Urinary tract pathology is defined as the pathologies that affect the urinary system.
Urinary tract pathology includes:
Congenital anomalies of the ureters
Inflammation of the ureter
Tumors of the ureter
Obstructions of the ureter
Congenital anomalies of the bladder
Inflammation of the bladder
Metaplastic lesions of the bladder
Neoplasms of the bladder
Inflammation of the urethra
Tumors of the urethra
Ureter pathology
What are Congenital Anomalies of the Ureters?
Congenital anomalies of the ureters are abnormalities that disrupt the development and therefore the structure of ureters.
Examples of congenital anomalies of the ureters include:
Double ureters
Bifid ureters
Ureteropelvic junction obstruction
Diverticula of the ureter
What are Double Ureters?
Double ureters or duplex collecting system is a congenital condition in which the ureteric bud, the embryological origin of the ureter, splits or arises twice.
What is the Pathology of Double ureters?
The pathology of double ureters is:
-Etiology: The cause of double ureters is an incomplete fusion of the upper and lower pole of the kidney which creates two separate drainage systems from the kidney.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to double ureters begins in the human fetus around the 4th week of embryonic development. A ureteric bud division gives rise to two separate parts, each with its renal pelvis and ureter.
-Morphology: The morphology associated with double ureters shows partially duplicated ureters fused into a single ureter proximal to the urinary bladder, which is also known as bifid ureter.
-Histology: The histology associated with double ureters shows characteristics as seen in a normal ureter.
How does Double ureters Present?
Patients with double ureters typically affect females in the neonatal period or early childhood. The symptoms, features, and clinical findings associated with double ureters include palpable abdominal mass in the newborn and may suggest an ectopic ureter or ureterocele. In older children, ureteral duplication may present with urinary tract infection – most commonly due to vesicoureteral reflux.
How is Double Ureters Diagnosed?
Double ureters is diagnosed by hydronephrosis in a postnatal follow-up examination or by the presentation as a urinary tract infection in a neonate.
How is Double Ureters Treated?
Double ureters are treated with ureteroureterostomy
What is the Prognosis of Double Ureters?
The prognosis of double ureters is excellent with appropriate management. Antibiotic suppression is usually warranted in newborns with hydronephrosis or in patients who present with UTI until the diagnosis is made and reflux is ruled out.
What are Bifid Ureters?
Bifid ureters is a congenital renal tract abnormality due to some error or disturbance during development. It is an example of incomplete duplication of the urinary collecting system.
What is the Pathology of Bifid Ureters?
The pathology of bifid ureters is:
-Etiology: The cause of bifid ureters is the development of two ureteric buds.
-Genes involved: ERK/MAPK.
-Pathogenesis: The sequence of events that lead to bifid ureters includes the development when the ureteric bud divides in the lower third of its course. The bifid ureter has resulted from the early division of the metanephric diverticulum; the duplication can be total, double ureter, or partial, bifid ureter.
-Morphology: The morphology associated with bifid ureters shows extrarenal traject of the two ureters which may be near parallel, one beside the other or maybe slightly apart at the top, with the convergent route to their confluence level.
-Histology: The histology associated with bifid ureters shows a thick, fibroelastic, lamina propria lies underneath the epithelium.
How does Bifid Ureters Present?
Patients with bifid ureters typically affect females more than males presenting in early childhood. The symptoms, features, and clinical findings associated with bifid ureters include frequent urinary tract infection, uretero ureteral reflux, ureteric stenosis, urinary lithiasis, and pyelonephritis, non-functioning of kidney units.
How are Bifid Ureters Diagnosed?
Intravenous urography is usually used to diagnose bifid ureters.
How is Bifid Ureters Treated?
The bifid ureter is treated with ureteroureterostomy.
What is the Prognosis of Bifid Ureters?
The prognosis of Bifid ureters is excellent with appropriate management.
What is Ureteropelvic Junction Obstruction?
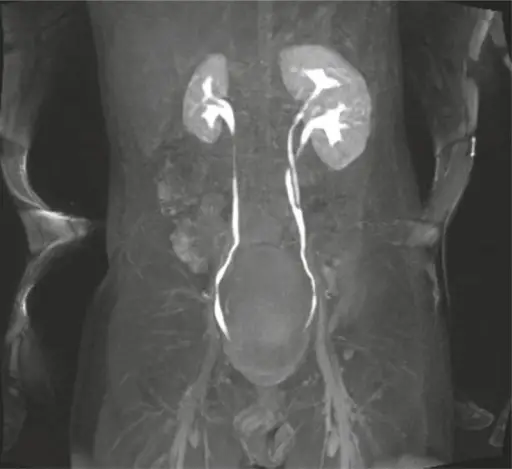
Ureteropelvic junction obstruction is defined as an obstruction of the flow of urine from the renal pelvis to the proximal ureter.
What is the Pathology of Ureteropelvic Junction Obstruction?
The pathology of Ureteropelvic junction obstruction is:
-Etiology: The etiology of ureteropelvic junction obstruction includes stenosis due to scarring of ureteral valves.
-Genes involved: AGTR2, BMP4, Id2.
-Pathogenesis: The sequence of events that lead to ureteropelvic junction obstruction includes partial or intermittent blockage of the flow of urine that occurs where the ureter enters the kidney.
-Morphology: The morphology associated with ureteropelvic junction obstruction shows marked dilatation of the renal calyces and pelvis, funneling down to a narrow beak end, with non visualization of the ipsilateral ureter.
-Histology: The histology associated with ureteropelvic junction obstruction shows parenchymal damage.
How does Ureteropelvic Junction Obstruction Present?
Patients with ureteropelvic junction obstruction typically affect males twice more than females usually presenting in the pediatric age group. The symptoms, features, and clinical findings associated with ureteropelvic junction obstruction include hydronephrosis. Older children may present with urinary tract infection (UTI), hematuria, a flank mass, or intermittent flank pain secondary to a primary UPJ obstruction. Adults with UPJ obstruction can present with various symptoms, including back and flank pain, UTI, and/or pyelonephritis.
How is Ureteropelvic Junction Obstruction Diagnosed?
Ureteropelvic junction obstruction is diagnosed using complete blood count, kidney function tests, including creatinine, GFR, and BUN.
How is Ureteropelvic Junction Obstruction Treated?
Ureteropelvic junction obstruction is treated by surgical intervention.
What is the Prognosis of Ureteropelvic Junction Obstruction?
The prognosis for ureteropelvic junction obstruction is good as it resolves gradually.
What are Diverticula of the Ureter?
