, and clinical findings associated with dermatofibrosarcoma protuberans include an asymptomatic, sclerotic plaque, and when it is enlarging it has fast growth and an ulcer is formed.
How is Dermatofibrosarcoma Protuberans Diagnosed?
The dermatofibrosarcoma protuberans are diagnosed through physical examination, chest radiography in case metastasis is questioned and an MRI may be requested too.
How is Dermatofibrosarcoma Protuberans Treated?
The dermatofibrosarcoma protuberans are treated surgical removal and radiotherapy as an adjunct and molecular targeted drug the imatinib mesylate.
What is the Prognosis of Dermatofibrosarcoma Protuberans?
The prognosis of dermatofibrosarcoma protuberans is poor mainly in those with a mean age of 50-years-old.
What are Bullous Diseases?
Bullous diseases are blistering disorders a skin condition characterized by fluid-filled skin swellings.
Examples of bullous diseases include:
- Pemphigus vulgaris
- Bullous pemphigoid
- Cicatricial pemphigoid
- Dermatitis herpetiformis
What is Pemphigus Vulgaris?
Pemphigus vulgaris is an autoimmune blistering disorder affecting the skin and the cutaneous layer and causes the formation of flaccid bullae on the skin and mucosa.
What is the Pathology of Pemphigus Vulgaris?
The pathology of pemphigus vulgaris is: the study of the disease affecting the skin and the mucosa.
-Etiology: The cause of pemphigus vulgaris is a result of autoimmunity but can be triggered by environmental factors e.g. exposure to chemicals.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pemphigus vulgaris antibody-mediated hypersensitivity causes the formation of lesions.
-Morphology: The morphology associated with pemphigus vulgaris shows superficial flaccid vesicles and bullae that rupture easily.
-Histology: The histology associated with pemphigus vulgaris shows supra basal bullae in location so that the basal layer remains attached to the dermis like a row of tombstones. The bullous cavity contains serum and acantholytic epidermal cells.
How does Pemphigus Vulgaris Present?
Patients with pemphigus vulgaris typically are the elderly and most common in males than females. age of 50-60 years. The symptoms, features, and clinical findings associated with pemphigus vulgaris include very painfulness, secondary infection, itchiness, discomfort, formation of blisters.
How is Pemphigus Vulgaris Diagnosed?
The diagnosis of pemphigus vulgaris is histopathology, direct and indirect immunofluorescence,
How is Pemphigus Vulgaris Treated?
The pemphigus vulgaris is treated immunosuppressive therapy, corticosteroids to inhibit inflammation, anti-tumor necrosis factor drugs.
What is the Prognosis of Pemphigus Vulgaris?
The prognosis of pemphigus vulgaris is good in childhood than in adulthood. If the disease is in a few areas the prognosis is good than if it has widespread.
What is Bullous Pemphigoid?
Bullous pemphigoid is an autoimmune disorder of the skin and mucosa that is chronic that occurs when the body attacks its cells.
What is the Pathology of Bullous Pemphigoid?
The pathology of bullous pemphigoid is:
-Etiology: The cause of bullous pemphigoid is immune mediated.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to bullous pemphigoid is the deposition of antibodies IgG and complement in the basement membrane of the skin.
-Morphology: The morphology associated with bullous pemphigoid shows tense bullae filled with clear fulfilled in the sacs on the skin.
-Histology: The histology associated with bullous pemphigoid shows the presence of perivascular infiltrate of lymphocytes and some eosinophils, occasional neutrophils, superficial dermal edema.
How does Bullous Pemphigus Present?
Patients with bullous pemphigus typically is equal to both men and women. The elderly with a mean age of 65years. The symptoms, features, and clinical findings associated with bullous pemphigoid include the formation of bullae (generalized bullous form), small tense blisters (vesicular form), vegetative form, exfoliative erythroderma, and nodular.
How is Bullous Pemphigoid Diagnosed?
The bullous pemphigoid is diagnosed, histopathology, direct and indirect immunofluorescence.
How is Bullous Pemphigoid Treated?
The bullous pemphigoid is treated by use of anti-inflammatories, immunosuppressants.
What is the Prognosis of Bullous Pemphigoid?
The prognosis of bullous pemphigoid is fair since any fatality that occurs mostly occurs as a result of the medication.
What is Cicatricial Pemphigoid?
Cicatricial pemphigoid is a disease of the skin and the mucosa membranes that affects the subepidermal layer.
