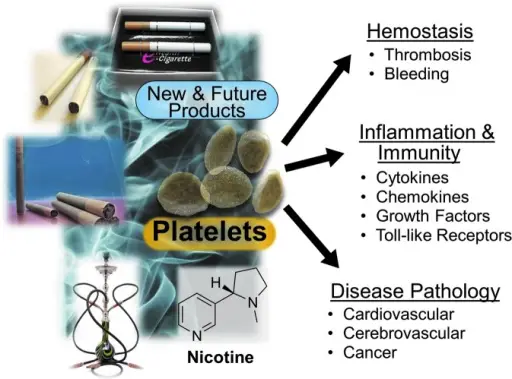
Hemostasis: Integrity of the blood vessel is necessary to carry blood tissues. Damage to the vascular wall is repaired by hemostasis, which involves the formation of a thrombus at the site of vessel injury. Hemostasis has two phases: Primary and Secondary. Primary hemostasis is mediated by the interaction between platelets and the vessel wall to form a weak platelet plug. Secondary hemostasis is mediated by the coagulation cascade and stabilizes the platelet plug.
Hemostasis is the process of preventing blood loss which depends on vascular endothelium, platelets, and the coagulation cascade.
What is Primary Hemostasis?
Primary hemostasis is the formation of the initial platelet plug.
There are four steps are four steps of primary hemostasis, and are as follows:
Step 1: Transient vasoconstriction of the damaged vessel wall that is mediated by stimulation and endothelin release from endothelial cells
Step 2: Platelet adhesion to the surface of damaged vessel. Von Willebrand factor (vWF) binds exposed subendothelial collagen. Platelets bind vWF using the GPIb receptor.
Step 3: Platelet degranulation. Adhesion causes shape change in platelets and degranulation with release of multiple mediators. ADP is released from platelet dense granules which promotes exposure of GPIIb/ IIIa receptor on platelets. TXA2 is synthesized by platelet cyclooxygenase (COX) and released; promotes platelet aggregation
Step 4: Platelet aggregation. Platelets aggregate at the site of injury via GPIIb/IIIa using fibrinogen as a linking molecule which results in formation of a weak platelet plug.
Secondary Hemostasis: Stabilizes the weak platelet plug that is produced by primary hemostasis via the coagulation cascade. The coagulation cascade produces thrombin, which converts fibrinogen in the platelet plug to fibrin. Cross linking of fibrin occurs, which stabilizes the platelet-fibrin thrombus. Factors of the coagulation cascade are produced by the liver in an inactive state. Activation requires exposure to an activating substance, calcium, and platelets.
What are Disorders of Primary Hemostasis?
Disorders of primary hemostasis are due to abnormalities in platelets.
Examples of disorders of primary hemostasis include:
- Immune thrombocytopenic purpura
- Microangiopathic hemolytic anemia
- Qualitative platelet disorders
What is Immune Thrombocytopenic Purpura?
Immune thrombocytopenic purpura is an acquired autoimmune bleeding disorder characterized by isolated thrombocytopenia (peripheral blood platelet count < 100 × 109/L).
What is the Pathology of Immune Thrombocytopenic Purpura?
The pathology of immune thrombocytopenic purpura is:
-Etiology: The cause of immune thrombocytopenic purpura is autoantibodies against platelet antigens. It may be triggered by drugs, infections, or lymphomas, or may be idiopathic.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to immune thrombocytopenic purpura shows impairment in CD4+ T regulatory cells and dendritic cells leads to the initiation and perpetuation of ITP. Thrombocytopenia due to IgG antiplatelet autoantibodies (principal mechanism) bind to platelet surface antigens such as glycoprotein.
-Histology: The histology associated with immune thrombocytopenic purpura shows splenic white pulp is prominent, with focal germinal centers and hyperplastic marginal zones.
How does Immune Thrombocytopenic Purpura Present?
Patients with immune thrombocytopenic purpura typically affect women present at the age range of 20-40 years. The symptoms, features, and clinical findings associated with immune thrombocytopenic purpura include petechiae, easy bruising, epistaxis, gum bleeding, and hemorrhages after minor trauma. Fortunately, more serious intracerebral or subarachnoid hemorrhages are uncommon.
How is Immune Thrombocytopenic Purpura Diagnosed?
Immune thrombocytopenic purpura is diagnosed based on the clinical features, the presence of thrombocytopenia, examination of the marrow, and the exclusion of secondary ITP. Reliable clinical tests for antiplatelet antibodies are not available.
How is Immune Thrombocytopenic Purpura Treated?