Diverticula of the ureter are acquired from false diverticula resulting from herniation of epithelium through the muscular layer of the ureter and characterized by the presence of multiple outpouchings smaller than 5 mm. It is sometimes bilateral and is often located in the upper two-thirds of the ureter.
What is the Pathology of Diverticula of the Ureter?
The pathology of Diverticula of the ureter is:
-Etiology: The cause of diverticula of the ureter is not clear, but chronic inflammation and/or obstruction are likely causes.
-Genes involved: Gene involvement is not clear.
-Pathogenesis: The sequence of events that lead to diverticula of the ureter includes urothelial hyperplasia caused by chronic inflammation and the consequent impaction of the hyperplastic urothelium into the subepithelial connective tissue.
-Morphology: The morphology associated with diverticula of the ureter shows multiple bilateral small outpouchings of the ureter involving the proximal two-thirds of the ureter
-Histology: The histology associated with diverticula of the ureter shows focal hyperplasia of the urothelium protruding into the muscule.
How does Diverticula of the Ureter Present?
Patients with diverticula of the ureter typically affect men 60-70 years of age, but it is a very uncommon occurrence. Most patients are asymptomatic, but it may be seen in patients with a history of chronic urinary tract infection or haematuria.
How is Diverticula of the Ureter Diagnosed?
Diverticula of the ureter are diagnosed by intravenous urography, antegrade urography, or retrograde pyelography.
How is Diverticula of the Ureter Treated?
There is no specific treatment indicated in asymptomatic patients.
What is the Prognosis of Diverticula of the Ureter?
The prognosis of diverticula of the ureter is generally good but can worsen in association with urothelial carcinoma.
What is Inflammation of the Ureter?
Inflammation of the ureter is Ureteritis.
Ureteritis is Proliferative or reactive changes occurring in von Brunn nests which acquire luminal spaces, become cystically dilated (cystitis cystica), undergo glandular metaplasia (cystitis glandularis), or intestinal-type metaplasia.
What is the Pathology of Ureteritis?
The pathology of Ureteritis is:
-Etiology: The cause of ureteritis is chronic irritation / local inflammatory insult.
-Genes involved: No genetic association.
-Pathogenesis: The sequence of events that lead to ureteritis involves the reactive process in response to chronic irritation, infection, calculi, outlet obstruction, catheterization. Urothelium proliferates and invaginates into underlying lamina propria.
-Morphology: The morphology associated with ureteritis shows multiple small submucosal cysts.
-Histology: The histology associated with ureteritis shows abundant urothelial von Brunn nests.
How does Ureteritis Present?
Patients with ureteritis typically affect males more than females and it can occur at any age. The symptoms, features, and clinical findings associated with ureteritis include the following. The majority are asymptomatic incidental findings. May infrequently cause recurrent urinary tract infections. Occasionally appears as a polypoid or papillary mass on cystoscopy. Cystitis glandularis can be associated with pelvic lipomatosis and bladder exstrophy.
How is Ureteritis Diagnosed?
Ureteritis is diagnosed by microscopic examination of resected tissue.
How is Ureteritis Treated?
Ureteritis is treated by the elimination of underlying sources of irritation. Antibiotic therapy is associated with chronic urinary tract infections. Occasionally surgical resection (transurethral) may be necessary.
What is the Prognosis of Ureteritis?
The prognosis of ureteritis is good. Reactive process without malignant potential. May regress if the cause of irritation is removed.
What are Tumors of the Ureter?
Tumors of the ureter are an abnormal growth of cells on the inside lining of the tubes (ureters) that connect your kidneys to your bladder.
Examples of Tumors of the Ureter include:
Fibroepithelial Polyp of the Ureter
Urothelial Carcinomas
What is Fibroepithelial Polyp of the Ureter?
Fibroepithelial Polyp of the Ureter is a rare benign tumor. They are an exophytic intraluminal mass of vascular connective tissue and variable inflammatory cells covered by normal urothelium.
What is the Pathology of Fibroepithelial Polyp of the Ureter?
The pathology of Fibroepithelial Polyp of the Ureter is:
-Etiology: The cause of fibroepithelial polyps is unclear, they are thought to be either congenital slow-growing lesions or lesions that develop as a result of chronic urothelial irritants, such as infection, inflammation, calculi, or obstruction.
-Genes involved: Gene involvement is not clear.
-Pathogenesis: The sequence of events that lead to fibroepithelial polyp remains uncertain.
-Morphology: The morphology associated with fibroepithelial polyp of the ureter shows long, smooth ureteral filling defects; their position may change between images, and they are associated with varying degrees of hydronephrosis.
-Histology: The histology associated with fibroepithelial polyp of the ureter shows loose vascular fibrous stroma with overlying benign transitional epithelium.
How does Fibroepithelial Polyp of the Ureter Present?
Patients with fibroepithelial polyp of the ureter typically affect males three times more than females in their 3rd to 4th decade of life. The symptoms, features, and clinical findings associated with the fibroepithelial polyp of the ureter include hematuria and flank pain. The pain is characteristically intermittent and colicky due to partial obstruction. Urinary frequency, dysuria, and pyuria are other less common findings. The flank pain may be attributable to either torsion or intussusception of the polyp or intermittent obstruction.
How is Fibroepithelial Polyp of the Ureter Diagnosed?
Fibroepithelial Polyp of the Ureter is diagnosed by intraoperative retrograde pyelogram. If a filling defect is encountered, ureteroscopy is indicated for polyp mapping.
How is Fibroepithelial Polyp of the Ureter Treated?
Fibroepithelial Polyp of the Ureter is treated by ureteroscopic resection.
What is the Prognosis of Fibroepithelial Polyp of the Ureter?
The prognosis of the fibroepithelial polyp of the ureter is excellent.
What are Urothelial Carcinomas?
Urothelial Carcinomas are cancers that begin in cells called urothelial cells that line the urethra, bladder, ureters, renal pelvis, and some other organs. Urothelial cells are also called transitional cells. These cells can change shape and stretch without breaking apart. Also called transitional cell cancer.
What is the Pathology of Urothelial Carcinomas?
The pathology of Urothelial Carcinomas is:
-Etiology: The cause of urothelial carcinomas is smoking, schistosomiasis infection, and occupational exposure to certain chemicals.
-Genes involved: FGFR3, TP53, PIK3CA, KDM6A, ARID1A, KMT2D, HRAS, TERT, KRAS, CREBBP, RB1 and TSC1.
-Pathogenesis: The sequence of events that lead to urothelial carcinomas develops via two distinct pathways, the first relates to papillary lesions, and the second relates to flat lesions.
