Spleen pathology is the scientific gross and microscopic pattern studies of the causes of disease and the associated changes at the levels of cells, tissues, and organs, which results in the presenting signs and symptoms associated with anomalies of the spleen.
What are Congenital Anomalies of the Spleen?
Congenital anomalies of the spleen are structural and, consequently, the functional abnormalities of the spleen arising during the developmental stage. Structural or functional abnormalities/anomalies allied to the spleen.
Congenital anomalies of the spleen include:
- Asplenia
- Hyposplenia
- Accessory spleens
What is Asplenia?
Asplenia is a disorder categorized with the anatomical absence of the spleen tissue. Asplenia stereotypically occurs in connotation with situs ambiguous also known as heterotaxia. Asplenia can be acquired or iatrogenic.
What is Hyposplenia?
Hyposplenia is an anomaly characterized by the absence of spleen functionality tributary to a diversity of ailment states. Splenic tissues exist, however they are smaller than usual and non-functioning. Hyposplenia presents with imbalances in the two basic roles of the spleen; fighting infection and filtering of dysfunctional red cells.
What are Accessory Spleens?
Accessory spleen is a congenital deviation characterized by the ectopic splenic tissue detached from the body of the spleen. Accessory spleens result from the failure of union of the primordial splenic buds at dorsal mesogastrium at the 5th-week of fetal life. Accessory spleens are diagnosed by imaging.
What are Cysts of the Spleen?
Cysts of the spleen include primary and secondary cysts, based on the existence of cellular or fibrous lining. True cysts are grouped into non-parasitic and parasitic. True non-parasitic cysts comprise congenital (epithelial), and neoplastic cysts (lymphangioma, metastases, haemangioma). False cysts may develop due to trauma, infarction-degeneration, hemorrhage, and also inflammation.
What is Nonspecific Acute Splenitis?
Nonspecific acute splenitis is the inflammation of the spleen that often is accompanied by enlargement of the spleen. Inflammation is due to micro-organisms or immune modulators such as cytokines that are unconfined as a response to antigens.
What is the Pathology of Nonspecific Acute Splenitis?
The pathology of nonspecific acute splenitis is:
-Etiology: The cause of nonspecific acute splenitis include viruses, bacterial, deficiency of vitamins and minerals. Acute or chronic infection (bacterial endocarditis, infectious mononucleosis, HIV, malaria, tuberculosis, histiocytosis, abscess).
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to nonspecific acute splenitis are infiltration of inflammatory cells, the proliferation of lymphoid follicles, congestion, and edema which is followed by propagation of fibrous tissues.
How does Nonspecific Acute Splenitis Present?
Patients with nonspecific acute splenitis typically there is no sex predilection is documented. Present at an age range of above 45-years-old, as the capsules of older spleens are thinner than their younger foils. The symptoms, features, and clinical findings associated with nonspecific acute splenitis include; splenic enlargement, congestion, and neutrophilic infiltration, which may occur in cases of sepsis due to the organisms themselves or secondary to inflammatory products.
How is Nonspecific Acute Splenitis Diagnosed?
Nonspecific acute splenitis is diagnosed by imaging studies including ultrasonography, noninvasive, highly sensitive aimed at evaluating splenic size. Angiographic findings to differentiate splenic cysts may also be utilized. Laboratory studies include a complete blood count (CBC) with differential, platelet count, and peripheral blood smear in cases of nonspecific acute splenitis.
How is Nonspecific Acute Splenitis Treated?
Nonspecific acute splenitis is treated through medical therapy which include antifungal treatment, parenteral broad-spectrum antibiotics, and corticosteroid therapy. Surgical interventions include percutaneous drainage and open drainage in case of an abscess develops.
What is the Prognosis of Nonspecific Acute Splenitis?
The prognosis of nonspecific acute splenitis is usually outstanding however, it is wedged by the underlying ailment causative state.
What is Splenomegaly?
Splenomegaly is defined as the enlargement of the spleen measured by weight or size. A typically sized spleen measures up to 12 cm craniocaudal length. The typical length of spleens are 12 cm to 20 cm, anything above designates splenomegaly. The standard weight of the adult spleen is around 70 g to 200 g. A weight of 400 g and above designates splenomegaly.
