Thyroid gland pathology is the study of diseases related to the thyroid gland.
Common thyroid issues include:
- Hyperthyroidism
- Hypothyroidism
- Thyroiditis
- Graves disease
- Diffuse goiters
- Multinodular goiters
- Neoplasms of the thyroid
What is Hyperthyroidism?
Hyperthyroidism is a set of disorders that involve excess synthesis and secretion of thyroid hormones by the thyroid gland. Hyperthyroidism may be seen in conditions such as Graves disease, multinodular goiter, and thyroid adenoma.
Examples of hyperthyroidism include:
- Thyrotoxicosis
- Primary hyperthyroidism
- Secondary hyperthyroidism
What is thyrotoxicosis?
Thyrotoxicosis is the clinical manifestation of excess thyroid hormone action at the tissue level due to inappropriately high circulating thyroid hormone concentrations.
Pathology: Thyrotoxicosis is mainly due to the release of preformed thyroid hormone into the circulation as inflammation destroys thyroid follicles.
Presentation: Thyrotoxicosis usually presents with heat intolerance associated with increased sweating, weight loss with a normal or increased appetite, palpitations, tremor, anxiety, proximal muscle weakness, alopecia and increased fatiguability.
Diagnosis: Thyrotoxicosis diagnosis is usually made through thyroid function tests including TSH, T3, FT4.
Treatment: Thyrotoxicosis is treated by symptomatic management. These may include beta-blockers and radioactive iodine.
Prognosis: Thyrotoxicosis prognosis good, but if thyrotoxicosis is not treated properly delirium, altered mental status, osteoporosis, muscle weakness, atrial fibrillation, may occur.
What is Primary Hyperthyroidism?
Primary hyperthyroidism occurs when the thyroid gland is the source of abnormal thyroid hormone production.
Pathology: Low TSH, high free T4, normal TRH stimulation test.
Presentation: Patients with primary hyperthyroidism may present with cardiovascular issues such as tachycardia or atrial fibrillation, eyelid spasms, thyroidgoiters, and heat intolerance.
Diagnosis: A blood test to measure TSH level
Treatment: Anti-thyroid drug.
Prognosis: Prognosis of primary hyperthyroidism is good with symptoms starting to resolve within several weeks.
What is Secondary Hyperthyroidism?
Secondary Hyperthyroidism occurs when the thyroid gland is stimulated by excessive thyroid-stimulating hormone.
Pathology: High TSH, abnormal TRH stimulation test.
Presentation: Patients with secondary hyperthyroidism may present with nervousness, weight loss, sweating, palpitations, tremor, diarrhea, heat intolerance, fatigue, loss of libido, and oligomenorrhea.
Diagnosis: A blood test to measure TSH level.
Treatment: Antithyroid drug and surgery.
Prognosis: Prognosis is good with symptoms starting to resolve within several weeks.
What is Hypothyroidism?
Hypothyroidism is a condition in which the thyroid gland is not able to produce enough thyroid hormone required for the body. Hypothyroidism may occur due to decreased thyroid hormone due to functional or structural issues. Hypothyroidism may also be due to autoimmune, congenital, or iatrogenic causes.
Pathology: Hypothyroidism may be due to destruction of the thyroid gland which leads to decreased secretion of thyroid hormones T3 and T4.
Presentation: The most common symptoms of hypothyroidism are fatigue, cold sensitivity, dry skin, muscle cramps, voice changes, and constipation. Advanced hypothyrodism signs may include sleep apnea, and pituitary hyperplasia.
Diagnosis: Hypothyroidism is diagnosed by serum thyrotropin (TSH), T3, and T4 levels.
Treatment: Thyroid hormone replacement therapy such as L-thyroxine.
Prognosis: The prognosis of hypothyroidism is good with early treatment if the disease hasn’t progressed to myxedema coma.
What is Cretinism?
Cretinism is a clinical condition characterized by the absence of thyroid hormone secondary to abnormal thyroid gland developmental or biosynthesis disorders. Cretinism is also known as congenital hypothyroidism.
