Soft tissue pathology is the study of diseases that affect tissues other than bone and cartilage. These tissues include muscles, tendons, ligaments, fascia, blood vessels, nerves, and fat.
Soft tissue tumors generally fall within the following seven categories:
Adipose tissue
Fibrous tissue
Skeletal muscle
Smooth muscle
Vascular tissue
Nerve sheath tissue
Uncertain origin
What are Benign Adipose Soft Tissue Tumors?
Benign adipose soft tissue tumors include:
Lipoma
What Are Lipomas?
Lipomas are benign tumors of fat and are the most common soft tissue tumors in adults.
What is the Pathology of Lipomas?
The pathology of lipoma is:
-Etiology: The precise cause of lipomas is unknown.
-Genes involved: HMGA2-LPP fusion gene.
-Pathogenesis: The sequence of events that lead to lipoma formation is still unclear.
-Histology: The histology associated with lipoma shows mature, normal-appearing adipocytes with small eccentric nuclei.
How does Lipoma Present?
Patients with lipoma are typically males or females present at an age range of 40-50 years. The symptoms, features, and clinical findings associated with lipoma include the following a soft tissue well-circumscribed nodule.
How is Lipoma Diagnosed?
Common lipomas frequently are diagnosed clinically and are sent for histologic examination after complete surgical excision.
How is Lipoma Treated?
Lipoma is usually treated by surgical excision.
What is the Prognosis of Lipoma?
The prognosis of lipoma is excellent for benign lipomas. Recurrence is uncommon but may develop if the excision was incomplete.
What are Malignant Adipose Soft Tissue Tumors?
Malignant adipose soft tissue tumors:
Liposarcoma
Myxoid liposarcoma
Well-differentiated liposarcoma
What is a Liposarcoma?
Liposarcoma is a rare mesenchymal neoplasm that involves deep soft tissues.
What is the Pathology of Liposarcoma?
The pathology of liposarcoma is:
-Etiology: The cause of liposarcoma is still unknown.
-Genes involved: An abnormality of band 12q13, FUS-CHOP.
-Pathogenesis: The sequence of events that lead to liposarcoma are fusion proteins created by chromosomal abnormalities. has been associated with the development of liposarcomas.
-Histology: The histology associated with liposarcoma shows mature adipocytes with a variable amount of fibrous stroma containing atypical nuclei.
How does Liposarcoma Present?
Patients with liposarcoma are typically males slightly more than females present at an age range of about 50 years. The symptoms, features, and clinical findings associated with liposarcoma are usually not detectable until the tumor is large and impinges on neighboring structures, causing tenderness, pain, or functional disturbances.
How is Liposarcoma Diagnosed?
Liposarcoma is diagnosed by radiographic imaging and biopsy.
How is Liposarcoma Treated?
Liposarcoma is treated by surgical excision. Adjuvant radiation therapy or chemotherapy may be needed.
What is the Prognosis of Liposarcoma?
The prognosis of a liposarcoma depends on several factors but is typically fair with proper management.
What is a Myxoid Liposarcoma?
Myxoid liposarcoma is a malignant tumor made of primitive non-lipogenic mesenchymal cells.
What is the Pathology of Myxoid Liposarcoma?
The pathology of myxoid liposarcoma is:
-Etiology: The cause of myxoid liposarcoma is not well-established but trauma has been implicated in some cases.
-Genes involved: FUS-DDIT3, EWSR1-DDIT3.
-Pathogenesis: The sequence of events that lead to myxoid liposarcoma are reciprocal translocations between chromosomes 12 and 16 which cause the fusion of genes DDIT3 and FUS which activate downstream PPARgamma2 and C/EBPalpha. This promotes the proliferation of malignant cells.
-Histology: The histology associated with myxoid Liposarcoma shows a chicken-wire pattern and atypical adipocytes.
How does a Myxoid Liposarcoma Present?
Myxoid liposarcoma usually affects older males. The symptoms, features, and clinical findings associated with myxoid liposarcoma typically include feeling a deep mass with mild aching pain.
How is Myxoid Liposarcoma Diagnosed?
Myxoid liposarcoma is diagnosed by physical exam and biopsy.
How is Myxoid Liposarcoma Treated?
Myxoid liposarcoma is treated by wide surgical resection. Certain patients may benefit from adjuvant radiotherapy or chemotherapy. Amputation may be necessary for unresectable tumors.
What is the Prognosis of Myxoid Liposarcoma?