Immune thrombocytopenic purpura is treated with corticosteroids, intravenous immunoglobulin, and anti-D immunoglobulin.
What is the Prognosis of Immune Thrombocytopenic Purpura?
The prognosis of immune thrombocytopenic purpura is good with platelet count returning to normal within 6 to 12 months.
What is Microangiopathic Hemolytic Anemia?
Microangiopathic hemolytic anemia is the loss of red blood cells through the destruction caused by factors in the small blood vessels.
What is the Pathology of Microangiopathic Hemolytic Anemia?
The pathology of microangiopathic hemolytic anemia is:
-Etiology: The cause of microangiopathic hemolytic anemia is the factors in the small blood vessels.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to microangiopathic hemolytic anemia includes the formation of a fibrin mesh due to increased activation of the system of coagulation.
-Histology: The histology associated with microangiopathic hemolytic anemia shows fragmented, distorted red blood cells (schistocytes) on the peripheral blood smear.
How does Microangiopathic Hemolytic Anemia Present?
Patients with microangiopathic hemolytic anemia typically affect females present at the age range of 20-50 years. The symptoms, features, and clinical findings associated with microangiopathic hemolytic anemia include schistocytes, bleeding, thrombosis, fatigue, pallor, palpitations, jaundice, and scleral icterus.
How is Microangiopathic Hemolytic Anemia Diagnosed?
Microangiopathic hemolytic anemia is diagnosed using a complete blood count.
How is Microangiopathic Hemolytic Anemia Treated?
Microangiopathic hemolytic anemia is treated with plasmapheresis and corticosteroids.
What is the Prognosis of Microangiopathic Hemolytic Anemia?
The prognosis of microangiopathic hemolytic anemia is poor with a mortality rate of 90% if left untreated.
What is Qualitative Platelet Disorders?
Qualitative platelet disorders is a disorder affecting the structure or function of platelets.
What is the Pathology of Qualitative Platelet Disorders?
The pathology of qualitative platelet disorders is:
-Etiology: The cause of qualitative platelet disorders is von Willebrand disease or absence of thrombocytopenia.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to qualitative platelet disorders includes deficiency or abnormality in the platelet granules or their contents also known as a storage pool disorder.
-Histology: The histology associated with qualitative platelet disorders shows the cytoplasmic granules, platelet membranes, and the cytoskeleton.
How does Qualitative Platelet Disorders Present?
Patients with qualitative platelet disorders typically affect both males and females present at the age range of 3-50 years. The symptoms, features, and clinical findings associated with qualitative platelet disorders include easy bruising, nosebleeds, bleeding of the mouth or gums, heavy menstrual bleeding, postpartum (after childbirth) bleeding, bleeding following dental work, and bleeding with invasive surgical procedures.
How is Qualitative Platelet Disorders Diagnosed?
Qualitative platelet disorders is diagnosed using blood tests.
How is Qualitative Platelet Disorders Treated?
Qualitative platelet disorders is treated with platelet transfusions or plasma exchange along with medications.
What is the Prognosis of Qualitative Platelet Disorders?
The prognosis of qualitative platelet disorders is poor with an increased mortality rate.
What are Disorders of Secondary Hemostasis?
Disorders of secondary hemostasis are caused by failure of fibrin clot formation due to deficiency of one or more coagulation factors. Disorders of secondary hemostasis can be due to factor abnormalities.
Examples of disorders of secondary hemostasis include:
- Hemophilia A
- Hemophilia B
- Coagulation factor inhibitor
- Von willebrand disease
- Disorder of hemostasis due to vitamin K deficiency
- Liver failure related disorder of hemostasis
- Large volume transfusion related disorder of hemostasis
What is Hemophilia A?
Hemophilia A is the most common hereditary cause of serious bleeding. It is an X-linked recessive disorder caused by reduced factor VIII activity.
What is the Pathology of Hemophilia A?
The pathology of hemophilia a is:
-Etiology: The cause of hemophilia a is mutations in factor VIII.
-Genes involved: F8.
-Pathogenesis: The sequence of events that lead to hemophilia a includes the deficit in factor VIII, or by an acquired inhibitor that binds factor VIII.
-Histology: The histology associated with hemophilia a shows missing factor VIII and hemarthrosis.
How does Hemophilia A Present?
Patients with hemophilia a typically affect the male present in the age range of 26-45 years. The symptoms, features, and clinical findings associated with hemophilia include spontaneous hemorrhages in joints, muscles and with life-threatening hemorrhage, and petechiae.
How is Hemophilia A Diagnosed?
Hemophilia a is diagnosed with specific assays for factor VIII.
How is Hemophilia A Treated?