-Morphology: The morphology associated with urothelial carcinomas shows a polypoid, sessile, fungating ulcerated and/or infiltrative lesion.
-Histology: The histology associated with urothelial carcinomas shows neoplastic cells invade the bladder wall as nests, cords, trabeculae, small clusters, or single cells that are usually separated by desmoplastic stroma.
How does Urothelial Carcinomas Present?
Patients with urothelial carcinomas typically affect males four times more than females in their adulthood. The symptoms, features, and clinical findings associated with urothelial carcinomas include bladder cancer characteristically causing blood in the urine. Blood in the urine is the most common symptom of bladder cancer and is painless. Other possible symptoms include pain during urination, frequent urination, or feeling the need to urinate without being able to do so. People with advanced disease may have pelvic or bony pain, lower-extremity swelling, or flank pain. Rarely, a palpable mass can be detected on physical examination.
How is Urothelial Carcinomas Diagnosed?
Diagnostic modalities used in diagnosing BC include Imaging (ultrasound, intravenous urography (IVU), computed tomography (CT), magnetic resonance imaging (MRI)), cystoscopy, and biopsy.
How is Urothelial Carcinomas Treated?
The treatment of bladder cancer is typically surgery.
What is the Prognosis of Urothelial Carcinomas?
The prognosis of urothelial carcinomas is good. The 5-year overall survival (OS) for pT1 is 75%, for pT2 is 50%, and for pT3 is 20%.
What are Obstructions of the Ureter?
Obstruction of the ureter is a blockage in one or both of the tubes (ureters) that carry urine from your kidneys to your bladder.
Examples of Obstructions of the Ureter include:
Sclerosing Retroperitoneal Fibrosis
What is Sclerosing Retroperitoneal Fibrosis?
Sclerosing Retroperitoneal Fibrosis is a relatively rare condition that is characterized by chronic inflammatory and fibrotic process in the retroperitoneum that can lead to compression of structures within the retroperitoneum.
What is the Pathology of Sclerosing Retroperitoneal Fibrosis?
The pathology of sclerosing retroperitoneal fibrosis is:
-Etiology: The cause of sclerosing retroperitoneal fibrosis is idiopathic in 70% of the cases.
-Genes involved: No genes associated.
-Pathogenesis: The sequence of events that lead to sclerosing retroperitoneal fibrosis is due to the manifestation of a systemic autoimmune disease, which may arise as a primary aortitis that elicits a periaortic fibro-inflammatory response.
-Morphology: The morphology associated with sclerosing retroperitoneal fibrosis shows poorly circumscribed fibrotic mass.
-Histology: The histology associated with sclerosing retroperitoneal fibrosis shows the appearance of RPF of a nonspecific inflammatory process.
How does Sclerosing Retroperitoneal Fibrosis Present?
Patients with sclerosing retroperitoneal fibrosis typically affect males 2 times more than females in 40 to 60 years of age. The symptoms, features, and clinical findings associated with sclerosing retroperitoneal fibrosis include lower back and/or flank pain. This pain is often described as dull, non-colicky, unchanged with position, and with radiation into the groin or lower abdomen. Other possible associated symptoms include nausea, generalized malaise, anorexia, weight loss, oliguria, anuria. Patient’s may also describe upper-leg claudication related to arterial compromise of the lower extremities, or symptoms of mesenteric ischemia due to compression of mesenteric arteries.
How is Sclerosing Retroperitoneal Fibrosis Diagnosed?
The diagnosis of retroperitoneal fibrosis cannot be made based on the results of laboratory studies. CT is the best diagnostic modality.
How is Sclerosing Retroperitoneal Fibrosis Treated?
Patients with signs of ureteral compression with hydronephrosis and uremia require emergent decompression by either percutaneous nephrostomy tube or indwelling ureteral stents.
What is the Prognosis of Sclerosing Retroperitoneal Fibrosis?
The prognosis of Sclerosing Retroperitoneal Fibrosis is good. Often within a few days of initiating treatment the patient’s symptoms begin to improve.
What are Congenital Anomalies of the Bladder?
Congenital Anomalies of the Bladder are a group of congenital abnormalities affecting the bladder.
Examples of Congenital Anomalies of the Bladder include:
Diverticula of the Bladder
Urachal anomalies of the bladder
Vesicoureteral reflux
Exstrophy of the Bladder
What is Diverticula of the Bladder?
Diverticula of the Bladder are balloon-like growths on the bladder commonly associated with chronic outflow obstruction, such as benign prostatic hyperplasia in older males. Usually found in pairs on opposite sides of the bladder.
What is the Pathology of Diverticula of the Bladder?
The pathology of Diverticula of the Bladder is:
-Etiology: The cause of Diverticula of the Bladder is Congenital cases are due to bladder outlet obstruction or failure of muscle development.
-Genes involved: EFEMP1.
-Pathogenesis: The sequence of events that lead to Diverticula of the Bladder is the raised intracystic pressure by the arrangement of the three interlacing muscle layers.
-Morphology: The morphology associated with Diverticula of the Bladder shows narrow necks, round / ovoid pouch from 1 – 18 cm (average 5.0 cm).
-Histology: The histology associated with Diverticula of the Bladder shows wall consists of fibrous tissue with no / scant muscularis propria.
How does Diverticula of the Bladder Present?
Patients with Diverticula of the Bladder typically affect males 1-80 years of age. The symptoms, features, and clinical findings associated with Diverticula of the Bladder include the following. Most bladder diverticula are small and asymptomatic. When symptomatic, usually associated with infections and stones (due to urine stasis), urinary retention, or perforation.
How is Diverticula of the Bladder Diagnosed?
Diverticula of the Bladder is diagnosed by an x-ray test of the bladder.
How is Diverticula of the Bladder Treated?
Diverticula of the Bladder is treated by nonoperative treatment, surgical bladder outlet reduction, or removal of the diverticulum.
What is the Prognosis of Diverticula of the Bladder?
The prognosis of Diverticula of the Bladder is poor in the case of tumor development.
What are Urachal Anomalies of the Bladder?
Urachal anomalies of the bladder are abnormalities that result from incomplete involution of this embryonic structure, leading to various pathologies. Congenital UA can be divided into five groups: patent urachus, umbilical-urachal sinus, vesicoureteral diverticulum, urachal cyst, and alternating sinus. Typically, a patent urachus is detected around birth, while the other congenital UA tends to be asymptomatic.
What is the Pathology of Urachal Anomalies?
The pathology of Urachal anomalies is:
-Etiology: The cause of Urachal anomalies is an incomplete involution of the urachus.