The prognosis of liposarcoma is generally poor. There is a high risk of local recurrence.
What is a Well Differentiated Liposarcoma?
Well, differentiated liposarcoma is the most common subtype of liposarcoma.
What is the Pathology of Well-differentiated Liposarcoma?
The pathology of well-differentiated liposarcoma is:
-Etiology: The cause of well-differentiated liposarcoma is extensive chromosomal aberrations.
-Genes involved: MDM2, CDK4, HMGA2.
-Pathogenesis: The sequence of events that lead to well-differentiated liposarcoma are having a diagnostic giant marker and ring chromosome, which affects uncontrolled cell proliferation.
-Histology: The histology associated with well-differentiated liposarcoma shows atypical stromal cells and lipoblasts in the context of mature fat.
How does Well-Differentiated Liposarcoma Present?
Patients with well-differentiated liposarcoma typically affect both males and females in the 6th decade of life. The symptoms, features, and clinical findings associated with well-differentiated liposarcoma include a painless mass present most often in the retroperitoneum or the limbs, urinary or bowel obstruction.
How is Well-Differentiated Liposarcoma Diagnosed?
Well-differentiated liposarcoma is diagnosed by CT scan and MRI.
How is Well-Differentiated Liposarcoma Treated?
Well-differentiated liposarcoma is treated mainly through tumor excision.
What is the Prognosis of Well-Differentiated Liposarcoma?
The prognosis of well-differentiated liposarcoma is good with complete tumor excision.
What are Benign Fibrous Soft Tissue Tumors?
Benign fibrous soft tissue tumors:
Fibromatosis
Nodular fasciitis
What is Fibromatosis?
Fibromatosis is a rare benign growth of the breast’s stroma made up of spindle-shaped cells that closely resemble normal breast cells.
What is the Pathology of Fibromatosis?
The pathology of Fibromatosis is:
-Etiology: The exact cause of fibromatosis remains unclear.
-Genes involved: Somatic β-catenin, CTNNB1, or APC gene.
-Pathogenesis: The sequence of events that lead to fibromatosis may be driven by a combination of genetic mutations, high estrogen states, and antecedent trauma which leads to activation of the canonical Wnt / β catenin pathway.
-Histology: The histology associated with fibromatosis shows long, sweeping fascicles with thin-walled vessels and microhemorrhages, bland cells with mild to moderate cellularity, and minimal atypia.
How does Fibromatosis Present?
Patients with fibromatosis typically affect females present at the age range of 36-42 years. The symptoms, features, and clinical findings associated with fibromatosis include cafe au lait spots, freckling in the armpits or groin area, lisch nodules, neurofibromas, and optic glioma.
How is Fibromatosis Diagnosed?
Fibromatosis is diagnosed by MRI, CT scan, and biopsy.
How is Fibromatosis Treated?
Fibromatosis is treated by surgical excision with a wide surgical margin.
What is the Prognosis of Fibromatosis?
The prognosis of fibromatosis is poor with local aggression of 20 – 30%.
What is Nodular Fasciitis?
Nodular fasciitis is a benign, soft tissue tumor.
What is the Pathology of Nodular Fasciitis?
The pathology of nodular fasciitis is:
-Etiology: The cause of nodular fasciitis is unknown. However, it is thought to be the local reaction to traumatic injuries.
-Genes involved: USP-6 and MYH-9.
-Pathogenesis: The sequence of events that lead to nodular fasciitis involves the self-limiting growth of a clone of neoplastic cells that contain a fusion gene.
-Histology: The histology associated with nodular fasciitis shows spindle-shaped myofibroblastic cells.
How does Nodular Fasciitis Present?
Patients with nodular fasciitis typically affect both males and females present at an age range of 20-40 years. The symptoms, features, and clinical findings associated with nodular fasciitis show mild pain, discomfort, or soreness.
How is Nodular Fasciitis Diagnosed?
Nodular fasciitis is diagnosed through a sonogram, MRI, CT scan, and biopsy.
How is Nodular Fasciitis Treated?
Nodular fasciitis is treated by simple excision.
What is the Prognosis of Nodular Fasciitis?
The prognosis of nodular fasciitis is excellent.
What are Malignant Fibrous Soft Tissue Tumors?
Malignant fibrous soft tissue tumors:
Malignant fibrous histiocytoma.
What is Malignant Fibrous Histiocytoma?
Malignant fibrous histiocytoma is pleomorphic sarcoma composed of fibroblasts, myofibroblasts, and histiocyte-like cells.