What is the Pathology of Cicatricial Pemphigoid?
The pathology of cicatricial pemphigoid is the scientific study of the disease of the skin and the mucosal layer.
-Etiology: The cause of cicatricial pemphigoid is not well known but can be drug-induced and presence of antibodies.
-Genes involved: COL17A1.
-Pathogenesis: The sequence of events that lead to cicatricial pemphigoid occurs when the antibodies that are used to maintain adhesion of tissue fail to do so due leading to separation of the dermis and the epidermis hence the formation of blisters.
-Morphology: The morphology associated with cicatricial pemphigoid shows the following depending on whether it is on the eye or the mucosa, tense blisters and erosions, symblepharon on the eye
-Histology: The histology associated with cicatricial pemphigoid shows clusters of erythrocytes in the subepithelial space, neutrophils, and lymphocytes are present together with the plasma cells.
How does Cicatricial Pemphigoid Present?
Patients with cicatricial pemphigoid typically affect the elderly mostly females with a mean age of 60-70 years. The symptoms, features, and clinical findings associated with cicatricial pemphigoid include continuous painful lesions of the skin depending on the location, erosions, inflammation, decreased tear and mucous production, and difficulty in breathing.
How Is Cicatricial Pemphigoid Diagnosed?
The cicatricial pemphigoid is diagnosed by physical exam, direct and indirect immunofluorescence, and biopsy.
How is Cicatricial Pemphigoid Treated?
The cicatricial pemphigoid is treated intralesional corticosteroids, topical therapy.
What is the Prognosis of Cicatricial Pemphigoid?
The prognosis of cicatricial pemphigoid is good if it is detected early but is poor if detected late due to its poor response to treatment.
What is Dermatitis Herpetiformis?
Dermatitis herpetiformis is a form of chronic, pruritic, vesicular dermatosis that mostly can be associated with celiac disease.
What is the Pathology of Dermatitis Herpertiformis?
The pathology of dermatitis herpertiformis is: the study of skin disease.
-Etiology: The cause of dermatitis herpertiformis is formation of antibodies against gluten found in diet
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to dermatitis herpertiformis is mostly due to genetics where persons develop IgA antibodies to gluten, as well as IgA autoantibodies that cross-react with endomysium and tissue transglutaminases, including epidermal transglutaminase expressed by keratinocytes.
-Morphology: The morphology associated with dermatitis herpertiformis shows a form of bilateral symmetry with neutrophils accumulating at the dermal papillae tips and injury to the basal layer.
-Histology: The histology associated with dermatitis herpertiformis shows neutrophilic micro abscess with eosinophils and granular deposition of the IgA antibodies of the tips of the papillary.
How does Dermatitis Herpertiformis Present?
Patients with dermatitis herpertiformis typically are maleS. The symptoms, features, and clinical findings associated with dermatitis herpetiformis include extreme pruritic urticaria, itchiness, redness and erosion, and a burning sensation.
How is Dermatitis Herpertiformis Diagnosed?
Dermatitis herpertiformis is diagnosed by physical exam, biopsy, and direct immunofluorescence.
How is Dermatitis Herpertiformis Treated?
The dermatitis herpertiformis is treated by encouraging a gluten-free diet and also the use of Dapsone medication.
What is the Prognosis of Dermatitis Herpertiformis?
The prognosis of dermatitis herpetiformis is good for those who can be able to handle a gluten free diet and dapsone medication.
What are Tumors of Cellular Migrants to the Skin?
Tumors of cellular migrants to the skin are the tumors that mostly and only arise from the progenitor cell of the human body.
Examples of tumors of cellular migrants to the skin include:
- Cutaneous T-cell lymphoma aka mycosis fungoides
- Mastocytosis
What is Cutaneous T-Cell Lymphoma aka Mycosis Fungoides?
Cutaneous T-cell lymphoma aka mycosis fungoides is a cutaneous disorder characterized by localization of the neoplastic T- lymphocytes.
What is the Pathology of Mycosis Fungoides?
The pathology of mycosis fungoides is the scientific study of the pathology that arises from the presence of T-lymphocytes.
-Etiology: The cause of mycosis fungoides is unclear.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mycosis fungoides involve Clonal growth of CD4 cells lacking the normal T cell antigens (CD7, CD5, CD 2).
-Morphology: The morphology associated with mycosis fungoides shows lymphoid atypia in the skin.
