Thromboembolic disease are diseases that result due to the formation of a thrombus or emboli.
What is Virchow’s Triad?
Virchow’s triad describes the three broad categories of factors in the development of venous thrombosis. It is put forward by Rudolf Virchow.
Virchow’s triad summarizes the three major risk factors for thrombosis which includes:
- Hypercoagulable state
- Disruption in blood flow
- Endothelial cell damage
What is a Hypercoagulable State?
Hypercoagulable state is an increased tendency to develop thrombosis due to the presence of one or more predisposing factors, which can either be inherited or acquired. It can be due to excessive procoagulant proteins or defective anticoagulant proteins.
Conditions that may cause a hypercoagulable state include:
- Coagulopathies
- Malignancies
- Certain medications
What is Disruption of Normal Blood Flow?
Disruption of normal blood flow is the deficient supply of blood to a body part that is mainly due to obstruction of the inflow of arterial blood. There are 2 main types of blood flow found in the human body for instance stasis and turbulence.
What is Endothelial Cell Damage?
Endothelial Cell Damage is due to the direct trauma and/or damage to endothelial cells by hypoxia caused by statis in the presence of activated clotting factors that initiate thrombosis. Also, the endothelial cell damage disrupts the protective function of endothelial cells, increasing the risk for thrombosis.
| Virchow’s Triad | Meaning |
| Hypercoagulable State | Excessive procoagulant proteins or defective anticoagulant proteins. |
| Disruption of Normal Blood Flow | Flow of blood is altered. |
| Stasis | Blood is not flowing. |
What is an Embolism?
An embolism is an intravascular mass that travels and occludes downstream vessels. Symptoms depend on the vessel involved, and may include myocardial infarction or cerebrovascular accidents like stroke.
Types of embolisms include:
- Thromboembolism
- Fat embolism
- Gas embolism
- Amniotic fluid embolism
- Pulmonary embolism
- Systemic embolism
What is Thromboembolism?
Thromboembolism is the obstruction of a blood vessel by a blood clot. It is responsible for approximately 95% of embolisms.
What is the Pathology of Thromboembolism?
The pathology of thromboembolism is:
-Etiology: The cause of thromboembolism is family history, sedentary lifestyle, older age, obesity, smoking, high blood pressure, high cholesterol, and diabetes.
-Genes involved: Certain clotting factor abnormalites may be implicated.
-Pathogenesis: The sequence of events that lead to thromboembolism depends upon Virchow’s triad, i.e, presence of abnormalities of blood flow, blood vessel wall, and blood clotting components.
-Morphology: The morphology associated with thromboembolism shows large embolus may embed in major branches or lodge astride the bifurcation as a saddle embolus.
-Histology: The histology associated with thromboembolism shows necrosis, recanaliztion, irregular, nonlaminar, often obliterative, intimai fibrosis.
How does Thromboembolism Present?
Patients with thromboembolism are typically males as compared to females present at the age range of over 60. The symptoms, features, and clinical findings associated with thromboembolism include heart attack, limb infarction, or even pneumonia, leg pain and tenderness, edema, sense of impending doom, anxiety, red and hot skin, and dilated veins.
How is Thromboembolism Diagnosed?
Thromboembolism is diagnosed using D-dimer blood test, factor VIII blood test, platelet aggregation test, MRI, duplex ultrasound.
How is Thromboembolism Treated?
Thromboembolism is treated with anticoagulants, antiplatelets, and thrombolytics initially, if progressed then surgery is an option.
What is the Prognosis of Thromboembolism?
The prognosis of thromboembolism is fair, with short-term survival ranging from 95% to 97% for deep vein thrombosis, while long-term survival ranges from 61% to 75% for deep vein thrombosis.
What is an Infarction?
An infarction is an ischemic necrosis due to occlusion of venous drainage or arterial supply.
What is a Myocardial Infarction?