What is the Pathology of Malignant Fibrous Histiocytoma?
The pathology of malignant fibrous histiocytoma is:
Etiology: The cause of malignant fibrous histiocytoma is not clear. Although these tumors may be linked to other medical conditions such as Paget disease, certain chemotherapy treatments, or past radiation treatments.
-Genes involved: G1/S checkpoint genes.
-Pathogenesis: The sequence of events that lead to malignant fibrous histiocytoma has not been clarified to date. However, it has been recognized as a complication of radiation, resulting from chronic postoperative repair, trauma, surgical incisions, or burn scars.
-Histology: The histology associated with malignant fibrous histiocytoma shows high cellularity, marked nuclear pleomorphism, usually accompanied by abundant mitotic activity and a spindle cell morphology.
How does Malignant Fibrous Histiocytoma Present?
Patients with malignant fibrous histiocytoma typically affect males slightly more than females present at an age of more than 50 years. The symptoms, features, and clinical findings associated with malignant fibrous histiocytoma include painless, enlarging nodules that can become painful if enlarging rapidly.
How is Malignant Fibrous Histiocytoma Diagnosed?
Malignant fibrous histiocytoma is diagnosed through MRI and biopsy.
How is Malignant Fibrous Histiocytoma Treated?
Malignant fibrous histiocytoma is treated with wide local excision.
What is the Prognosis of Malignant Fibrous Histiocytoma?
The prognosis of malignant fibrous histiocytoma is good since it is superficial, small in size, and low grade.
What are Benign Skeletal Muscle Soft Tissue Tumors?
Benign skeletal muscle soft tissue tumors are soft tissue tumors that tend not to metastisize.
Examples of benign skeletal muscle soft tissue tumors include:
Rhabdomyoma
What is a Rhabdomyoma?
Rhabdomyoma is a benign tumor of striated muscle.
What is the Pathology of Rhabdomyoma?
The pathology of rhabdomyoma is:
-Etiology: The cause of rhabdomyoma is genetic modification during the development of striated muscle.
-Genes involved: TSC1, TSC2.
-Pathogenesis: The sequence of events that lead to rhabdomyoma involves mutations in the TSC1 and TSC2 genes.
-Morphology: The morphology associated with rhabdomyoma shows the presence of a mixture of spindle-shaped cells with indistinct cytoplasm and muscle fibers, which resemble striated muscle tissue.
-Histology: The histology associated with rhabdomyoma shows well-circumscribed, not encapsulated, sheets of large, well-differentiated skeletal muscle cells.
How does Rhabdomyoma Present?
Patients with rhabdomyoma typically affect males present at the age range of over 60 years. The symptoms, features, and clinical findings associated with rhabdomyoma include mass in the region of the neck, hoarseness, difficulty breathing, difficulty swallowing, or a combination.
How is Rhabdomyoma Diagnosed?
Rhabdomyoma is diagnosed using imaging and biopsy.
How is Rhabdomyoma Treated?
Rhabdomyoma is treated with excision.
What is the Prognosis of Rhabdomyoma?
The prognosis of rhabdomyoma is good. Excision is curative but may recur if incompletely excised.
What are Malignant Skeletal Muscle Soft Tissue Tumors?
Malignant skeletal muscle soft tissue tumors tend to cause damage and potentially metastisize.
Examples of malignant skeletal muscle soft tissue tumors include:
Alveolar rhabdomyosarcoma
Embryonal rhabdomyosarcoma
What is Alveolar Rhabdomyosarcoma?
Alveolar rhabdomyosarcoma is a subtype of the rhabdomyosarcoma soft tissue cancer family whose lineage is from mesenchymal cells, and which is related to skeletal muscle cells.
What is the Pathology of Alveolar Rhabdomyosarcoma?
The pathology of alveolar rhabdomyosarcoma is:
-Etiology: The cause of alveolar rhabdomyosarcoma is usually sporadic with no genetic predisposition.
-Genes involved: PAX3-FOXO1, PAX7-FOXO1.
-Pathogenesis: The sequence of events that lead to alveolar rhabdomyosarcoma include several genetic recombination events acting together cause the fusion protein, which leads to dysregulation of transcription and acts as an oncogene.
-Histology: The histology associated with alveolar rhabdomyosarcoma shows larger, uniformly round to polygonal cells, variable number of rhabdomyoblasts, multinucleated tumor giant cells with wreath-like nuclei, and mitoses.
How does Alveolar Rhabdomyosarcoma Present?