Hemophilia a is treated with factor VIII infusions.
What is the Prognosis of Hemophilia A?
The prognosis of hemophilia a is poor with 50-60% of people having a severe form of the disorder.
What is Hemophilia B?
Hemophilia B is an X-linked disorder having severe factor IX deficiency.
What is the Pathology of Hemophilia B?
The pathology of hemophilia B is:
-Etiology: The cause of hemophilia b is mutations in coagulation factor IX.
-Genes involved: F9.
-Pathogenesis: The sequence of events that lead to hemophilia b includes the deficit in factor IX, or by an acquired inhibitor that binds factor IX.
-Histology: The histology associated with hemophilia b shows missing factor IX and hemarthrosis.
How does Hemophilia B Present?
Patients with hemophilia b typically affect males present at the age range of 26-45 years. The symptoms, features, and clinical findings associated with hemophilia b include spontaneous hemorrhages in joints, and petechiae.
How is Hemophilia B Diagnosed?
Hemophilia B is diagnosed using specific assays of factor IX.
How is Hemophilia B Treated?
Hemophilia b is treated by infusion of recombinant factor IX.
What is the Prognosis of Hemophilia B?
The prognosis of hemophilia b is poor with a life expectancy of fewer than 10 years with proper treatment.
What is Coagulation Factor Inhibitor Related Disorder of Hemostasis?
Coagulation factor inhibitor related disorder of hemostasis are antibodies that either inhibit the activity or increase the clearance of a clotting factor.
What is the Pathology of Coagulation Factor Inhibitor Related Disorder of Hemostasis?
The pathology of coagulation factor inhibitor-related disorder of hemostasis is:
-Etiology: The cause of coagulation factor inhibitor-related disorder of hemostasis is immune-mediated depletion or inhibition of a coagulation factor.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to coagulation factor inhibitor-related disorder of hemostasis shows that specific or non-specific autoantibodies generate immune complexes with vWF, increasing its clearance from the circulation.
How does Coagulation Factor Inhibitor Related Disorder of Hemostasis Present?
Patients with coagulation factor inhibitor-related disorder of hemostasis typically affect males and females both present at the age range of 26-45 years. The symptoms, features, and clinical findings associated with coagulation factor inhibitor-related disorder of hemostasis include hemorrhage, bleeding disorders, and bleeding diathesis.
How is Coagulation Factor Inhibitor Related Disorder of Hemostasis Diagnosed?
Coagulation factor inhibitor-related disorder of hemostasis is diagnosed by doing a complete blood count.
How is Coagulation Factor Inhibitor Related Disorder of Hemostasis Treated?
Coagulation factor inhibitor-related disorder of hemostasis is treated with DDAVP, FVIII infusions, and bypassing agents.
What is the Prognosis of Coagulation Factor Inhibitor Related Disorder of Hemostasis?
The prognosis of coagulation factor inhibitor-related disorder of hemostasis is fair if treated properly in a timely manner.
What is Von Willebrand Disease?
Von Willebrand disease is an autosomal dominant disorder caused by mutations in vWF, a large protein that promotes the adhesion of platelets to subendothelial collagen.
What is the Pathology of Von Willebrand Disease?
The pathology of von willebrand disease is:
-Etiology: The cause of von willebrand disease is mutation in vWF protein.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to von willebrand disease is due to an abnormality, either quantitative or qualitative, of the von Willebrand factor, which is a large multimeric glycoprotein required for normal platelet adhesion.
-Histology: The histology associated with von willebrand disease shows mucocutaneous hemorrhage and decreased factor VIII.
How does Von Willebrand Disease Present?
Patients with von willebrand disease typically have no gender preference. The symptoms, features, and clinical findings associated with von willebrand disease include epistaxis, easy bruising, bleeding, menorrhagia. It has similar symptoms as platelet function defects.
How is Von Willebrand Disease Diagnosed?
Von willebrand disease is diagnosed by testing factor VIII activity, vWF antigen, vWF activity often done by ristocetin cofactor assay.
How is Von Willebrand Disease Treated?
Von Willebrand disease is treated with DDAVP (desmopressin). It temporarily increases vWF and factor VIII levels 2 – 3x.
What is the Prognosis of Von Willebrand Disease?
The prognosis of von willebrand disease is poor because it’s a lifelong condition.
What is Disorder of Hemostasis due to Vitamin K Deficiency?
Disorder of hemostasis due to vitamin K deficiency is the hemostatic disease due to vitamin K deficiency.
What is the Pathology of Disorder of Hemostasis due to Vitamin K Deficiency?