Myocardial infarction is the irreversible death of heart muscle secondary to prolonged lack of oxygen supply. It typically occurs due to thromboembolism in a coronary artery.
What is the Pathology of Myocardial Infarction?
The pathology of myocardial infarction is:
-Etiology: The cause of myocardial infarction is coronary artery disease.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to myocardial infarction includes complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque
-Morphology: The morphology associated with myocardial infarction shows early morphologic indicators of irreversible myocardial damage are rupture of the sarcolemma and contraction band necrosis. The size of the infarction increases with the duration of ischemia.
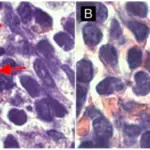
-Histology: The histology associated with myocardial infarction shows left ventricle myocardium with the focus of coagulated necrosis, nuclei are localized in the center of cells.
How does Myocardial Infarction Present?
Patients with myocardial infarction typically affect males present at the age range of 30-64 years. The symptoms, features, and clinical findings associated with myocardial infarction include chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw, heartburn, shortness of breath, nausea, feeling faint, a cold sweat, or feeling tired.
How is Myocardial Infarction Diagnosed?
Myocardial infarction is diagnosed using ECG, blood tests (troponin), and coronary angiography.
How is Myocardial Infarction Treated?
Myocardial infarction is treated with aspirin, nitroglycerin, and opioids, supplemental oxygen, percutaneous coronary intervention, coronary artery bypass surgery, and angioplasty.
What is the Prognosis of Myocardial Infarction?
The prognosis of myocardial infarction is fair with a 30% mortality rate; about 50% of the deaths occur prior to arrival at the hospital. An additional 5-10% of survivors die within the first year after their myocardial infarction.
What is Fat Embolism?
Fat embolism is a rare form of embolism that often results from multiple fractures or a fracture of the femur. Fat droplets enter the vein from bone marrow or surrounding adipose tissue.
What is the Pathology of Fat Embolism?
The pathology of fat embolism is:
-Etiology: The cause of fat embolism is trauma with long bone fractures, extensive soft tissue trauma, burn injuries, severe fatty liver, and very rarely with orthopedic procedures.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to depot-derived fat embolism arises by disruption of depot fat, usually as a result of trauma, allowing direct entry into the bloodstream. Plasma-derived fat embolism is caused by agglutination of endogenous or infused exogenous fat such as Intralipid, with consequent embolism.
-Morphology: The morphology associated with fat embolism shows platelet activation and granulocyte recruitment (with free radical, protease, and eicosanoid release), complete the vascular assault
-Histology: The histology associated with fat embolism shows microscopic fat globules, fat and marrow emboli
How does Fat Embolism Present?
Patients with fat embolism typically affect males present at the age range of 20-30 years. The symptoms, features, and clinical findings associated with fat embolism include rapid breathing, shortness of breath, mental confusion, lethargy, coma, petechial rash, fever, and anemia.
How is Fat Embolism Diagnosed?
Fat embolism is diagnosed using Gurd’s criteria (petechial rash, respiratory distress, mental concussion).
How is Fat Embolism Treated?
Fat embolism is treated using supportive care, supplemental oxygen, heparin, and steroids.
What is the Prognosis of Fat Embolism?
The prognosis of fat embolism is fair with almost 80% of people fully recovering with no lasting side effects.
What is Gas Embolism?
Gas embolism occurs when air travels through the vascular system. It can occur in decompression sickness (the bends) when divers ascend too quickly. It can also (very rarely) occur if air enters the arterial or venous system through surgery or during a clinical procedure (e.g., cannulation).
What is the Pathology of Gas Embolism?
The pathology of gas embolism is:
-Etiology: The cause of gas embolism is injections and surgical procedures, lung trauma, scuba diving, explosion and blast injuries,
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gas embolism occurs whenever a blood vessel is open and a pressure gradient exists favoring the entry of gas.