Patients with alveolar rhabdomyosarcoma typically affect both males and females present at the age range of older children to young adults. The symptoms, features, and clinical findings associated with alveolar rhabdomyosarcoma show a soft mass of tissue that is painless, but the tumor can be detected if it starts to put pressure on other structures in the primary site.
How is Alveolar Rhabdomyosarcoma Diagnosed?
Alveolar rhabdomyosarcoma is diagnosed by immunostaining.
How is Alveolar Rhabdomyosarcoma Treated?
Alveolar rhabdomyosarcoma is treated with standard surgery, radiation therapy, and intensive chemotherapy.
What is the Prognosis of Alveolar Rhabdomyosarcoma?
The prognosis of alveolar rhabdomyosarcoma is poor with a 4-year survival rate.
What is Embryonal Rhabdomyosarcoma?
Embryonal rhabdomyosarcoma is a rare histological form of cancer of connective tissue wherein the mesenchymal-derived malignant cells resemble the primitive developing skeletal muscle of the embryo.
What is the Pathology of Embryonal Rhabdomyosarcoma?
The pathology of embryonal rhabdomyosarcoma is:
-Etiology: The cause of embryonal rhabdomyosarcoma is sporadic with no genetic predisposition.
-Genes involved: RAS family of oncogenes.
-Pathogenesis: The sequence of events that lead to embryonal rhabdomyosarcoma are translocations resulting in altered expression, function, and subcellular localization of the fusion products relative to the wild-type proteins, and ultimately contributing to oncogenic behavior by modifying growth, differentiation, and apoptosis pathways.
-Histology: The histology associated with embryonal rhabdomyosarcoma shows primitive mesenchymal cells that show variable degrees of skeletal muscle differentiation.
How does Embryonal Rhabdomyosarcoma Present?
Patients with embryonal rhabdomyosarcoma typically affect both males and females present at the age range of 0-4 years. The symptoms, features, and clinical findings associated with embryonal rhabdomyosarcoma shows lump or swelling that keeps getting bigger or does not go away, it may be painful, crossed eyes or bulging of the eye, headache, trouble urinating or having bowel movements, blood in the urine, bleeding in the nose, throat, vagina, or rectum.
How is Embryonal Rhabdomyosarcoma Diagnosed?
Embryonal rhabdomyosarcoma is diagnosed by X-rays, MRI, PET scan, CT scan, and biopsy.
How is Embryonal Rhabdomyosarcoma Treated?
Embryonal rhabdomyosarcoma is treated with surgery.
What is the Prognosis of Embryonal Rhabdomyosarcoma?
The prognosis of embryonal rhabdomyosarcoma is good with over 70% of patients surviving for five years after diagnosis.
What are Benign Smooth Muscle Soft Tissue Tumors?
Examples of benign smooth muscle soft tissue tumors include:
Leiomyoma
What is a Leiomyoma?
Leiomyoma is the bland smooth muscle tumor without mitotic figures.
What is the Pathology of Leiomyoma?
The pathology of leiomyoma is:
-Etiology: The cause of leiomyoma is ischemia or hormonal stimulation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to leiomyoma is not well understood.
-Morphology: The morphology associated with leiomyoma shows monotonous spindle cells with indistinct borders arranged in intersecting fascicles.
-Histology: The histology associated with leiomyoma shows bundles or fascicles of spindled cells with eosinophilic and possibly fibrillar cytoplasm
How does Leiomyoma Present?
Patients with leiomyoma typically affect women present in the age range of 40 and above (postmenopausal). The symptoms, features, and clinical findings associated with leiomyoma include menorrhagia, pelvic pain, pelvic pressure, frequent urination, heavy menstrual bleeding, and difficulty emptying the bladder.
How is Leiomyoma Diagnosed?
Leiomyoma is diagnosed using ultrasound, MRI, and biopsy.
How is Leiomyoma Treated?
Leiomyoma is treated with hysterectomy or myomectomy.
What is the Prognosis of Leiomyoma?
The prognosis of leiomyoma is excellent as the patient remains asymptomatic for many years or indefinitely.
What are Malignant Smooth Muscle Soft Tissue Tumors?
Malignant smooth muscle soft tissue tumors:
Leiomyosarcoma
What is a Leiomyosarcoma?
Leiomyosarcoma is a rare tumor derived from smooth muscles. It has three types, spindle / conventional, epithelioid, and myxoid.
What is the Pathology of Leiomyosarcoma?