Disorders associated with splenomegaly include:
- Infections
- Congestive states related to portal hypertension
- Lymphohematogenous disorders
- Inflammatory conditions
- Lysosomal storage diseases
- Glycogen storage diseases
- Amyloidosis
- Primary neoplasms
- Secondary neoplasms
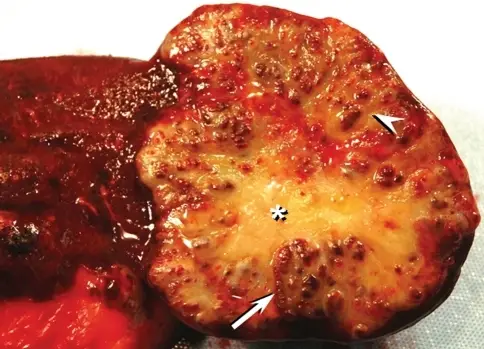
What are Splenic Infarcts?
Splenic infarcts are common lesions caused by the occlusion of the major splenic artery or any of its branches. Splenic infarction may be the result of arterial or venous occlusion usually caused by bland or septic emboli as well as venous congestion by abnormal cells.
What is the Pathology of Splenic Infarcts?
The pathology of splenic infarcts is:
-Etiology: The causes of splenic infarcts are may include bloodborne malignancy (lymphoma, leukemia), myelofibrosis, infections, trauma, or clotting issues.
-Genes involved: HBB (hemoglobin subunit beta).
-Pathogenesis: The sequence of events that lead to splenic infarcts are due to an abnormality of splenic circulation.
How does Splenic Infarcts Present?
Patients with splenic infarcts typically affect both genders. Present at an age range of 40-years-old. Splenic infarcts are typically due to thromboembolic ailments. The symptoms, features, and clinical findings associated with splenic infarcts include left-upper-quadrant abdominal pain. Additional symptoms of splenic infarcts include nausea and vomiting, fever and chills, pleuritic chest ache, and left shoulder agony.
How is Splenic Infarcts Diagnosed?
Splenic Infarcts is diagnosed through: Computed tomography (CT), performed with intravenous (IV) nonionic contrast. Magnetic resonance imaging (MRI), made with IV gadolinium contrast to identify infarcted splenic parenchyma. Other diagnosis modes include radioisotope scans and ultrasonographic evaluation of the spleen.
How is Splenic Infarcts Treated?
Splenic Infarcts is treated through analgesia, nonsteroidal anti-inflammatory drugs (NSAIDs), and close follow-up. An isolated splenic abscess can be treated with percutaneous drainage, and splenectomy avoided. Surgical intervention may be indicated in certain cases such as sepsis, hemorrhage, abscess, or tenacious pseudocyst formation.
What is the Prognosis of Splenic Infarcts?
The prognosis of splenic infarcts varies according to the primary disease accountable for the infarct. Massively enlarged spleens splenectomies, associated hematologic malignancies, are allied with mortalities of as high as above 35%. At the other end, many infarcts are clinically mysterious, with no significant long-term sequelae.
What is Mononucleosis?
Mononucleosis is a benign, self-limiting lymphoproliferative ailment caused by the Epstein-Barr virus (EBV), one of the herpesviruses. Also known as glandular fever. Contagion may occur from childhood to old age but the orthodox acute infection is more in adolescents and young adults. Conveyed by person-to-person contact such as by kissing.
What is the Pathology of Mononucleosis?
The pathology of mononucleosis is:
-Etiology: The cause of mononucleosis is the Epstein-Barr virus (EBV) also known as human herpesvirus 4, a widely disseminated double-stranded DNA herpes virus. Spread of Mononucleosis is by contact, typically salivary secretions.
-Genes involved: EBERs (LMP2A), EBNA1 and LMPs
-Pathogenesis: The sequence of events that lead to mononucleosis is Epstein-Barr virus is introduced into the oropharynx, begins the replication process. The predilection for infection of the B-cells of lymphoid tissue. The infection spreads over the lymphatic system. The body develops antibodies against the virus. In a higher percent, heterophile antibodies are produced in response to the infection.
-Histology: The histology related to mononucleosis shows the presence of lymphocytosis and increased circulating atypical lymphocytes which affirm the diagnosis of Epstein-Barr virus infection.
How does Mononucleosis Present?
Patients with mononucleosis typically, Epstein-Barr virus is widely dispersed in all population groups. However, the indicative infection is in adolescents of both genders. Present at an age range of 15 to 24-years. The symptoms, features, and clinical findings associated with mononucleosis include: The classical triad, fever, lymphadenopathy, pharyngitis, Other complaints are, tonsillar enlargement rash, and/or periorbital edema relative bradycardia, splenic tenderness
How is Mononucleosis Diagnosed?
Mononucleosis is diagnosed through, imaging, CT scan, and/or MRI to rule out other causes of encephalitis. Laboratory studies such as liver function tests, heterophile antibody tests, or Epstein-Barr virus-specific antibodies to affirm the presence of the disease may be done as well.
How is Mononucleosis Treated?