-Genes involved: Not clear.
-Pathogenesis: The sequence of events that lead to urachal anomalies is due to abnormal sealing during embryogenesis. This may give rise to urachal cysts, patent urachus, urachal sinus, and urachal diverticulum.
-Morphology: The morphology associated with urachal anomalies shows different patterns.
-Histology: The histology associated with Urachal anomalies shows fragmented tubules separated by fibrous cords, but without a desmoplastic tissue response. No goblet cells, no atypia in the epithelium
How do Urachal Anomalies Present?
Patients with Urachal anomalies typically affect males more than females in their adulthood. The symptoms, features, and clinical findings associated with Urachal anomalies include the following in each abnormality, but are typically asymptomatic.
How are Urachal Anomalies Diagnosed?
Urachal disorders are usually diagnosed using ultrasound, sinogram, and VCUG.
How is Urachal Anomalies Treated?
Urachal anomalies are treated with surgical excision and antibiotics.
What is the Prognosis of Urachal Anomalies?
The prognosis of Urachal anomalies is usually good with proper treatment.
What is Vesicoureteral Reflux?
Vesicoureteral reflux, also known as vesicoureteric reflux, is a condition in which flows retrograde, or backward, from the bladder into one or both ureters and then to the renal calyx or kidneys.
What is the Pathology of Vesicoureteral Reflux?
The pathology of Vesicoureteral reflux is:
-Etiology: The etiology of vesicoureteral reflux is the failure of the bladder to empty properly.
-Genes involved: PAX2 (10q24. 31).
-Pathogenesis: The sequence of events that lead to Vesicoureteral reflux includes the congenital anomalous development of the ureterovesical junction. Reflux of urine from the bladder into the ureter may cause bacterial infection of the upper urinary tract; about 30 to 40% of infants and toddlers with urinary tract infections have VUR.
-Morphology: The morphology associated with vesicoureteral reflux shows congenital pouches, openings, or abnormal connections.
-Histology: The histology associated with Vesicoureteral reflux shows the smooth muscle.
How does Vesicoureteral Reflux Present?
Patients with Vesicoureteral reflux typically affect males more than females at birth after one year of age, females have five to six times more prevalence of VUR as compared to males. Most children with vesicoureteral reflux are asymptomatic.
How is Vesicoureteral Reflux Diagnosed?
Vesicoureteral reflux is diagnosed by cystography, fluoroscopic voiding cystourethrogram (VCUG), ultrasound, and technetium-99m dimercaptosuccinic acid (DMSA) scintigraphy.
How is Vesicoureteral Reflux Treated?
Vesicoureteral reflux is treated with antibiotics, bowel and bladder management.
What is the Prognosis of Vesicoureteral Reflux?
The prognosis of vesicoureteral reflux is good with a 95% success rate.
What is Exstrophy of the Bladder?
Exstrophy of the Bladder is a congenital anomaly that exists along the spectrum of the exstrophy-epispadias complex, and most notably involves protrusion of the urinary bladder through a defect in the abdominal wall.
What is the Pathology of Exstrophy of the Bladder?
The pathology of Exstrophy of the Bladder is:
-Etiology: The cause is not yet clinically established but is thought to be in part due to failed reinforcement of the cloacal membrane by underlying mesoderm.
-Genes involved: ISL1.
-Pathogenesis: The sequence of events that lead to Exstrophy of the Bladder is a developmental abnormality that occurs 4-5 weeks after conception in which the cloacal membrane is not replaced by tissue that will form the abdominal muscles.
-Histology: The histology associated with Exstrophy of the Bladder shows acute and chronic inflammation; lamina propria fibrosis.
How does Exstrophy of the Bladder Present?
Patients with Exstrophy of the Bladder typically affect males two or six times more than females presenting at birth. The symptoms, features, and clinical findings associated with Exstrophy of the Bladder include a flattened puborectal sling, separation of the pubic symphysis. shortening of a pubic ramus, external rotation of the pelvis.
How is Exstrophy of the Bladder Diagnosed?
The diagnosis of exstrophy bladder is clinical and does not require any other additional investigations. Routine hemogram and blood chemistry are performed as a part of the preoperative work-up.
How is Exstrophy of the Bladder Treated?
Exstrophy of the Bladder is treated by surgical excision.
What is the Prognosis of Exstrophy of the Bladder?
The Prognosis of Exstrophy of the Bladder is good with the most important criterion for improving long-term prognosis being the success of the initial closure.
What is Inflammation of the Bladder?
Inflammation of the Bladder is the Inflammation of the urinary bladder, allso called cystitis.
Examples of Inflammation of the bladder includes:
Acute cystitis
Chronic cystitis
Interstitial cystitis
Polypoid cystitis
Malakoplakia
What is Acute Cystitis?
Acute cystitis is an infection of the bladder or lower urinary tract.
What is the Pathology of Acute Cystitis?
The pathology of acute cystitis is:
-Etiology: The cause of acute cystitis is typically caused by Escherichia coli, Staphylococcus saprophyticus, and Klebsiella species.
-Genes involved: IL-1β
-Pathogenesis: The sequence of events that lead to acute cystitis in women begins with the colonization of the vaginal introitus by uropathogens from the fecal flora, followed by ascension via the urethra into the bladder and, in the case of pyelonephritis, to the kidneys via the ureters.
-Morphology: The morphology associated with acute cystitis is not clear.
-Histology: The histology associated with acute cystitis usually shows neutrophils.
How does Acute Cystitis Present?
Patients with acute cystitis typically affect females 16-35 years of age. The symptoms, features, and clinical findings associated with acute cystitis include burning with urination, and frequent urination.
How is Acute Cystitis Diagnosed?
Acute cystitis is diagnosed with a urine dipstick test.
How is Acute Cystitis Treated?
Acute cystitis is treated empirically with antibiotics.
What is the Prognosis of Acute Cystitis?
The prognosis of acute cystitis is excellent with proper treatment.
What is Chronic Cystitis?
Chronic cystitis is a chronic inflammatory condition of the bladder that is refractory to treatment or surgical correction.
What is the Pathology of Chronic Cystitis?
The pathology of chronic cystitis is:
-Etiology: The cause of chronic cystitis is bacterial pathogens.
-Genes involved: HSPA1B, CXCR1 & 2, TLR2, TLR4, TGF-β1 genes.
-Pathogenesis: The sequence of events that lead to chronic cystitis is obstruction and stasis of urine flow.
-Morphology: The morphology associated with chronic cystitis shows red, friable, heaped and ulcerated mucosa on cystoscopy.