The pathology of leiomyosarcoma is:
-Etiology: The cause of leiomyosarcoma is unknown. However, genetics is considered one of the causes.
-Genes involved: TP53.
-Pathogenesis: The sequence of events that lead to leiomyosarcoma includes cytogenetic and molecular changes.
-Morphology: The morphology associated with leiomyosarcoma shows bulky, fleshy tumor invading into a myometrial wall or polypoid tumor projecting into the lumen.
-Histology: The histology associated with leiomyosarcoma shows severe atypia, increased mitoses, and tumor cell necrosis.
How does Leiomyosarcoma Present?
Patients with leiomyosarcoma typically affect females present at the age range of 40-69 years. The symptoms, features, and clinical findings associated with leiomyosarcoma include abnormal vaginal bleeding, lump or swelling under the skin, bloating and abdominal swelling.
How is Leiomyosarcoma Diagnosed?
Leiomyosarcoma is diagnosed using MRI and CT scans.
How is Leiomyosarcoma Treated?
Leiomyosarcoma is treated with total abdominal hysterectomy, bilateral salpingo-oophorectomy for postmenopausal females and those with metastatic disease.
What is the Prognosis of Leiomyosarcoma?
The prognosis of leiomyosarcoma is poor as therapeutic options are limited.
What are Benign Vascular Soft Tissue Tumors?
Benign vascular soft tissue tumors:
Hemangioma
What is a Hemangioma?
Hemangiomas are usually benign vascular tumors derived from blood vessel cell types.
What is the Pathology of Hemangioma?
The pathology of emangioma is:
-Etiology: The cause of hemangioma is not currently well-established.
-Genes involved: TEM8 (ANTXR1), VEGFR2, VEGFR3 (FLT4), and DUSP5.
-Pathogenesis: The pathogenesis of hemangiomas is characterized by endothelial and pericytic hyperplasia, followed by a slower but steady involution phase that may last for years.
-Histology: The histology associated with hemangiomas shows hyperplastic endothelial cells, pericytes with and without lumens, and prominent basement membranes.
How does Hemangioma Present?
Patients with hemangioma typically affect females five times more than males during infancy. The symptoms, features, and clinical findings associated with hemangioma include flat and erythematous red patches.
How is Hemangioma Diagnosed?
Hemangioma is diagnosed clinically through biopsy and CT scan.
How is Hemangioma Treated?
Hemangioma is treated through beta-blockers and corticosteroids.
What is the Prognosis of Hemangioma?
The prognosis of hemangioma is very good.
What are Malignant Vascular Soft Tissue Tumors?
Malignant vascular soft tissue tumors:
Angiosarcoma
What is an Angiosarcoma?
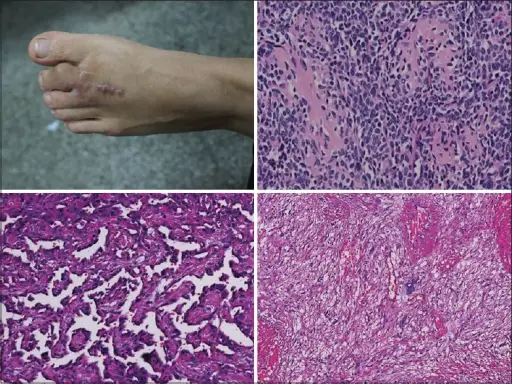
Angiosarcoma is a rare malignant vascular neoplasm of endothelial-type cells that line vessel walls.
What is the Pathology of Angiosarcoma?
The pathology of Angiosarcoma is:
-Etiology: The causes of angiosarcoma include exposure to vinyl chloride monomer (VCM) for prolonged periods, polyvinyl chloride (PVC) polymerization plants, arsenic-containing insecticides, and thorium dioxide irradiation.
-Genes involved: PTPRB/PLCG1.
-Pathogenesis: The pathogenesis of angiosarcoma is characterized by a rapid and extensive infiltrating overgrowth of vascular endothelial cells.
-Histology: The histology associated with angiosarcoma shows irregular anastomosing vascular spaces lined by endothelial cells.
How does Angiosarcoma Present?
Patients with angiosarcoma typically affect males more than females present at the age range of 40-75 years. The symptoms, features, and clinical findings associated with angiosarcoma show bruised, purple-ish areas on the skin.
How is Angiosarcoma Diagnosed?
Angiosarcoma is not diagnosed through MRI and CT scans.
How is Angiosarcoma Treated?
Angiosarcoma is treated by complete surgical resection with wide margins for local and locoregional disease in combination with preoperative or postoperative radiotherapy.