The pathology of disorder of hemostasis due to vitamin k deficiency is:
-Etiology: The cause of disorder of hemostasis due to vitamin k deficiency isn’t clear but considered obstructive jaundice as one of the causes.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to disorder of hemostasis due to vitamin k deficiency shows the deficiency of the proteins that require vitamin K for their synthesis, including prothrombin, factor X, factor IX, and factor VII.
How does Disorder of Hemostasis due to Vitamin K Deficiency Present?
Patients with disorder of hemostasis due to vitamin k deficiency typically newborn males and females present at the range of over 65 years. The symptoms, features, and clinical findings associated with disorder of hemostasis due to vitamin k deficiency include hemorrhage, bruises, Easy bruising, soft tissue hematoma, gastrointestinal bleeding, epistaxis, intracranial bleeding, hematuria, hemoptysis, intraperitoneal and retroperitoneal bleeding.
How is Disorder of Hemostasis due to Vitamin K Deficiency Diagnosed?
Disorder of hemostasis due to vitamin k deficiency is diagnosed using blood tests.
How is Disorder of Hemostasis due to Vitamin K Deficiency Treated?
Disorder of hemostasis due to vitamin k deficiency is treated by giving vitamin K once, then 12 – 24 hours later, then measuring PT (should normalize).
What is the Prognosis of Disorder of Hemostasis due to Vitamin K Deficiency?
The prognosis of disorder of hemostasis due to vitamin k deficiency is fair if treated in a timely manner.
What is Liver Failure Related Disorder of Hemostasis?
Liver failure related disorder of hemostasis is the hemostatic disease due to liver dysfunction.
What is the Pathology of Liver Failure Related Disorder of Hemostasis?
The pathology of liver failure related disorder of hemostasis is:
-Etiology: The cause of liver failure-related disorder of hemostasis is cirrhosis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to liver failure-related disorder of hemostasis shows an imbalanced intestinal homeostasis results in a breach of the gut barrier and subsequent microbial translocation. Microbial translocation is an important pathogenic factor in the progression of chronic liver disease.
-Histology: The histology associated with liver failure related disorder of hemostasis shows panacinar hepatic necrosis with the collapse of the reticulin framework.
How does Liver Failure Related Disorder of Hemostasis Present?
Patients with a liver failure-related disorder of hemostasis typically affects male and female present at the age range of 25-55 years. The symptoms, features, and clinical findings associated with liver failure related disorder of hemostasis include thrombocytopenia, reduced levels of coagulation factors and inhibitors, reduced levels of fibrinolytic proteins, and increased plasma levels of coagulation factor VIII and VWF, jaundice, malaise, ascites, nausea, and vomiting.
How is Liver Failure Related Disorder of Hemostasis Diagnosed?
Liver failure-related disorder of hemostasis is diagnosed using blood tests and liver function tests.
How is Liver Failure Related Disorder of Hemostasis Treated?
Liver failure-related disorder of hemostasis is treated by doing liver transplant, auxiliary partial orthotopic liver transplant, and usual antibiotics.
What is the Prognosis of Liver Failure Related Disorder of Hemostasis?
The prognosis of liver failure-related disorder of hemostasis is poor with an increased mortality rate.
What is Large Volume Transfusion Related Disorder of Hemostasis?
Large volume transfusion-related disorder of hemostasis is the hemostatic disease due to large volume transfusion dysfunction.
What is the Pathology of Large Volume Transfusion Related Disorder of Hemostasis?
The pathology of large volume transfusion-related disorder of hemostasis is:
-Etiology: The cause of large volume transfusion-related disorder of hemostasis is traumatic injury.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to large volume transfusion-related disorder of hemostasis includes severe blood loss leading to the lethal triad of trauma (hypothermia, coagulopathy, and acidosis).
How does Large Volume Transfusion Related Disorder of Hemostasis Present?
Patients with large volume transfusion-related disorder of hemostasis typically affect males and females present at the age range of 25-65 years. The symptoms, features, and clinical findings associated with large volume transfusion-related disorder of hemostasis include hypothermia, dilutional coagulopathy, hypocalcemia, hypomagnesemia, citrate toxicity, metabolic acidosis, hyperkalemia and hypokalaemia, immune hemolysis, and air embolism. Also, fever, chills, urticaria, and nausea.
How is Large Volume Transfusion Related Disorder of Hemostasis Diagnosed?
Large volume transfusion-related disorder of hemostasis is diagnosed using blood tests and coagulation testing.
How is Large Volume Transfusion Related Disorder of Hemostasis Treated?
Large volume transfusion-related disorder of hemostasis is treated with transfusions and antibiotics.