-Histology: The histology associated with mycosis fungoides shows mixed perivascular infiltrate, dermal papillae fibrosis.
How does Mycosis Fungoides Present?
Patients with mycosis fungoides typically slightly high in females than males, present at an age range of over 50 years. The symptoms, features, and clinical findings associated with mycosis fungoides occurs in three forms Premycotic stage in which the lesions are erythematous, red-brown, scaly and pruritic, Infiltrative stage with slightly elevated, bluish-red, firm plaques and the Fungoid stage include pruritic plaques, itchiness, patches on the lower trunk and the gluteal region and ulceration.
How is Mycosis Fungoides Diagnosed?
Mycosis fungoides is diagnosed by physical exam and history taking, and skin biopsy.
How is Mycosis Fungoides Treated?
Mycosis fungoides is treated by topical medication, and chemotherapy.
What is the Prognosis of Mycosis Fungoides?
The prognosis of mycosis fungoides is good if the disease is not advanced.
What is Mastocytosis?
Mastocytosis is a disorder characterized by increased proliferation and accumulation of the mast cells in various organs of the body
What is the Pathology of Mastocytosis?
The pathology of mastocytosis is:
-Etiology: The cause of mastocytosis is the extreme activity of mast cells.
-Genes involved: KIT.
-Pathogenesis: The sequence of events that lead to mastocytosis, the consequence of the chronic and episodic release of mast cell mediators, and extreme buildup of mast cells in a tissue.
-Morphology: Rash.
-Histology: The histology associated with mastocytosis shows infiltrates of the dermal mast cells around the blood vessels, round nuclei filled with cytoplasm.
How does Mastocytosis Present?
Patients with mastocytosis typically affect both males and females and the highest percentage are children and peaks at the age of 30-50 years. The symptoms, features, and clinical findings associated with mastocytosis include cutaneous lesions, flushing, headache, wheezing, diarrhea.
How is Mastocytosis Diagnosed?
The mastocytosis is diagnosed history taking and physical exam, CBC count, urinalysis, total tryptase level, bone scan and radiology.
How is Mastocytosis Treated?
The mastocytosis is treated by clearing the underlying symptoms such as the use of antihistamines, and topical corticosteroids.
What is the Prognosis of Mastocytosis?
The prognosis of mastocytosis is very good due to good response o the medication.
What are Familial Cancer Syndromes with Skin Manifestations?
Familial cancer syndromes with skin manifestations are genetic disorders tere is inheritance of mutated genes which manifest in an individual.
Examples of familial cancer syndromes with skin manifestations include:
- Ataxia-telangiectasia
- Cowden syndrome
- Familial melanoma syndrome
- Nevoid basal cell carcinoma syndrome
- Muir-Torre syndrome
- Neurofibromatosis type 1
- Neurofibromatosis type 2
- Tuberous sclerosis
- Xeroderma pigmentosum
What is Ataxia-Telangiectasia?
Ataxia telangiectasia is a very rare inherited disorder that affects the immune system, and nervous system.
What is the Pathology of Ataxia-Telangiectasia?
The pathology of ataxia-telangiectasia is:
-Etiology: The cause of ataxia-telangiectasia is mutations in the ATM
-Genes involved: Ataxia telangiectasia mutated (ATM)
-Pathogenesis: The sequence of events that lead to ataxia-telangiectasia are as a result of ATM gene mutation, which speciously controls the cell cycle and plays a key role in the guard of the genome.
-Morphology: The morphology associated with ataxia-telangiectasia shows progeric skin variations.
-Histology: The histology associated with ataxia-telangiectasia shows different granulomatous patterns.
How does Ataxia Telangiectasia Present?
Patients with ataxia-telangiectasia typically are children below the age of 5 years old and equally among males and females. The symptoms, features, and clinical findings associated with ataxia-telangiectasia include difficulty in movement coordination, inability to balance self, muscle twitching, slurred speech, clusters of the blood vessel are seen on the eyes.
How is Ataxia-Telangiectasia Diagnosed?
The ataxia-telangiectasia is diagnosed mostly by physical examination, history taking, a blood sample to identify the level of alpha-fetoprotein, genetic testing, and MRI.
How is Ataxia-Telangiectasia Treated?
The ataxia-telangiectasia is treated by the use of antibiotics, injection with immunoglobulins to lower chances of infection, use of beta-adrenergic blockers, regular screening to detect cancer.
What is the Prognosis of Ataxia-Telangiectasia?