What is the Prognosis of Angiosarcoma?
The prognosis of angiosarcoma is generally poor. The 5-year survival rate of patients with angiosarcoma is approximately 12-33%.
What are Benign Nerve Sheath Soft Tissue Tumors?
Benign nerve sheath soft tissue tumors:
Schwannoma
Neurofibroma
What is a Schwannoma?
Schwannoma is a benign nerve sheath tumor arising from differentiated Schwann cells.
What is the Pathology of Schwannoma?
The pathology of Schwannoma is:
-Etiology: The cause of schwannoma is not identifiable as such. It is mostly sporadic.
-Genes involved: Merlin (schwannomin, NF2)
-Pathogenesis: The sequence of events that lead to schwannoma include loss of function of merlin, either by direct genetic change involving the NF2 gene on chromosome 22 or secondarily to merlin inactivation.
-Histology: The histology associated with schwannoma shows spindle cells.
How does Schwannoma Present?
Patients with schwannoma typically affect both males and females in the age range of 20-50 years. The symptoms, features, and clinical findings associated with schwannoma include a visible lump, numbness, muscle weakness, pins, and needles feeling, night-time back or neck pain, pains that are aching, burning, or sharp pain.
How is Schwannoma Diagnosed?
Schwannoma is diagnosed using imaging studies. A biopsy may confirm the diagnosis.
How is Schwannoma Treated?
Schwannoma is treated by surgery.
What is the Prognosis of Schwannoma?
The prognosis of schwannoma is usually good as they are slow-growing tumors.
What is a Neurofibroma?
Neurofibroma are benign nerve sheath tumors of neural origin in the peripheral nervous system.
What is the Pathology of Neurofibroma?
The pathology of Neurofibroma is:
-Etiology: The cause of neurofibroma is not known.
-Genes involved: NF-1.
-Pathogenesis: The pathogenesis of neurofibroma includes biallelic inactivation of the tumor suppressor gene neurofibromatosis type 1 which is located on 17q11.2.
-Histology: The histology associated with neurofibromas shows proliferation of all elements of peripheral nerves.
How does Neurofibroma Present?
Patients with neurofibroma typically affect both males and females in the age range of 20-30 years. The symptoms, features, and clinical findings associated with neurofibroma include soft masses, transient itching, pain, numbness and tingling in the affected area, severe bleeding, physical disfiguration, cognitive disability, stinging, neurological deficits, changes in movement (clumsiness in the hands, trouble walking), bowel incontinence, scoliosis, UTI, urinary retention, urgency, frequency, urinary incontinence, hematuria, hydronephrosis, or pelvic mass.
How is Neurofibroma Diagnosed?
Neurofibroma is diagnosed by immunohistochemistry, MRI, CT scan, and biopsy.
How is Neurofibroma Treated?
Neurofibroma is treated predominantly by surgical resection. Adjunctive chemotherapy and medications such as ACE inhibitors may be required.
What is the Prognosis of Neurofibroma?
The prognosis of neurofibroma is generally excellent.
What is a Malignant Peripheral Nerve Sheath Tumor?
A malignant peripheral nerve sheath tumor (MPNST) is a form of a malignant neoplasm of the connective tissue surrounding nerves.
What is the Pathology of Malignant Peripheral Nerve Sheath Tumor?
The pathology of malignant peripheral nerve sheath tumor is:
-Etiology: The cause of malignant peripheral nerve sheath tumors is either sporadic or due to NF-1 mutation.
-Genes involved: NF-1.
-Pathogenesis: The sequence of events that lead to malignant peripheral nerve sheath tumors is the germline mutations in NF1 predisposed to the development of peripheral nerve sheath neoplasms in patients with type 1 neurofibromatosis.
-Histology: The histology associated with malignant peripheral nerve sheath tumors shows a marbled appearance due to alternating hypocellular and hypercellular areas with perivascular accentuation.
How does Malignant Peripheral Nerve Sheath Tumor Present?
Patients with malignant peripheral nerve sheath tumors typically affect both males and females 40 years and above. The symptoms, features, and clinical findings associated with malignant peripheral nerve sheath tumor include peripheral edema, difficulty in moving the extremity, pain, and numbness.
How is Malignant Peripheral Nerve Sheath Tumor Diagnosed?
A malignant peripheral nerve sheath tumor is diagnosed by MRI.
How is Malignant Peripheral Nerve Sheath Tumor Treated?
