Stress related mucosal disease is a stress-related injury superficial mucosal damage and stress ulcers focal deep mucosal damage. Both types are caused by mucosal ischemia, and both show a propensity for the acid-producing corpus and fundus.
What is the Pathology of Stress-Related Mucosal Disease?
The pathology of stress-related mucosal disease is:
-Etiology: The cause of stress-related mucosal disease is mucosal erosions and superficial hemorrhages in patients who are critically ill or in those who are under extreme physiologic stress, resulting in minimal-to-severe.
-Genes involved: HSP-70.
-Pathogenesis: The sequence of events that lead to stress-related mucosal disease are gastric mucosal injury which is most often due to local ischemia. Upregulation and increased release of the vasoconstrictor endothelin-1 also contributes to ischemic gastric mucosal injury while increased COX-2 expression appears to be protective. Systemic acidosis may also contribute to mucosal injury by lowering the intracellular pH of mucosal cells.
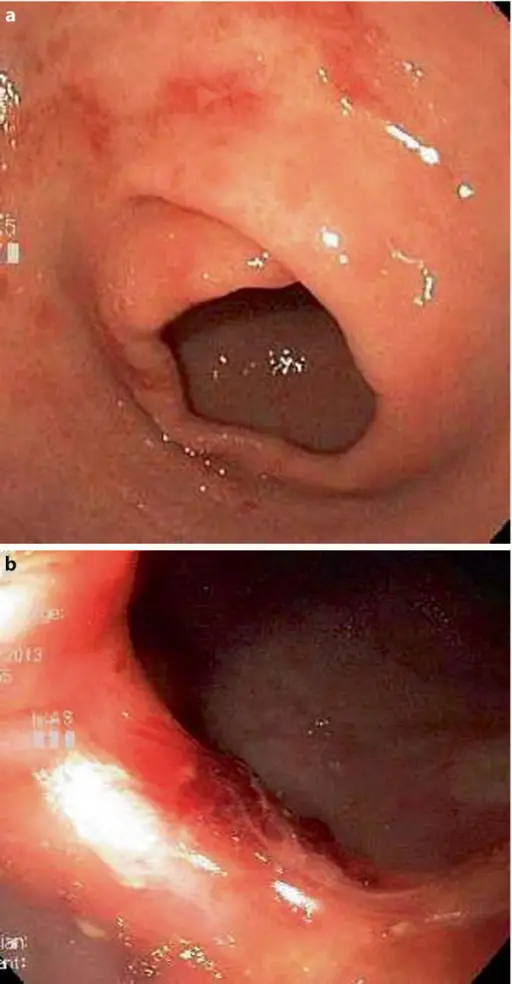
-Histology: The histology associated with stress-related mucosal disease are: shallow erosions to deeper lesions that involve the entire mucosal thickness true ulceration.
How does Stress-Related Mucosal Disease Present?
Patients with stress-related mucosal disease typically all genders of any age but more in people with age >50 years. The symptoms, features, and clinical findings associated with stress-related mucosal disease include: Acute gastroduodenal lesions related to severe sepsis. Respiratory failure, hypotension, sepsis, and jaundice, sepsis and gastrointestinal bleeding.
How is Stress-Related Mucosal Disease Diagnosed?
Stress-related mucosal disease is diagnosed by endoscopy.
How is Stress-Related Mucosal Disease Treated?
Stress-related mucosal disease is treated by antacids, cimetidine, and other histamine H2-receptor antagonists, and vigorous acid suppression.
What is the Prognosis of Stress-Related Mucosal Disease?
The prognosis of disease in lower case is good. Mortality is increased in people with clinically significant bleeding compared to those patients who do not bleed. Institution of prophylaxis is recommended in high-risk patients.