The prognosis of ataxia-telangiectasia is poor if there is the involvement of the pulmonary system since most patients die during adolescence.
What is Cowden Syndrome?
Cowden syndrome is also known as multiple hamartoma syndrome.
What is the Pathology of Cowden Syndrome?
The pathology of cowden syndrome is:
-Etiology: The cause of cowden syndrome is mainly by the mutation of the PTEN gene and can be familial.
-Genes involved: Mutation of PTEN tumor suppressor gene.
-Pathogenesis: The sequence of events that lead to cowden syndrome is a result of mutation of the PTEN gene which is responsible for allowing cell death to be inhabited and there is the excess accumulation of the cells hence causing cowden syndrome.
-Morphology: The morphology associated with cowden syndrome shows distinctive clear, glycogenated, presence resembling the outer root sheath to the hair follicle.
-Histology: The histology associated with cowden syndrome shows lobules bound by a condensed eosinophilic membrane.
How does cowden syndrome Present?
Patients with cowden syndrome typically are affected equally but the type of cancer that may arise depends on the sex of the patient and the age-onset is from birth up to 46-years-old. The symptoms, features, and clinical findings associated with cowden syndrome depend on the system-affected oral lesions, cutaneous facial papules.
How is Cowden Syndrome Diagnosed?
Cowden syndrome is diagnosed by physical exam and history taking genetic testing,
How is Cowden Syndrome Treated?
Cowden syndrome is treated routine cancer screening, self-examination, and surgical care and long-term monitoring.
What is the Prognosis of Cowden Syndrome?
The prognosis of cowden syndrome is good if detected early.
What is Familial Melanoma Syndrome?
Familial melanoma syndrome is a group of skin diseases that have a common genetic origin.
What is the Pathology of Familial Melanoma Syndrome?
The pathology of familial melanoma syndrome is:
-Etiology: The cause of familial melanoma syndrome is CDKN2A and CD4K germline mutations.
-Genes involved: CDKN2A and CD4K.
-Pathogenesis: The sequence of events that lead to familial melanoma syndrome is poorly understood believed to be a result of CDKN2A and CD4K germline mutations.
-Morphology: The morphology associated with familial melanoma syndrome shows asymmetric, raised, color variegation present, of variable sizes.
-Histology: The histology associated with familial melanoma syndrome show lentiginous melanocytic hyperplasia with spindle or epithelioid melanocytes.
How does Familial Melanoma Syndrome Present?
Patients with familial melanoma syndrome typically difficult to estimate the gender prevalence present at an age range of 15 to 25 years. The symptoms, features, and clinical findings associated with familial melanoma syndrome include the presence of several primary melanomas, the inclination to develop superficial dispersion melanomas with absence sunburns, and a low amount of acral and nodular melanomas.
How is Familial Melanoma Syndrome Diagnosed?
Familial melanoma syndrome is diagnosed through the clinical familial history, dermoscopic studies. CT, MRI, and endoscopic ultrasound.
How is Familial Melanoma Syndrome Treated?
Familial melanoma syndrome is treated through surgical interventions, chemotherapy, and lifetime follow-up.
What is the Prognosis of Familial Melanoma Syndrome?
The prognosis of familial melanoma syndrome is poor as it associated with other ailments and high relapse.
What is Nevoid Basal Cell Carcinoma Syndrome?
Nevoid basal cell carcinoma syndrome is a pattern of multiple organ abnormalities caused by the mutation of the PTCH gene causing multiple basal cell skin cancer.
What is the Pathology of Familial Melanoma Syndrome?
The pathology of familial melanoma syndrome is:
-Etiology: The cause of nevoid basal cell carcinoma is mostly mutation of genes, UV light exposure and radiation.
-Genes involved: PTCH1 and PTCH2 and the SUFU genes
-Pathogenesis: The sequence of events that lead to familial melanoma syndrome are genetic.
-Morphology: The morphology associated with familial melanoma syndrome are skin lesions.
-Histology: The histology associated with familial melanoma syndrome are melanocytic neoplasms.
How does Nevoid Basal Cell Carcinoma Present?
Patients with nevoid basal cell carcinoma typically may occur from the age of 20 years. The symptoms, features, and clinical findings associated with nevoid basal cell carcinoma include cysts of the jaws, calcium deposition in the brain, pits on the palm of the hands and skeletal bone changes.
How is Nevoid Basal Cell Carcinoma Diagnosed?