Pathology: Thyroid dysgenesis is the most common cause.
Presentation: The infants show decreased activity, large anterior fontanelle, poor feeding and weight gain, small stature or poor growth, jaundice, decreased stooling or constipation, hypotonia, and hoarse cry.
Diagnosis: This is made through a blood test by measuring the level of TSH present in the body.
Treatment: Thyroid hormone replacement or levothyroxine.
Prognosis: Prognosis is very poor as the disease must be treated within the first four weeks after birth otherwise the intellectual disability may be permanent.
What is Myxedema?
Myxedema is a dermatologic condition with thick, dry, and waxy skin mainly present due to the accumulation of mucopolysaccharides in the dermis.
Pathology: Mainly caused by excess TSH secretion or hypothyroidism.
Presentation: Pink, yellow and waxy plaques and nodules on the anterolateral aspect of the leg, generalized puffiness, macroglossia, ptosis, periorbital edema, and coarse, sparse hair
Diagnosis: Diagnosis is based on clinical symptoms for instance hoarse voice, dry skin, mental and physical slowness, cold intolerance, and weakness.
Treatment: Thyroid hormone replacement, self-limiting, steroid, and antibiotics.
Prognosis: Prognosis is poor with a mortality rate of up to 50 percent.
What is Thyroiditis?
Thyroiditis is the inflammation of the thyroid gland
Conditions that may be associated with thyroiditis include:
- Hashimoto Thyroiditis
- Subacute Lymphocytic Thyroiditis
- Granulomatous Thyroiditis
What is Hashimoto Thyroiditis?
Hashimoto thyroiditis is an autoimmune disease with goiter, elevated circulating antithyroid peroxidase, and antithyroglobulin antibodies in which the body immune system attacks the thyroid gland. Hashimotos thyroiditis is also known as struma lymphomatosis, lymphocytic thyroiditis.
What is the Pathology of Hashimoto Thyroiditis?
The pathology of hashimoto thyroiditis is:
-Etiology: The cause of hashimoto thyroiditis is heredity, excessive iodine, radiation exposure.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to hashimoto thyroiditis involves the formation of antithyroid antibodies that attack the thyroid tissue, resulting in progressive fibrosis.
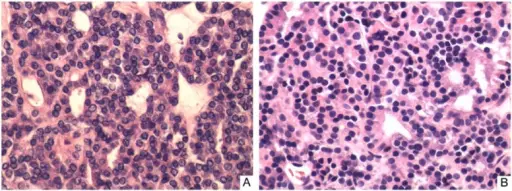
-Histology: The histology associated with hashimoto thyroiditis shows Extensive lymphocytic infiltrate with germinal center formation.
How does Hashimoto Thyroiditis Present?
Patients with Hashimoto thyroiditis are typically middle aged women. The symptoms, features, and clinical findings associated with Hashimoto thyroiditis include voice hoarseness and pressure symptoms in the neck from thyroid enlargement, slowed movement and loss of energy.
How is Hashimoto Thyroiditis Diagnosed?
Hashimoto thyroiditis is diagnosed by detecting elevated levels of antithyroid peroxidase antibodies in the serum.
How is Hashimoto Thyroiditis Treated?
Hashimoto thyroiditis is treated with thyroid hormone replacement such as levothyroxine.
What is the Prognosis of Hashimoto Thyroiditis?
The prognosis of Hashimoto thyroiditis is good with early treatment as it can reverse the symptoms immediately.
What is Subacute Lymphocytic Thyroiditis?
Subacute lymphocytic thyroiditis is the Inflammation of the thyroid gland that includes granulomas.
What is the Pathology of Subacute Lymphocytic Thyroiditis?