-Histology: The histology associated with chronic cystitis shows small vessels radiating towards a central scar.
How does Chronic Cystitis Present?
Patients with chronic cystitis typically affect women more commonly than males in 30 to 50 years of age. The symptoms, features, and clinical findings associated with chronic cystitis include variable symptoms, including discomfort with bladder filling and relief with voiding.
How is Chronic Cystitis Diagnosed?
The diagnosis of chronic cystitis is usually made clinically, with urine culture, and urinalysis.
How is Chronic Cystitis Treated?
Chronic cystitis is treated with corrective surgical treatment of anatomic pathology, immunomodulatory therapy, and antibiotics.
What is the Prognosis of Chronic Cystitis?
The prognosis of chronic cystitis is good with appropriate treatment.
What is Interstitial Cystitis?
Interstitial cystitis is a condition that affects the urinary bladder, characterized by chronic inflammation. It is not secondary to an infection. It is a rare idiopathic condition of the edematous and possibly ulcerated bladder mucosa and a diagnosis of exclusion.
What is the Pathology of Interstitial Cystitis?
The pathology of interstitial cystitis is:
-Etiology: The etiology of interstitial cystitis is not well understood, and the current thoughts around its pathogenesis remain multifactorial.
-Genes involved: T13q22–q32.
-Morphology: The morphology associated with interstitial cystitis shows classic inflammatory type lesions: reddened mucosal areas with small vessels radiating towards a central scar, fibrin deposit or coagulum; site may rupture with oozing of blood and can have bullous edema.
Nonulcer type: normal-appearing urothelium or can have multiple glomerulations.
-Histology: The histology associated with interstitial cystitis shows mucosal ulceration with overlying fibrinous exudates and necrotic debris.
How does Interstitial Cystitis Present?
Patients with interstitial cystitis typically affect females between 50-60 years of age. The symptoms, features, and clinical findings associated with interstitial cystitis include suprapubic pain, urinary frequency, painful sexual intercourse, and waking up from sleep to urinate.
How is Interstitial Cystitis Diagnosed?
The diagnosis of interstitial cystitis is usually made through potassium sensitivity tests and cystoscopy.
How is Interstitial Cystitis Treated?
Interstitial cystitis is treated with antibiotics and surgical intervention.
What is the Prognosis of Interstitial Cystitis?
The prognosis of interstitial cystitis is good with appropriate treatment.
What is Polypoid Cystitis?
Polypoid pystitis is a reversible inflammatory exophytic lesion of the bladder mucosa
What is the Pathology of Polypoid Cystitis?
The pathology of polypoid cystitis is:
-Etiology: The cause of polypoid cystitis is an injury to the bladder mucosa.
-Genes involved: TP53.
-Pathogenesis: The sequence of events that lead to polypoid cystitis is from injury caused by urinary catheters. Polypoid cystitis can also be caused by other conditions that injure or irritate the inner lining of the bladder such as kidney stones, and radiation therapy.
-Morphology: The morphology associated with polypoid cystitis shows friable, broad-based, often edematous bullous, polypoid or papillary lesions.
-Histology: The histology associated with polypoid cystitis shows thin, finger-like papillae or broad-based polypoid lesions with congestion and edema of lamina propria.
How does Polypoid Cystitis Present?
Patients with polypoid cystitis typically affect males 49 years of age. The symptoms, features, and clinical findings associated with polypoid cystitis include painful urination and hematuria, pain with burning urination, and pressure in the bladder along with urinary incontinence.
How is Polypoid Cystitis Diagnosed?
Polypoid cystitis is diagnosed by ultrasound or CT scan to better visualize the bladder.
How is Polypoid Cystitis Treated?
Polypoid cystitis is treated by a combination of endoscopic resection, ureteral stenting, and in resistant cases oral steroids which can be considered to aid the resolution of inflammation in the absence of infection.
What is the Prognosis of Polypoid Cystitis?
The prognosis of polypoid cystitis is generally good with appropriate treatment.
What is Malakoplakia?
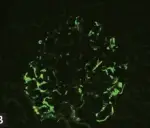
Malakoplakia is a rare inflammatory condition that typically occurs in immunocompromised individuals and is thought to be secondary to a bactericidal defect in macrophages. Malakoplakia typically affects the urinary tract, but the involvement of nearly every organ system has been reported.
What is the Pathology of Malakoplakia?
The pathology of Malakoplakia is:
-Etiology: The cause of malakoplakia is the insufficient killing of bacteria by macrophages.
-Genes involved: BTK.
-Pathogenesis: The sequence of events that lead to malakoplakia is deficiencies in beta-glucuronidase and intracellular cGMP resulting in inadequate microtubular function and phagolysosomal activity, leading to the accumulation of partially digested bacteria in macrophages.
-Morphology: The morphology associated with malakoplakia shows single or multiple white-yellow soft raised plaques on the mucosal surface
-Histology: The histology associated with malakoplakia shows dermal sheets of von Hansemann cells and a variable mixed inflammatory infiltrate consisting of neutrophils, lymphocytes, and plasma cells.
How does Malakoplakia Present?
Patients with malakoplakia are typically affected immunocompromised women at 50 years of age. The symptoms, features, and clinical findings associated with Malakoplakia include urinary symptoms and urinary tract infection.
How is Malakoplakia Diagnosed?
Malakoplakia is diagnosed by urinalysis.
How is Malakoplakia Treated?
Malakoplakia is treated by catheterizing the affected person with full aseptic precautions. Additionally, irrigating the bladder with distilled water three times daily with a 3-way Foley catheter and urinary antiseptics like pyridium may be used to help relieve urinary symptoms. Antibiotics such as trimethoprim-sulfamethoxazole or ciprofloxacin may be used.
What is the Prognosis of Malakoplakia?
The prognosis of malakoplakia is excellent with appropriate treatment.
What are Metaplastic Lesions of the Bladder?
Metaplastic lesions of the bladder are tumors of the bladder that are metaplastic.
Metaplastic lesions of the bladder include:
Cystitis cystica
Cystitis glandularis
Squamous metaplasia of the bladder
Nephrogenic adenoma of the bladder
What is Cystitis Cystica?
Cystitis cystica is a rare chronic reactive inflammatory disorder thought to be caused by chronic irritation of the urothelium because of infection, calculi, outlet obstruction, or tumor resulting in multiple small filling defects in the bladder wall.
What is the Pathology of Cystitis Cystica?
The pathology of cystitis cystica is:
-Etiology: The cause of cystitis cystica is chronic irritation and local inflammatory insult.
-Genes involved: No associated genes.