What is the Prognosis of Large Volume Transfusion Related Disorder of Hemostasis?
The prognosis of large volume transfusion-related disorder of hemostasis is poor with an increased mortality rate.
What is Heparin-Induced Thrombocytopenia?
Heparin-induced thrombocytopenia is the development of thrombocytopenia, due to the administration of various forms of heparin.
What is the Pathology of Heparin-Induced Thrombocytopenia?
The pathology of heparin-induced thrombocytopenia is:
-Etiology: The cause of heparin-induced thrombocytopenia is IgG antibodies that bind to platelet factor 4 on platelet membranes in a heparin-dependent fashion.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to heparin-induced thrombocytopenia shows that resultant activation of the platelets induces their aggregation, thereby exacerbating the condition that heparin is used to treat—thrombosis. Both venous and arterial thromboses occur, even in the setting of marked thrombocytopenia.
-Histology: The histology associated with heparin-induced thrombocytopenia shows skin lesions associated with the use of low-molecular-weight heparins.
How does Heparin-Induced Thrombocytopenia Present?
Patients with heparin-induced thrombocytopenia typically affect females present at the age range of over 50. The symptoms, features, and clinical findings associated with heparin-induced thrombocytopenia include that affected patients usually have a reduction in platelet count within 4 – 20 days after heparin exposure for the first time, 1 – 3 days after reexposure to heparin; platelet count typically decreases 50% or more to under 100K. The symptoms include enlargement or extension of a previously diagnosed blood clot, or the development of a new blood clot elsewhere in the body, skin tenderness, swelling, skin that’s warm to the touch, shortness of breath, change in heart rate, sharp pain in chest, dizziness, and anxiety.
How is Heparin-Induced Thrombocytopenia Diagnosed?
Heparin-induced thrombocytopenia is diagnosed using ELISA methodology and 4 T score.
How is Heparin-Induced Thrombocytopenia Treated?
Heparin-induced thrombocytopenia is treated by the cessation of heparin and by using low-molecular-weight heparin preparations.
What is the Prognosis of Heparin-Induced Thrombocytopenia?
The prognosis of heparin-induced thrombocytopenia is poor and can cause severe morbidities such as loss of limb or death.
What is Disseminated Intravascular Coagulation?
Disseminated intravascular coagulation is the sudden or insidious onset of widespread thrombosis within the microcirculation.
What is the Pathology of Disseminated Intravascular Coagulation?
The pathology of disseminated intravascular coagulation is:
-Etiology: The cause of disseminated intravascular coagulation is the systemic activation of thrombin that causes consumptive coagulopathy. It can also be due to sepsis, surgery, major trauma, cancer, and complications of pregnancy.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to disseminated intravascular coagulation includes the release of tissue factor or thromboplastic substances into the circulation or widespread endothelial cell damage.
-Morphology: The morphology associated with disseminated intravascular coagulation shows that microthrombi are most often found in the arterioles and capillaries of the kidneys, adrenals, brain, and heart, but no organ is spared. The glomeruli contain small fibrin thrombi. These may be associated with only a subtle, reactive swelling of the endothelial cells or varying degrees of focal glomerulitis.
-Histology: The histology associated with disseminated intravascular coagulation shows the presence of ischemia and necrosis due to fibrin deposition in small and medium-sized vessels of various organs.
How does Disseminated Intravascular Coagulation Present?
Patients with disseminated intravascular coagulation typically affect males present at the age range of 40 and above, mostly in advanced age. The symptoms, features, and clinical findings associated with disseminated intravascular coagulation include circulatory insufficiency, particularly in the brain, lungs, heart, and kidneys, bleeding diathesis, shock, with acute renal failure, dyspnea, cyanosis, convulsions, and coma, copious postpartum bleeding or by the presence of petechiae and ecchymoses on the skin, severe hemorrhage into the gut or urinary tract.
How is Disseminated Intravascular Coagulation Diagnosed?
Disseminated intravascular coagulation is diagnosed based on prolongation of the prothrombin time, declining platelet count, characteristic history, and peripheral blood smear showing schistocytes.
How is Disseminated Intravascular Coagulation Treated?
Disseminated intravascular coagulation is treated depending upon the underlying cause, plasma transfusion, or fresh frozen plasma, heparin.
What is the Prognosis of Disseminated Intravascular Coagulation?
The prognosis of disseminated intravascular coagulation is fair depending on the nature of the underlying disorder and the severity of the intravascular clotting and fibrinolysis.
What are Disorders of Fibrinolysis?
Disorders of fibrinolysis include:
- Liver cirrhosis
- Amyloidosis
- Acute promyelocytic leukemia