The pathology of subacute lymphocytic thyroiditis is:
-Etiology: The cause of subacute lymphocytic thyroiditis is a systemic viral infection
-Genes involved: HLA-B35
-Pathogenesis: The sequence of events that lead to subacute lymphocytic thyroiditis includes the destruction of follicular epithelium and loss of follicular integrity
-Histology: The histology associated with subacute lymphocytic thyroiditis shows neutrophils and destruction of follicles with colloid depletion in early cases and fibrosis in late cases.
How does Subacute Lymphocytic Thyroiditis Present?
Patients with subacute lymphocytic thyroiditis are typically middle aged females. The symptoms, features, and clinical findings associated with subacute lymphocytic thyroiditis include myalgia, fatigue, prostration, high-grade fever, malaise, dysphagia, hoarseness, and pain over the thyroid area.
How is Subacute Lymphocytic Thyroiditis Diagnosed?
Subacute lymphocytic thyroiditis is diagnosed using a radioactive iodine uptake test (RAIU).
How is Subacute Lymphocytic Thyroiditis Treated?
Subacute lymphocytic thyroiditis is treated with aspirin, prednisone, and propranolol.
What is the Prognosis of Subacute Lymphocytic Thyroiditis?
The prognosis of subacute lymphocytic thyroiditis is very good as the symptom reversed in 1-3 months.
What is Granulomatous Thyroiditis?
Granulomatous thyroiditis is Inflammation of the thyroid gland that includes granulomas. Also known as De Quervain thyroiditis. It is the most common cause of a painful thyroid gland.
What is the Pathology of Granulomatous Thyroiditis?
The pathology of granulomatous thyroiditis is:
-Etiology: The cause of granulomatous thyroiditis is a systemic viral infection.
-Genes involved: HLA-B35.
-Pathogenesis: The sequence of events that lead to granulomatous thyroiditis includes the destruction of follicular epithelium and loss of follicular integrity.
-Histology: The histology associated with granulomatous thyroiditis shows neutrophils and destruction of follicles with colloid depletion in early cases and fibrosis in late cases.
How does Granulomatous Thyroiditis Present?
Patients with granulomatous thyroiditis are typically middle aged women. The symptoms, features, and clinical findings associated with subacute lymphocytic thyroiditis include myalgia, fatigue, prostration, high-grade fever, malaise, dysphagia, hoarseness, and pain over the thyroid area.
How is Granulomatous Thyroiditis Diagnosed?
Granulomatous thyroiditis is diagnosed using a radioactive iodine uptake test.
How is Granulomatous Thyroiditis Treated?
Granulomatous thyroiditis is treated with steroids and antibiotics.
What is the Prognosis of Granulomatous Thyroiditis?
The prognosis of granulomatous thyroiditis is very good as the symptom reversed in 1-3 months.
What is Graves Disease?
Graves disease is an autoimmune disease due to autoantibodies to thyroid proteins that cause hyperthyroidism.
What is the Pathology of Graves Disease?
The pathology of Graves disease is:
-Etiology: The cause of Graves disease is a malfunction of the immune system.
Genes involved: None.
-Pathogenesis: The sequence of events that lead to graves’ disease involves the production of IgG autoantibodies directed against the thyrotropin receptor, which is called the thyroid stimulating immunoglobulin.
-Histology: The histology associated with Graves’ disease shows hyperplastic thyroid follicles with papillary infoldings while the nuclei are round.
How does Graves Disease Present?
Patients with graves’ disease typically present in middle age women present at the age range of 35-45. The symptoms, features, and clinical findings associated with graves’ disease include enlarged thyroid, muscle weakness, tremors, sweating, and heat intolerance. Exopthalmos may be present as well, which is a characteristic bulging of the eyes.
How is Graves Disease Diagnosed?
Graves disease is diagnosed clinically by symptoms, presence of laboratory markers of hyperthyroidism, ophthalmopathy, and presence of serum anti thyrotropin antibodies.
How is Graves Disease Treated?
Graves’ disease is treated with Beta-blockers.
What is the Prognosis of Graves Disease?
The prognosis of the disease is fair. The signs and symptoms of Graves ophthalmopathy usually become stable for a year or so and then begin to get better, often on their own
What are Diffuse Goiters?