-Morphology: The morphology associated with gas embolism shows decompression sickness, the bends, and the chokes.
-Histology: The histology associated with gas embolism show multifocal ischemic necrosis.
How does Gas Embolism Present?
Patients with gas embolism typically affect females present at the age range of 50-70 years. The symptoms, features, and clinical findings associated with gas embolism include hypotension, shortness of breath, vertigo, loss of consciousness, convulsions, numbness, loss of coordination, bloody sputum. Symptoms of other consequences of lung over expansion such as pneumothorax, subcutaneous or mediastinal emphysema may also be present.
How is Gas Embolism Diagnosed?
Gas embolism is diagnosed by doing a physical examination, ultrasound, and CT scan.
How is Gas Embolism Treated?
Gas embolism is treated with Trendelenburg position and left lateral decubitus position initially. Therapeutic recompression, and hyperbaric oxygen may be used as well.
What is the Prognosis of Gas Embolism?
The prognosis of gas embolism is good if treated early, however, the large air embolism might be fatal.
What is Amniotic Fluid Embolism?
Amniotic fluid embolism is a sudden and unexpected life-threatening birth complication that can affect both mother and baby.
What is the Pathology of Amniotic Fluid Embolism?
The pathology of amniotic fluid embolism is:
-Etiology: The cause of amniotic fluid embolism is the breakdown in the placental barrier, such as from trauma
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to amniotic fluid embolism is not clear. A possible cause is that any breach of the barrier between maternal blood and amniotic fluid forces the entry of amniotic fluid into the systemic circulation and results in a physical obstruction of the pulmonary circulation.
-Morphology: The morphology associated with amniotic fluid embolism shows that during labor, if the placental membranes tear at the same time the uterine veins rupture, then amniotic fluid can get into the bloodstream and travels to the lungs.
-Histology: The histology associated with amniotic fluid embolism shows fetal debris, epithelial squames in a peripheral pulmonary artery.
How does Amniotic Fluid Embolism Present?
Patients with amniotic fluid embolism typically affect females present at the age range of 35 and above. The symptoms, features, and clinical findings associated with amniotic fluid embolism include sudden shortness of breath, pulmonary edema, sudden low blood pressure, cardiovascular collapse, disseminated intravascular coagulopathy, bleeding from the uterus, cesarean incision or intravenous (IV) sites, altered mental state, fetal distress, seizures, and loss of consciousness.
How is Amniotic Fluid Embolism Diagnosed?
Amniotic fluid embolism is diagnosed using blood tests, ECG, pulse oximetry, chest X-ray, and echocardiogram.
How is Amniotic Fluid Embolism Treated?
Amniotic fluid embolism is treated with catheter placement as an emergency treatment, others include supplemental oxygen, medications, and blood/fluid transfusions.
What is the Prognosis of Amniotic Fluid Embolism?
The prognosis of amniotic fluid embolism is very poor as most women do not survive.
What is Pulmonary Embolism?
Pulmonary embolism is a common and serious clinical complication of DVT, resulting from fragmentation or detachment of the venous thrombus.
What is the Pathology of Pulmonary Embolism?
The pathology of pulmonary embolism is:
-Etiology: The cause of pulmonary embolism is venous thromboembolism (VTE) arising from the deep veins of the lower limbs.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pulmonary embolism includes deep venous thrombi to detach and embolize to the pulmonary circulation. The most common source is deep venous thrombus (DVT) of the lower extremity. Pulmonary infarction can occur if a large or medium-sized artery is obstructed. Ten percent of pulmonary embolisms cause infarction.
-Morphology: The morphology associated with pulmonary embolism shows wedge-shaped, hemorrhagic parenchyma and fibrinous pleural exudate which may eventually scar.
-Histology: The histology associated with pulmonary embolism shows neutrophils present if septic emboli and ischemic necrosis of the lung substance within the area of hemorrhage, affecting the alveolar walls, bronchioles, and vessels.