-Pathogenesis: The sequence of events that lead to cystitis cystica is a reactive process in response to chronic irritation, infection, calculi, outlet obstruction, catheterization. Urothelium proliferates and invaginates into underlying lamina propria.
-Morphology: The morphology associated with cystitis cystica shows translucent submucosal cysts, mostly < 5 mm diameter.
-Histology: The histology associated with cystitis cystica shows abundant urothelial von Brunn nests. Often exhibit a vaguely lobular distribution of invaginations.
How does Cystitis Cystica Present?
Patients with cystitis cystica typically affect both males and females at any age. The symptoms, features, and clinical findings associated with cystitis cystica include the following. The majority are asymptomatic incidental findings.
How is Cystitis Cystica Diagnosed?
Cystitis cystica is diagnosed by microscopic examination of resected tissue.
How is Cystitis Cystica Treated?
Cystitis cystica is treated by the elimination of underlying sources of irritation. Antibiotic therapy is associated with chronic urinary tract infections. Occasionally surgical resection (transurethral) may be necessary
What is the Prognosis of Cystitis Cystica?
The prognosis of cystitis cystica is variable. It is a reactive process without malignant potential. May regress if the cause of irritation is removed.
What is Cystitis Glandularis?
Cystitis glandularis is a proliferative disorder of the urinary bladder in which there is glandular metaplasia of the transitional cells lining the urinary bladder.
What is the Pathology of Cystitis Glandularis?
The pathology of cystitis glandularis is:
-Etiology: The cause of cystitis glandularis is chronic bladder outlet obstruction, pelvic lipomatosis, benign prostatic hypertrophy, bladder transitional/urothelial cell carcinoma.
-Genes involved: CCND1, CCNA1, EGFR, AR, CX3CL1, CXCL6, and CXCL1.
-Pathogenesis: The sequence of events that lead to Cystitis glandularis result in metaplasia of the urothelium, which proliferates into buds, which grow down into the connective tissue beneath the epithelium in the lamina propria.
-Morphology: The morphology associated with cystitis glandularis shows lobulated outline of the urinary bladder with a nodular filling defect within.
-Histology: The histology associated with cystitis glandularis shows abundant urothelial von Brunn nests.
How does Cystitis Glandularis Present?
Patients with cystitis glandularis typically affect both males and females at all years of age. The symptoms, features, and clinical findings associated with cystitis glandularis include renal colic and abdominal pain; a few patients with a shorter course of the disease also had nausea, vomiting, frequency, urgency, dysuria, hematuria, and fever.
How is Cystitis Glandularis Diagnosed?
Cystitis glandularis is diagnosed by cystoscopy in ureteroscopic surgery.
How is Cystitis Glandularis Treated?
Cystitis glandularis is treated by removing the source of irritation and surgical excision of the area of inflammation or cystectomy in rare severe cases.
What is the Prognosis of Cystitis Glandularis?
The prognosis of cystitis glandularis is variable.
What is Squamous Metaplasia of the Bladder?
Squamous metaplasia of the bladder is a benign non-cancerous change (metaplasia) of surfacing lining cells (epithelium) to a squamous morphology.
What is the Pathology of Squamous Metaplasia of the Bladder?
The pathology of squamous metaplasia of the bladder is:
-Etiology: The cause of squamous metaplasia of the bladder is urinary tract infections.
-Genes involved: UP genes.
-Pathogenesis: The sequence of events that lead to squamous metaplasia of the bladder is the excessive formation of squamous epithelium with desquamation and piling of the epithelium, identifying this lesion as a ‘cholesteatoma’. The urothelium is replaced by stratified squamous epithelium which can be classified into keratinizing and nonkeratinizing subtypes.
-Morphology: The morphology associated with squamous metaplasia of the bladder shows solitary and large at the time of detection, with muscular wall invasion reported in a high proportion of patients.
-Histology: The histology associated with squamous metaplasia of the bladder shows that the epithelium has abundant intracytoplasmic glycogen, similar to vaginal or cervical squamous epithelium.
How does Squamous Metaplasia of the Bladder Present?
Patients with squamous metaplasia of the bladder typically affect women. The symptoms, features, and clinical findings associated with squamous metaplasia of the bladder include non-specific irritative urinary symptoms including haematuria, dysuria, urgency, and frequency.
How is Squamous Metaplasia of the Bladder Diagnosed?
Squamous metaplasia of the bladder is diagnosed on morphology.
How is Squamous Metaplasia of the Bladder Treated?
Squamous metaplasia of the bladder is treated by transurethral resection, cystectomy, and fulguration.
What is Nephrogenic Adenoma of the Bladder?
Nephrogenic adenoma of the bladder is a benign polypoid, papillary, fungating, or velvety lesion found in the bladder or prostatic urethra after urothelial injury which has multiple histologic patterns.
What is the Pathology of Nephrogenic Adenoma of the Bladder?
The pathology of Nephrogenic adenoma of the bladder is:
-Etiology: The cause of nephrogenic adenoma of the bladder is urinary tract infections.
-Genes involved: PAX2, PAX8, AMACR, CD10, CK7, GATA3, CK903.
-Pathogenesis: The sequence of events that lead to a nephrogenic adenoma is the metaplastic lesion.
-Morphology: The morphology associated with nephrogenic adenoma of the bladder shows friable soft tissue fragments.
-Histology: The histology associated with nephrogenic adenoma of the bladder shows tubules lined by cuboidal or hobnail cells.
How is Nephrogenic Adenoma of the Bladder Diagnosed?
Nephrogenic adenoma of the bladder is diagnosed by biopsy.
How is Nephrogenic Adenoma of the Bladder Treated?
Nephrogenic adenoma of the bladder is treated with urinary bladder is resection and antibiotics.
What is the Prognosis of Nephrogenic Adenoma of the Bladder?
The prognosis of nephrogenic adenoma of the bladder is variable.
What are Neoplasms of the Bladder?
Neoplasms of the bladder are tumors that arise from the bladder layers.
Examples of neoplasms of the bladder include:
Transitional tumors of the bladder
Exophytic papillomas of the bladder
Inverted papilloma of the bladder
Papillary urothelial neoplasm of low malignant potential
Low grade papillary urothelial carcinoma
High grade papillary urothelial carcinoma
Carcinoma in situ of the bladder
Adenocarcinoma of the bladder
Mixed carcinoma of the bladder
Sarcoma of the bladder
Small cell carcinoma of the bladder
What are Transitional Tumors of the Bladder?