Diffuse goiters is an autoimmune condition characterized by a diffusely hyperplastic thyroid gland with excessive overproduction of thyroid hormone. A simple nontoxic goiter, which may be diffuse or nodular, is noncancerous hypertrophy of the thyroid without hyperthyroidism, hypothyroidism, or inflammation.
What is a Multinodular Goiter?
A multinodular goiter is a goiter in the thyroid gland with multiple nodules.
What are Thyroid Congenital Nodules?
Thyroid congenital anomalies are those anomalies that have a lump or an enlarged area in the thyroid gland that are present by birth.
Examples of thyroid congenital anomalies include thyroglossal duct cysts.
What is a Thyroglossal Duct Cyst?
A thyroglossal duct cyst is a mass or lump in the front part of the neck that is filled with fluid.
What is the Pathology of Thyroglossal Duct Cyst?
The pathology of thyroglossal duct cyst is:
-Etiology: The cause of thyroglossal duct cyst is the abnormal development of the cells in the thyroid gland between the 4th and 8th week of fetal development.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to thyroglossal duct cyst involves that during embryonic development, the thyroid gland remains connected to the foramen and hyoid bone, the duct gradually disappears by the 10th week of development.
-Histology: The histology associated with thyroglossal duct cyst shows benign cells lining a cystic wall.
How does a Thyroglossal Duct Cyst Present?
Patients with thyroglossal duct cysts typically occur in both males and females. The symptoms, features, and clinical findings associated with thyroglossal duct cyst are a subtle neck swelling without pain.
How is Thyroglossal Duct Cyst Diagnosed?
Thyroglossal duct cyst is diagnosed by physical examination and later referred to imaging.
How is Thyroglossal Duct Cyst Treated?
Thyroglossal duct cyst is treated through surgical removal.
What is the Prognosis of Thyroglossal Duct Cyst?
The prognosis of a thyroglossal duct cyst is good with excision.
What are Neoplasms of the Thyroid?
Neoplasms of the Thyroid are the tumors of the thyroid.
Examples of thyroid adenomas include:
- Follicular adenomas
What is Follicular Adenomas?
Follicular Adenomas are a benign encapsulated tumor of the thyroid gland
What is Thyroid Carcinomas?
Thyroid carcinomas are painless, palpable, solitary thyroid nodules.
Examples of thyroid carcinomas include:
- Anaplastic carcinoma
- Follicular Carcinoma
- Medullary Carcinoma
- Papillary Carcinoma
What is Anaplastic Carcinoma?
Anaplastic carcinoma is the most aggressive malignancy of the thyroid gland.
What is the Pathology of Anaplastic Carcinoma?
The pathology of anaplastic carcinoma is:
-Etiology: The cause of anaplastic carcinoma is unclear but could be associated with iodine deficiency and radiation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to anaplastic carcinoma involves the anaplastic transformation of differentiated thyroid carcinoma
-Histology: The histology associated with anaplastic carcinoma shows widely invasive growth, extensive tumor necrosis, marked nuclear pleomorphism, and high mitotic activity
How does Anaplastic Carcinoma Present?
Patients with anaplastic carcinoma typically occur in females present at the age range of 60 -70 years. The symptoms, features, and clinical findings associated with anaplastic carcinoma include multinodular goiter, rapidly enlarging, painful, firm, ill-defined, lower anterior neck mass, hoarseness, dyspnea, and dysphagia.
How is Anaplastic Carcinoma Diagnosed?
Anaplastic carcinoma is diagnosed using neck imaging studies such as ultrasound, CT scan, or MRI.
How is Anaplastic Carcinoma Treated?
Anaplastic carcinoma is treated radiation therapy or chemotherapy.
What is the Prognosis of Anaplastic Carcinoma?
The prognosis of anaplastic carcinoma is poor as hardly half of the people survive after they are diagnosed with anaplastic carcinoma.
What is Follicular Carcinoma?