The nevoid basal cell carcinoma is diagnosed by physical examination, CT scan and MRI.
How is Nevoid Basal Cell Carcinoma Treated?
The nevoid basal cell carcinoma is treated surgically and chemotherapy and also management of the symptoms.
What is the Prognosis of Nevoid Basal Cell Carcinoma?
The prognosis of nevoid basal cell carcinoma is fair.
What is Muir-Torre Syndrome?
Muir-Torre syndrome is a form of lynch syndrome characterized by oil gland skin tumors mostly affecting the gastrointestinal tract.
What is the Pathology of Muir-Torre?
The pathology of muir-torre syndrome is the scientific study of the oil gland tumors in the gastrointestinal tract.
-Etiology: The cause of muir-torre syndrome is gene mutation.
-Genes involved: MS2, MLH1, MLH6 and the MLH3 genes.
-Pathogenesis: The sequence of events that lead to Muir-Torre syndrome is genetic.
-Morphology: The morphology associated with muir-torre syndrome shows unevenly sized, partly differentiated sebaceous lobules.
-Histology: The histology associated with muir-torre syndrome shows a sebaceous cell with prominent cytoplasmic vacuoles.
How does Muir-Torre Syndrome Present?
Patients with muir-torre syndrome typically males are more affected than the female with the age ranging from the young adults to the elderly. The symptoms, features, and clinical findings associated with muir-torre syndrome include the presence of a sebaceous tumor, internal malignancy, familial history of cancer mostly the close relatives
How is Muir-Torre Syndrome Diagnosed?
The Muir-Torre syndrome is diagnosed physical examination, history taking, dermatoscopy, confocal microscopy.
How is Muir-Torre Syndrome Treated?
The Muir-Torre syndrome is treated by oral isotretinoin and surgical removal.
What is the Prognosis of Muir-Torre Syndrome?
The prognosis of muir-torre syndrome is poor due to the high rate of recurrence even after surgical removal.
What is Neurofibromatosis Type 1?
Neurofibromatosis type 1 is a medical condition characterized by a change in skin pigmentation and the development of nerve tumors.
What is the Pathology of Neurofibromatosis Type 1?
The pathology of neurofibromatosis type 1 is the scientific study of the changes that cause the skin to cause changes in pigmentation.
-Etiology: The cause of neurofibromatosis is the mutation of the NF1 gene which regulates excessive cell growth.
-Genes involved: NF1 gene.
-Pathogenesis: The sequence of events that lead to neurofibromatosis type 1; results from the NF1 gene mutation/deletion. The gene artifact neurofibromin obliges as a tumor suppressor.
-Morphology: The morphology associated with neurofibromatosis type 1 shows large volumes of cortical and subcortical structures and can be cutaneous, subcutaneous, and also plexiform lesions.
-Histology: The histology associated with neurofibromatosis type 1 shows Schwann cells with wire-like collagen, are infiltrative with myxoid areas, and has Meissner corpuscles
How does Neurofibromatosis Type 1 Present?
Patients with neurofibromatosis type 1 typically are of both gender and occur at the age of 20 years. The symptoms, features, and clinical findings associated with neurofibromatosis type 1 include macrocephaly, optical gliomas, scoliosis, early puberty, pseudoarthrosis, neurofibromas.
How is Neurofibromatosis Type 1 Diagnosed?
The neurofibromatosis type 1 is diagnosed history taking and physical examination, schwannomatosis, x-rays, CT scans and MRI.
How Is Neurofibromatosis Type 1 Treated?
The neurofibromatosis Type 1 is treated but close monitoring to check for any changes, surgical removal maybe involved and later radiotherapy and chemotherapy can be considered and the use of Selumetinib medication.
What is the Prognosis of Neurofibromatosis Type 1?
The prognosis of neurofibromatosis type 1 is good if there are no complications.
What is Neurofibromatosis Type 2?
Neurofibromatosis Type 2 is also known as central neurofibromatosis a genetic disorder marked by the development of tumors in the central and peripheral nervous system.
What is the Pathology of Neurofibromatosis Type 2?
The pathology of neurofibromatosis type 2 is: A multisystem genetic syndrome allied with spinal cord schwannomas, bilateral vestibular schwannomas, meningiomas, juvenile cataracts, with a paucity of cutaneous features, and gliomas.
-Etiology: The cause of neurofibromatosis is NF2 gene mutation
-Genes involved: NF2 gene.