Transitional tumors of the bladder, also called urothelial carcinoma, are a type of cancer that typically occurs in the urinary system. Transitional cell carcinomas arise from the transitional epithelium, a tissue lining the inner surface of these hollow organs. When the term “urothelial” is used, it specifically refers to carcinoma of the urothelium, meaning a transitional cell carcinoma of the urinary system.
What is the Pathology of Transitional Tumors of the Bladder?
The pathology of transitional tumors of the bladder is:
-Etiology: The cause of transitional tumors is the environmental carcinogenic influences.
-Genes involved: RAS.
-Pathogenesis: The sequence of events that lead to transitional tumors of the bladder is a polyclonal field change defect with frequent recurrences due to a heightened potential for malignant transformation.
-Morphology: The morphology associated with transitional tumors of the bladder shows subtle bladder wall thickening.
-Histology: The histology associated with transitional tumors of the bladder shows a nested pattern of invasion.
How do Transitional Tumors of the Bladder Present?
Patients with transitional tumors of the bladder typically affect older males. The symptoms, features, and clinical findings associated with transitional tumors of the bladder include painless gross hematuria. Patients with advanced disease can present with pelvic or bony pain, lower-extremity edema from iliac vessel compression, or flank pain from ureteral obstruction.
How are Transitional Tumors of the Bladder Diagnosed?
Transitional tumors of the bladder are diagnosed by CT, conventional urography, and MRI.
How are Transitional Tumors of the Bladder Treated?
Transitional tumors are treated with transurethral resection with or without intravesical therapy.
What is the Prognosis of Transitional Tumors of the Bladder?
The prognosis of transitional tumors is excelled in the case of superficial tumors.
What are Exophytic Papillomas of the Bladder?
Exophytic papillomas of the bladder are an uncommon benign exophytic neoplasm composed of a delicate fibrovascular core covered by normal-appearing urothelium.
What is the Pathology of Exophytic Papillomas of the Bladder?
The pathology of exophytic papillomas of the bladder is:
-Etiology: The cause of exophytic papillomas of the bladder is unknown.
-Genes involved: KRAS / HRAS.
-Pathogenesis: The sequence of events that lead to exophytic papillomas of the bladder is encountered as a de novo lesion (without prior urothelial neoplasm).
-Morphology: The morphology associated with exophytic papillomas of the bladder shows soft, pink, small isolated growth with delicate papillary structures, usually pedunculated.
-Histology: The histology associated with exophytic papillomas of the bladder shows discrete papillary structures with central fibrovascular cores with hierarchical branching patterns but without fusion.
How does Exophytic Papillomas of the Bladder Present?
Patients with exophytic papillomas of the bladder typically affect males at less than 50 years of age. The symptoms, features, and clinical findings associated with exophytic papillomas of the bladder include painless hematuria which can either be gross or microscopic.
How is Exophytic Papillomas of the Bladder Diagnosed?
Exophytic papillomas of the bladder are diagnosed by ultrasound, cystoscopy, and biopsy.
How are Exophytic papillomas of the bladder Treated?
Exophytic papillomas of the bladder are treated by resection such as transurethral resection of bladder tumor (TURBT).
What is the Prognosis of Exophytic Papillomas of the Bladder?
The prognosis of exophytic papillomas of the bladder is fair.
What is Inverted Papilloma of the Bladder?
Inverted papilloma of the bladder is a rare non-invasive endophytic urothelial tumor of the urinary bladder accounting for less than 1% of urothelial neoplasms.
What is the Pathology of Inverted Papilloma of the Bladder?
The pathology of Inverted papilloma of the bladder is:
-Etiology: The etiology of inverted urothelial papilloma of the bladder remains unknown.
-Genes involved: FGFR.
-Pathogenesis: The sequence of events that lead to Inverted papilloma of the bladder is the finding of nonrandom inactivation of X chromosomes is well documented which suggests that inverted papilloma is a clonal neoplasm that arises from a single progenitor cell.
-Morphology: The morphology associated with inverted papilloma of the bladder shows solitary, smooth, polypoid, sessile, or pedunculated. Usually, 3 cm or less but can be as large as 8 cm.
-Histology: The histology associated with inverted papilloma of the bladder shows normal urothelial lining, uniformity of urothelial cells, absent or infrequent mitosis, microcyst formation, and squamous metaplasia.
How does Inverted Papilloma of the Bladder Present?
Patients with inverted papilloma of the bladder typically affect males 5 times more than females in 50 to 60 years of age. The clinical features of inverted urothelial papilloma of the bladder are not specific but may include dysuria, flank pain, low back pain, occasional pyuria, or vague abdominal discomfort.
How is Inverted Papilloma of the Bladder Diagnosed?
Inverted papilloma of the bladder is diagnosed by imaging studies or cystoscopy during the evaluation of other conditions like benign prostatic hyperplasia, hematuria, or prostate cancer. Although ultrasonography of the bladder may detect a bladder mass, cystoscopy remains the diagnostic procedure of choice.
How is Inverted Papilloma of the Bladder Treated?
Inverted papilloma of the bladder is treated by simple excision which is curative.
What is the Prognosis of Inverted Papilloma of the Bladder?
The prognosis of inverted urothelial papilloma is fair depending upon intervention.
What is Papillary Urothelial Neoplasm of Low Malignant Potential?
Papillary urothelial neoplasm of low malignant potential is an exophytic (outward growing), (microscopically) nipple-shaped (or papillary) pre-malignant growth of the lining of the upper genitourinary tract (the urothelium), which includes the renal pelvis, ureters, urinary bladder, and part of the urethra.
What is the Pathology of Papillary Urothelial Neoplasm of Low Malignant Potential?
The pathology of Papillary urothelial neoplasm of low malignant potential is:
-Etiology: The cause of Papillary urothelial neoplasm of low malignant potential is unknown.
-Genes involved: No specific genes are involved.
-Pathogenesis: The sequence of events that lead to Papillary urothelial neoplasm of low malignant potential is an increased cellular proliferation that exceeds the thickness of normal urothelium and appears to lack the capacity to invade or metastasize.
-Morphology: The morphology associated with papillary urothelial neoplasm of low malignant potential shows 1-2 cm regular polypoid tumors.
-Histology: The histology associated with Papillary urothelial neoplasm of low malignant potential shows an orderly arrangement of cells within papillae with minimal architectural abnormalities and minimal nuclear atypia, regardless of cell thickness.
How does Papillary Urothelial Neoplasm of Low Malignant Potential Present?
Patients with Papillary urothelial neoplasm of low malignant potential typically affect males at 65 years of age. The symptoms, features, and clinical findings associated with Papillary urothelial neoplasm of low malignant potential shows microscopic hematuria.