Malignant peripheral nerve sheath tumor is treated predominantly by surgical resection. Adjunctive radio and chemotherapy may also be used.
What is the Prognosis of Malignant Peripheral Nerve Sheath Tumor?
The prognosis of malignant peripheral nerve sheath tumors is poor with high metastatic potential.
What are Benign Soft Tissue Tumors of Uncertain Origin?
Benign soft tissue tumors of uncertain origin:
Solitary fibrous tumor
What is a Solitary Fibrous Tumor?
The solitary fibrous tumor is a fibroblastic tumor.
What is the Pathology of Solitary Fibrous Tumor?
The pathology of solitary fibrous tumor is:
-Etiology: The cause of the solitary fibrous tumor is unknown.
-Genes involved: NAB2-STAT6.
-Pathogenesis: The sequence of events that lead to the solitary fibrous tumor is the paracentric inversion involving chromosome 12q, resulting in NAB2-STAT6 gene fusion.
-Histology: The histology associated with solitary fibrous tumors shows ovoid to fusiform spindle cells with indistinct cell borders arranged haphazardly or in short, ill-defined fascicles.
How does Solitary Fibrous Tumor Present?
Patients with solitary fibrous tumors typically affect both males and females at 40-70 years of age. The symptoms, features, and clinical findings associated with solitary fibrous tumors show painless lump with slow growth.
How is Solitary Fibrous Tumor Diagnosed?
A solitary fibrous tumor is diagnosed by histologic findings. Imaging features are non-specific.
How is Solitary Fibrous Tumor Treated?
Solitary fibrous tumor is treated by surgical resection.
What is the Prognosis of Solitary Fibrous Tumor?
The prognosis of solitary fibrous tumors is poor with a 10 – 30% (local or distant) recurrence rate.
What are Malignant Soft Tissue Tumors of Uncertain Origin?
Malignant soft tissue tumors of uncertain origin:
Alveolar soft part sarcoma
Clear cell sarcoma
Synovial sarcoma
Undifferentiated pleomorphic sarcoma
What is Alveolar Soft Part Sarcoma?
Alveolar soft part sarcoma is a rare, slow-growing soft-tissue tumor of an unclear cause.
What is the Pathology of Alveolar Soft Part Sarcoma?
The pathology of alveolar soft part sarcoma is:
-Etiology: The cause of alveolar soft part sarcoma is unknown.
-Genes involved: ASPL and TFE3.
-Pathogenesis: The sequence of events that lead to alveolar soft part sarcoma includes the chromosomal analysis which shows the breaking and joining of two chromosomes in the tumor cells.
-Histology: The histology associated with alveolar soft part sarcoma shows well-defined nests of cells separated by fibrous stroma.
How does Alveolar Soft Part Sarcoma Present?
Patients with alveolar soft part sarcoma typically affect young females at an age range of 30 years. The symptoms, features, and clinical findings associated with alveolar soft part sarcoma include a painless swelling, or soreness caused by compressed nerves or muscles, affecting the range of motion in the area.
How is Alveolar Soft Part Sarcoma Diagnosed?
Alveolar soft part sarcoma is diagnosed by imaging scans such as CT or MRI.
How is Alveolar Soft Part Sarcoma Treated?
Alveolar soft part sarcoma is treated by surgery combined with radiation therapy.
What is the Prognosis of Alveolar Soft Part Sarcoma?
The prognosis of alveolar soft part sarcoma is poor.
What is Clear Cell Sarcoma?
Clear cell sarcoma is a malignant soft tissue sarcoma composed of monotonous epithelioid and spindle cells with clear to eosinophilic cytoplasm characterized by melanocytic differentiation and EWSR1-ATF1 / CREB1 rearrangement.
What is the Pathology of Clear Cell Sarcoma?
The pathology of clear cell sarcoma is:
-Etiology: The cause of clear cell sarcoma is unknown.
-Genes involved: EWSR1-ATF1 / CREB1
-Pathogenesis: The sequence of events that lead to clear cell sarcoma is the recurrent chromosomal translocation, t(12; 22), resulting in fusion of the EWS gene on 22q12 with the ATF1 gene on 12q13.
-Histology: The histology associated with clear cell sarcoma shows nests of epithelioid spindle cells with clear eosinophilic cytoplasm and prominent nucleoli plus melanocytic differentiation
How does Clear Cell Sarcoma Present?
Patients with clear cell sarcoma typically affect both males and females present at the age range of 30 years and above. The symptoms, features, and clinical findings associated with clear cell sarcoma include a painless, slow-growing lump.