How does Pulmonary Embolism Present?
Patients with pulmonary embolism typically affect males present at the age range of 40 and above, mostly in the advanced age. The symptoms, features, and clinical findings associated with pulmonary embolism include pleuritic chest pain (sharp & stabbing pain, well localized, exacerbated by deep inspiration), breathlessness, hemoptysis, collapse, tachycardia, and hypotension.
How is Pulmonary Embolism Diagnosed?
Pulmonary embolism is diagnosed using CT scan, D dimer test, Ventilation-perfusion scan, and pulmonary angiogram.
How Is Pulmonary Embolism Treated?
Pulmonary embolism is treated with anticoagulants and thrombolytics.
What is the Prognosis of Pulmonary Embolism?
The prognosis of pulmonary embolism is poor with 20-30% affecting more in men as compared to women.
What is Systemic Embolism?
Systemic embolism refers to the emboli in the arterial circulation. It usually occurs due to thromboembolism. Most commonly originate in the left heart.
What is the Pathology of Systemic Embolism?
The pathology of systemic embolism is:
-Etiology: The cause of systemic embolism is aortic aneurysm, artificial heart valves, ulcerated atherosclerotic plaques, and infective endocarditis
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to systemic embolism includes the formation of intracardiac thrombi after classical heart transplantation are presumably the enlarged left atria, the non-contractile portion of recipient atrium, and the asynchrony between the donor and the recipient atria which encourages stasis.
-Morphology: The morphology associated with systemic embolism shows origination from aortic aneurysms, thrombi overlying ulcerated atherosclerotic plaques, fragmented valvular vegetations.
-Histology: The histology associated with systemic embolism shows ischemic necrosis.
How does Systemic Embolism Present?
Patients with systemic embolism typically affect males present in the age range of 50 and above. The symptoms, features, and clinical findings associated with systemic embolism include shortness of breath, tachycardia, altered mental state, nausea, vomiting, however, most patients are asymptomatic too.
How is Systemic Embolism Diagnosed?
Systemic embolism is diagnosed using a thoracic CT scan or TEE.
How is Systemic Embolism Treated?
Systemic embolism is treated with anticoagulants and thrombolytics, surgical intervention.
What is the Prognosis of Systemic Embolism?
The prognosis of systemic embolism is poor with an increased mortality rate.
What is Antiphospholipid Syndrome?
Antiphospholipid syndrome is an autoimmune disorder that causes an increased risk of blood clots.
What is the Pathology of Antiphospholipid Syndrome?
The pathology of antiphospholipid syndrome is:
-Etiology: The cause of the antiphospholipid syndrome is genetics
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to antiphospholipid syndrome includes antiphospholipid antibodies to react against proteins that bind to anionic phospholipids on plasma membranes.
-Morphology: The morphology associated with antiphospholipid syndrome shows necrosis, vascular thrombosis, proliferation, and sclerosis in the absence of inflammation.
-Histology: The histology associated with antiphospholipid syndrome shows noninflammatory bland thrombosis with no signs of perivascular inflammation or leukocytoclastic vasculitis.
How does Antiphospholipid Syndrome Present?
Patients with antiphospholipid syndrome typically affect females present at the age range of 30-45 years. The symptoms, features, and clinical findings associated with the antiphospholipid syndrome include deep vein thrombosis, stroke, recurrent miscarriage, intrauterine growth restriction, preterm birth, developmental retardation in newborns, low platelet count, heart valve disease, and livedo reticularis.
How is Antiphospholipid Syndrome Diagnosed?
Antiphospholipid syndrome is diagnosed with blood tests.
How is Antiphospholipid Syndrome Treated?
Antiphospholipid syndrome is treated with anticoagulants such as heparin.
What is the Prognosis of Antiphospholipid Syndrome?
The prognosis of antiphospholipid syndrome is very poor with a high mortality rate.