-Pathogenesis: The sequence of events that lead to neurofibromatosis type 2 is a result of NF2 mutation, which severs as a tumor suppressor, declined function, and/or production of the gene grades to the tendency to develop of tumors.
-Morphology: Nodules.
-Histology: The histology associated with neurofibromatosis type 2 shows 3 cell types, glial cells, Schwann cells, or meningeal cells.
How does Neurofibromatosis Type 2 Present?
Patients with neurofibromatosis typically have no gender prevalence present at an age range of the early 20s. The symptoms, features, and clinical findings associated with neurofibromatosis type 2 include bilateral schwannomas, meningioma, gliomas, visual defects, cranial nerves palsies.
How is Neurofibromatosis Type 2 Diagnosed?
The neurofibromatosis type 2 is diagnosed genetic testing, imaging studies, auditory. Ophthalmic and histological.
How is Neurofibromatosis Type 2 Treated?
The neurofibromatosis type 2 is treated by tumor resection radiotherapy, pain medication chemotherapy, auditory brain stem implants.
What is the Prognosis of Neurofibromatosis Type 2?
The prognosis of neurofibromatosis is fair since it depends on the age and the progression of the disease.
What is Tuberous Sclerosis?
Tuberous sclerosis is an autosomal genetic disorder affecting cellular differentiation, multiplication, and migration.
What is the Pathology of Tuberous Sclerosis?
The pathology of tuberous sclerosis is: the gross and microscopic examination in a genetic illness affecting cellular differentiation, multiplication, and migration, resultant in hamartomatous lesions.
-Etiology: The cause of tuberous sclerosis is the mutation of genes.
-Genes involved: TSC-1, TSC-2 genes.
-Pathogenesis: The sequence of events that lead to tuberous sclerosis is a result of mTOR constitutively activation in hamartin or tuberin.
-Morphology: The morphology associated with tuberous sclerosis shows patches of light-colored skin, reddish bumps in the skin, and the nails, pink or dark in color.
-Histology: Atypia.
How does Tuberous Sclerosis Present?
Patients with tuberous sclerosis typically affect both sexes equally and the onset is at a very early age. The symptoms, features, and clinical findings associated with tuberous sclerosis include adenoma sebaceum, cardiac disease, retinal astrocytoma, giant ependymal astrocytoma.
How is Tuberous Sclerosis Diagnosed?
The tuberous sclerosis is diagnosed CT scan, blood workups, renal ultrasound, echocardiography.
How is Tuberous Sclerosis Treated?
The tuberous sclerosis is treated mainly by the use of antiepileptic medication, surgery, cryotherapy.
What is the Prognosis of Tuberous Sclerosis?
The prognosis of tuberous sclerosis is fair depending on the stage the disease is.
What is Xeroderma Pigmentosum?
Xeroderma pigmentosum is an inherited disease caused by the defectiveness of the DNA to repair.
What is the Pathology of Xeroderma Pigmentosum?
The pathology of xeroderma pigmentosum is:
-Etiology: The cause of xeroderma pigmentosum is exposure to UV light causing more damage to the skin that cannot repair itself chemical exposure.
-Genes involved: XPA, ERCC3, XP3, ERCC2.
-Pathogenesis: The sequence of events that lead to xeroderma pigmentosum results from a defect in nucleotide excision repair (NER), causing scarce repair of DNA damaged by UV radiation.
-Morphology: The morphology associated with xeroderma pigmentosum shows augmented melanin pigment at the basal cell layer.
-Histology: The histology associated with xeroderma pigmentosum shows hyperkeratosis, thinning, and atrophy of stratum malpighia, chronic inflammatory cell infiltrate in the dermis and irregular accumulation of melanin in the basal cell layer.
How does Xeroderma Pigmentosum?
Patients with xeroderma pigmentosum typically affect both males and females equally and the age onset of 2years. The symptoms, features, and clinical findings associated with xeroderma pigmentosum include persistent sunburn, blistering, scaling of the skin, crusting of the skin patches of the affected skin.
How is Xeroderma Pigmentosum Diagnosed?
Xeroderma pigmentosum is diagnosed by history and physical.
How is Xeroderma Pigmentosum Treated?
The xeroderma pigmentosum is treated by prevention of exposure to sunlight.
What is the Prognosis of Xeroderma Pigmentosum?
The prognosis of xeroderma pigmentosum is poor, the life expectancy is reduced by about 30-years-old.