How is Clear Cell Sarcoma Diagnosed?
Clear cell sarcoma is diagnosed through MRI and biopsy.
How is Clear Cell Sarcoma Treated?
Clear cell sarcoma is treated by complete surgical excision with or without radiotherapy.
What is the Prognosis of Clear Cell Sarcoma?
The prognosis of clear cell sarcoma is poor with a 5-year survival rate in 50-65% of patients.
What is Synovial Sarcoma?
Synovial sarcoma is a malignant soft tissue tumor of uncertain histogenesis with variable epithelial differentiation.
What is the Pathology of Synovial Sarcoma?
The pathology of Synovial sarcoma is:
-Etiology: The etiology of synovial sarcoma is poorly understood.
-Genes involved: SS18 and either SSX1, SSX2 or SSX4
-Pathogenesis: The sequence of events that lead to synovial sarcoma is driven by the chromosomal translocation t(X;18)(p11;q11) involving genes SS18 and either SSX1, SSX2, or SSX4.
-Histology: The histology associated with synovial sarcoma shows poorly differentiated (round cell), monophasic epithelial, calcifying/ossifying, and myxoid findings.
How does Synovial Sarcoma Present?
Patients with synovial sarcoma typically affect males slightly more than females at the age of about 35 years. The symptoms, features, and clinical findings associated with synovial sarcoma include asymptomatic swelling or mass, and fatigue.
How is Synovial Sarcoma Diagnosed?
Synovial sarcoma is diagnosed by biopsy.
How is Synovial Sarcoma Treated?
Synovial sarcoma is treated by surgical resection and radiotherapy.
What is the Prognosis of Synovial Sarcoma?
The prognosis of Synovial sarcoma is poor.
What is Undifferentiated Pleomorphic Sarcoma?
Undifferentiated pleomorphic sarcoma is a rare type of cancer that begins mostly in the soft tissues of the body.
What is the Pathology of Undifferentiated Pleomorphic Sarcoma?
The pathology of Undifferentiated pleomorphic sarcoma is:
-Etiology: The etiology of undifferentiated pleomorphic sarcoma is not clear.
-Genes involved: TP53, RB1, CDKN2A, ATRX, and CDKN2B.
-Pathogenesis: The sequence of events that lead to undifferentiated pleomorphic sarcoma is the tumorigenesis of undifferentiated pleomorphic sarcoma initiated by a subpopulation of cells called side population cells, which the Hoechst dye efflux assay can identify.
-Histology: The histology associated with undifferentiated pleomorphic sarcoma shows spindle, round/epithelioid, or pleomorphic, demonstrating marked cytologic atypia.
How does Undifferentiated Pleomorphic Sarcoma Present?
Patients with undifferentiated pleomorphic sarcoma typically affect young adults’ males more than females present at the age range of 25 and above. The symptoms, features, and clinical findings associated with undifferentiated pleomorphic sarcoma include swelling, pain, tingling, and numbness.
How is Undifferentiated Pleomorphic Sarcoma Diagnosed?
Undifferentiated pleomorphic sarcoma is diagnosed through MRI and biopsy.
How is Undifferentiated Pleomorphic Sarcoma Treated?
Undifferentiated pleomorphic sarcoma is treated by surgical resection with a negative margin.
What is the Prognosis of Undifferentiated Pleomorphic Sarcoma?
The prognosis of undifferentiated pleomorphic sarcoma is fair.
What is a Myofibroma?
Myofibroma is a solitary nodular tumor of the soft tissue, bone, or internal organs.
What is the Pathology of Myofibroma?
The pathology of Myofibroma is:
-Etiology: The cause of myofibroma is a genetic mutation.
-Genes involved: PDGFRB, SRF-RELA.
-Pathogenesis: The sequence of events that lead to myofibroma is the mutations in the PDGFRB gene.
-Histology: The histology associated with myofibroma shows well-circumscribed, nodular neoplasms characterized by a distinctive biphasic growth pattern.
How does Myofibroma Present?
Patients with myofibroma typically affect males in early childhood or adulthood present at the age range of 15 years and above. The symptoms, features, and clinical findings associated with myofibroma include a painless, slow-growing mass.
How is Myofibroma Diagnosed?
Myofibroma is diagnosed by tissue sampling.
How is Myofibroma Treated?
Myofibroma is treated by surgery.
What is the Prognosis of Myofibroma?
The prognosis of myofibroma is good. They usually do not recur.