What is thrombosis?
Thrombosis is the formation of a blood clot within a blood vessel. It prevents blood from flowing normally through the circulatory system.
What is the Pathology of Thrombosis?
The pathology of thrombosis is:
-Etiology: The cause of thrombosis is Virchow’s triad issues.
-Genes involved: Certain clotting factors may be implicated.
-Pathogenesis: The sequence of events that lead to thrombosis formation begins when platelets bind to collagen exposed at the site of vascular injury. Such binding leads to platelet activation, as a result of which platelet membranes acquire the ability to provide catalytic support for the biochemical reactions that lead to thrombin formation
-Morphology: The morphology associated with thrombosis shows variable size and shape, may develop anywhere in the cardiovascular system, occurs in sites of stasis, firmly attached to the point of origin.
-Histology: The histology associated with thrombosis shows attachment to the vessel wall, and Lines of Zahn.
How does Thrombosis Present?
Patients with thrombosis typically affect males present at the age range of 40 and above, mostly in advanced age. The symptoms, features, and clinical findings associated with thrombosis include warm skin around the painful area, throbbing or cramping pain most common location is the deep veins (DVT) of the leg below the knee, which can occur in an artery or vein, swollen veins that are hard or sore when you touch them, warm skin around the area.
How is Thrombosis Diagnosed?
Thrombosis is diagnosed using blood tests, ultrasound, venography, CT scan, and MRI.
How is Thrombosis Treated?
Thrombosis is treated with anticoagulants, catheters, stents.
What is the Prognosis of Thrombosis?
The prognosis of thrombosis is good and resolves completely with no complication.
What is Disseminated Intravascular Coagulation?
Disseminated Intravascular Coagulation is the sudden or insidious onset of widespread thrombosis within the microcirculation.
What is the Pathology of Disseminated Intravascular Coagulation?
The pathology of disseminated intravascular coagulation is:
-Etiology: The cause of disseminated intravascular coagulation is the systemic activation of thrombin that causes consumptive coagulopathy. It can also be due to sepsis, surgery, major trauma, cancer, and complications of pregnancy
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to disseminated intravascular coagulation includes the release of tissue factor or thromboplastic substances into the circulation or widespread endothelial cell damage
-Morphology: The morphology associated with disseminated intravascular coagulation shows that microthrombi are most often found in the arterioles and capillaries of the kidneys, adrenals, brain, and heart, but no organ is spared. The glomeruli contain small fibrin thrombi. These may be associated with only a subtle, reactive swelling of the endothelial cells or varying degrees of focal glomerulitis
-Histology: The histology associated with disseminated intravascular coagulation shows the presence of ischemia and necrosis due to fibrin deposition in small and medium-sized vessels of various organs.
How does Disseminated Intravascular Coagulation Present?
Patients with disseminated intravascular coagulation typically affect males present at the age range of 40 and above, mostly in advanced age. The symptoms, features, and clinical findings associated with disseminated intravascular coagulation include circulatory insufficiency, particularly in the brain, lungs, heart, and kidneys, bleeding diathesis, shock, with acute renal failure, dyspnea, cyanosis, convulsions, and coma, copious postpartum bleeding or by the presence of petechiae and ecchymoses on the skin, severe hemorrhage into the gut or urinary tract.
How is Disseminated Intravascular Coagulation Diagnosed?
Disseminated intravascular coagulation is diagnosed based on prolongation of the prothrombin time, declining platelet count, characteristic history, and peripheral blood smear showing schistocytes.
How is Disseminated Intravascular Coagulation Treated?
Disseminated intravascular coagulation is treated depending upon the underlying cause, plasma transfusion, or fresh frozen plasma, heparin.
What is the Prognosis of Disseminated Intravascular Coagulation?
The prognosis of disseminated intravascular coagulation is fair depending on the nature of the underlying disorder and the severity of the intra vascular clotting and fibrinolysis.