Mononucleosis is treated by medical care, which monitors patients with thrilling tonsillar enlargement for airway obstruction. Steroids for imminent or established airway obstruction. Surgery in case spontaneous splenic rupture, rare patients with Epstein-Barr virus infection. Refrain from active physical activity for a month.
What is the Prognosis of Mononucleosis?
The prognosis of (mononucleosis) is good. The majority of patients with Epstein-Barr virus infection recuperate without sequelae and develop enduring immunity to monitoring the dormant virus. The acute phase of the disease resolves by end of week two, but malaise indications may persevere for months. In rare situations, malignancies have been related to the infection.
What are Splenic Ruptures?
Splenic ruptures are ruptures typically due to blunt force trauma that may be direct or indirect. Nontraumatic or spontaneous rupture occurs in an enlarged spleen but rarely in a normal spleen.
What is the Pathology of Splenic Ruptures?
The pathology of splenic ruptures is:
-Etiology: The cause of splenic ruptures is trauma which could be direct or indirect.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to splenic ruptures is trauma and bleeding.
How does Splenic Ruptures Present?
Patients with splenic ruptures typically according to studies suggest that traumatic splenic ruptures are more probable to occur in males (2:1 male to female ratio) in ages ranging from 18 to 34 years. The symptoms, features, and clinical findings associated with splenic ruptures include tachycardia, tachypnea, restlessness, anxiety, decreased capillary refill, and decreased pulse pressure. Complaint of left upper quadrant abdominal tenderness with minor focal injury to the spleen may also be present.
How is Splenic Ruptures Diagnosed?
Splenic ruptures is diagnosed through history and physical examination, imaging studies, and laboratory studies. Imaging such as focused abdominal sonographic technique (FAST scan), CT scanning, angiography, and MRI may be helpful. Laboratory tests, complete blood cell count, or hemoglobin level help provide baseline values.
How is Splenic Ruptures Treated?
Splenic ruptures is treated via Interventional radiology (splenic angioembolization), or surgical therapy (emergency celiotomy or splenorrhaphy).
What is the Prognosis of Splenic Ruptures?
The prognosis of splenic ruptures is good. Prognosis is usually excellent, but those patients left asplenic by their injuries and surgery increase the risk of fatal and debilitating infection for the remainder of their lives.
What are Neoplasms of the Spleen?
Neoplasms of the spleen are typically lymphomas or leukemias.
What is Splenic Lymphoma?
Splenic lymphoma is an indolent B-cell malignancy typically relating to the spleen, bone marrow, and blood. It is one of the distinct types of marginal zone lymphomas.
What is the Pathology of Splenic Lymphoma?
The pathology of splenic lymphoma is:
-Etiology: The cause of splenic lymphoma is not usually clear, although it has been linked with those who have been detected with the hepatitis C virus (HCV) and/or other autoimmune syndromes.
-Genes involved: BIRC3-MALT1, Bcl-10, MALT1, and FOXP1.
-Pathogenesis: The sequence of events that lead to splenic lymphoma is, lymphoma grows in the white pulp with the biphasic picture. The Medium-size monocytoid B-cells are prearranged into the pale ring around the follicle containing an MZ pattern, while small centrocyte-like cells obliterate the mantle zone and take possession of the germinal centers. An Inconstant degree of plasmacytic diversity might be present. Lymphoma cells might comprise the red pulp irregularly or diffusely, with successive spread to the sinuses.
How does Splenic Lymphoma Present?
Patients with splenic lymphoma typically, affect both men and women, although more common in men. Present at an age range of middle-aged or elderly, with the average age at diagnosis of 65 years. The symptoms, features, and clinical findings associated with splenic lymphoma include an enlarged spleen (splenomegaly), B symptoms (night sweats, persistent fevers, unexplained weight loss), thrombocytopenia, and anemia.
How is Splenic Lymphoma Diagnosed?
Splenic lymphoma is diagnosed can be detected using a combination of blood tests complete blood count (CBC) and a bone marrow biopsy.
How is Splenic Lymphoma Treated?
Splenic lymphoma is treated through surgical therapy (splenectomy) followed by long-term antibiotic treatment, chemotherapy regimen. Other standard treatment options include radiotherapy to the spleen, rituximab with or without chemotherapy, or chemo-immunotherapy combinations, rituximab, and chlorambucil. Treatment varies depending on the stage and what symptoms are present.
What is the Prognosis of Splenic Lymphoma?
The prognosis of splenic lymphoma is good it responds well to treatment. However, since it is indolent lymphoma, splenic lymphoma often relapses.
For more information on lymphomas refer to white blood cell pathology.