Follicular carcinoma is the carcinoma of the thyroid with follicular differentiation but no papillary nuclear features.
What is the Pathology of Follicular Carcinoma?
The pathology of follicular carcinoma is:
-Etiology: The cause of follicular carcinoma is old age, radiation exposure, and iodine deficiency.
-Genes involved: RAS.
-Pathogenesis: The sequence of events that lead to follicular carcinoma involves point mutations that result in dysregulation of the phosphatidylinositol-3 kinase (PI3K)/AKT signaling pathway.
-Histology: The histology associated with follicular carcinoma shows neoplastic follicular cells.
How does Follicular Carcinoma Present?
Patients with follicular carcinoma are typically females. present at the age range of 40-60 years. The symptoms, features, and clinical findings associated with follicular carcinoma include difficulty breathing, hoarseness, difficulty swallowing persistent cough, voice changes, and vocal cord paralysis
How is Follicular Carcinoma Diagnosed?
Follicular carcinoma is diagnosed using blood testing.
How is Follicular Carcinoma Treated?
Follicular carcinoma is treated thyroidectomy or lobectomy.
What is the Prognosis of Follicular Carcinoma?
The prognosis of follicular carcinoma is poor overall however, the prognosis is found to be good in females with a survival of 5 years.
What is Medullary Carcinoma?
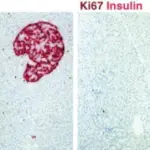
Medullary carcinoma is a neuroendocrine tumor derived from C cells of the ultimobranchial body of the neural crest, which secrete calcitonin.
What is the Pathology of Medullary Carcinoma?
The pathology of medullary carcinoma is:
-Etiology: The cause of medullary carcinoma is unknown. Medullary carcinoma is associated with MEN 2A syndrome.
-Genes involved: RET.
-Pathogenesis: The sequence of events that lead to medullary carcinoma involves the gain of function mutations in the RET proto-oncogene, a 21-exon gene located on chromosome 10q11.
-Histology: The histology associated with medullary carcinoma shows islands of tumor cells having irregular borders, and amyloid.
How does Medullary Carcinoma Present?
Patients with medullary carcinoma typically present in either male or female present at the age range of 35-45. The symptoms, features, and clinical findings associated with medullary carcinoma include hoarseness, dysphagia, respiratory difficulty, lump presence in the neck, and diahorrea.
How is Medullary Carcinoma Diagnosed?
Medullary carcinoma is diagnosed using fine-needle aspiration biopsy.
How is Medullary Carcinoma Treated?
Medullary carcinoma is treated with total thyroidectomy with cervical lymphadenectomy
What is the Prognosis of Medullary Carcinoma?
The prognosis of medullary carcinoma is good with a 5-year survival rate.
What is Papillary Carcinoma?
Papillary carcinoma is the well-differentiated form of thyroid cancer.
What is the Pathology of Papillary Carcinoma?
The pathology of papillary carcinoma is:
-Etiology: The cause of papillary carcinoma is ionizing radiation before the age of 20, or genetic predisposition.
-Genes involved: RET or RAS.
-Pathogenesis: The sequence of events that lead to papillary carcinoma involves somatic rearrangement of RET protooncogene and point mutation in BRAF and RAS genes.
-Histology: The histology associated with papillary carcinoma shows grossly firm mass which is not encapsulated while nuclei are small without nuclear membrane.
How does Papillary Carcinoma Present?
Patients with papillary carcinoma typically occur in females present at the age range of 20-40. The symptoms, features, and clinical findings associated with papillary carcinoma include persistent cough, difficulty breathing, or difficulty swallowing.
How is Papillary Carcinoma Diagnosed?
Papillary carcinoma is diagnosed using preoperative fine-needle aspiration cytology.
How is Papillary Carcinoma Treated?
Papillary carcinoma is treated with total thyroidectomy or postoperative radioactive iodine therapy
What is the Prognosis of Papillary Carcinoma?
The prognosis of papillary carcinoma is good with a ten-year survival rate.