How is Papillary Urothelial Neoplasm of Low Malignant Potential Diagnosed?
Papillary urothelial neoplasm of low malignant potential is diagnosed by cystoscopy.
How is Papillary Urothelial Neoplasm of Low Malignant Potential Treated?
Papillary urothelial neoplasm of low malignant potential is treated like non-invasive low-grade papillary urothelial carcinomas, excision, and regular follow-up cystoscopies.
What is the Prognosis of Papillary Urothelial Neoplasm of Low Malignant Potential?
The prognosis of papillary urothelial neoplasm of low malignant potential is fair with 10 percent survival rates.
What is Low-Grade Papillary Urothelial Carcinoma?
Low-grade papillary urothelial carcinoma is a urothelial neoplasm composed of papillary fronds, which exhibit an overall orderly appearance but have mild variability in architectural and/or cytologic features.
What is the Pathology of Low-Grade Papillary Urothelial Carcinoma?
The pathology of low grade papillary urothelial carcinoma is:
-Etiology: The cause of low grade papillary urothelial carcinoma is smoking, occupational exposure to chlorinated hydrocarbons, polycyclic aromatic hydrocarbons and aromatic amines, arsenic exposure.
-Genes involved: FGFR3, PIK3CA, PTEN.
-Pathogenesis: The sequence of events that lead to Low grade papillary urothelial carcinoma is the genetic alterations.
-Morphology: The morphology associated with low grade papillary urothelial carcinoma shows exophytic papillary lesions, single or multiple; can vary greatly in size.
-Histology: The histology associated with Low grade papillary urothelial carcinoma shows neoplastic urothelium lining fibrovascular cores, long, slender papillae with minimal fusing or branching.
How does Low-Grade Papillary Urothelial Carcinoma Present?
Patients with Low grade papillary urothelial carcinoma typically affect males 2 times more than females at 70 years of age. The symptoms, features, and clinical findings associated with low grade papillary urothelial carcinoma include painless hematuria (gross or microscopic) and gross hematuria associated with more advanced pathologic stage.
How is Low-Grade Papillary Urothelial Carcinoma Diagnosed?
Low-grade papillary urothelial carcinoma is diagnosed by cystoscopy, ultrasound, CT scan, and biopsy.
What is the Prognosis of Low Grade Papillary Urothelial Carcinoma?
The prognosis of low grade papillary urothelial carcinoma is poor with a high mortality rate.
What is High-Grade Papillary Urothelial Carcinoma?
High-grade papillary urothelial carcinoma is neoplastic proliferation of the urothelium with a papillary configuration and no invasion beyond the basement membrane.
What is the Pathology of High-Grade Papillary Urothelial Carcinoma?
The pathology of high grade papillary urothelial carcinoma is:
-Etiology: The cause of high grade papillary urothelial carcinoma is smoking, occupational exposure to chlorinated hydrocarbons, polycyclic aromatic hydrocarbons and aromatic amines, arsenic exposure.
-Genes involved: TP53, PIK3CA, TSC1, HRAS, APC.
-Pathogenesis: The sequence of events that lead to high-grade papillary urothelial carcinoma is genetic alterations.
-Histology: The histology associated with high grade papillary urothelial carcinoma shows fibrovascular cores lined by neoplastic urothelium, complex, solid to fused papillae common.
How does High-Grade Papillary Urothelial Carcinoma Present?
Patients with high-grade papillary urothelial carcinoma typically affect males more than females at 70 years of age. The symptoms, features, and clinical findings associated with high-grade papillary urothelial carcinoma include painless, intermittent hematuria, gross hematuria associated with a more advanced pathologic stage.
How is High-Grade Papillary Urothelial Carcinoma Diagnosed?
High-grade papillary urothelial carcinoma is diagnosed by cystoscopy, ultrasound, CT scan, and biopsy.
How is High-Grade Papillary Urothelial Carcinoma Treated?
High grade papillary urothelial carcinoma is treated by transurethral resection of the tumor.
What is the Prognosis of High Grade Papillary Urothelial Carcinoma?
The prognosis of high grade papillary urothelial carcinoma is poor with a high mortality rate.
What is Carcinoma in Situ of the Bladder?
Carcinoma in situ of the bladder is a flat lesion composed of cells in mid to upper epithelium with high cytologic grade. By definition, no invasion into lamina propria.
What is the Pathology of Carcinoma in Situ of the Bladder?
The pathology of carcinoma in situ of the bladder is:
-Etiology: The cause of carcinoma in situ of the bladder is usually de-novo synthesis although smoking can be a risk factor.
-Genes involved: HER2.
-Pathogenesis: The sequence of events that lead to carcinoma in situ of the bladder is the intact surface cells before progressive proliferation results in a tumor mass, recognition of early neoplastic alteration before a papillary structure forms is unlikely and most of the evidence is spatially based upon urothelial changes adjacent to papillary tumors.
-Morphology: The morphology associated with carcinoma in situ of the bladder shows flat, grossly erythematous, granular, or cobblestone mucosa.
-Histology: The histology associated with carcinoma in situ of the bladder shows flat lesion composed of cells with large, irregular, hyperchromatic nuclei, prominent nuclear pleomorphism, high N/C ratio, mitotic figures in mid to upper epithelium.
How does Carcinoma in Situ of the Bladder Present?
Patients with carcinoma in situ of the bladder typically affect males between 50-70 years of age. The symptoms, features, and clinical findings associated with carcinoma in situ of the bladder include dysuria, nocturia, urinary frequency, and urgency with microscopic hematuria. Cystoscopic findings may range from unremarkable to erythema or edema.
How is Carcinoma in Situ of the Bladder Diagnosed?
Carcinoma in situ of the bladder is diagnosed by urine cytology.
How is Carcinoma in situ of the bladder Treated?
Carcinoma in situ of the bladder is treated by BCG therapy or intravesical hyperthermia and mitomycin-C, local resection, or total cystectomy.
What is the Prognosis of Carcinoma in Situ of the Bladder?
The prognosis of carcinoma in situ of the bladder is poor in patients with coexisting noninvasive papillary urothelial carcinoma.
What is Adenocarcinoma of the Bladder?
Adenocarcinoma of the bladder is carcinoma derived from the urothelium and showing pure glandular differentiation, not including urachal adenocarcinoma or urothelial carcinoma with glandular differentiation.
What is the Pathology of Adenocarcinoma of the Bladder?
The pathology of Adenocarcinoma of the bladder is:
-Etiology: The causes of Adenocarcinoma of the bladder is the progression of extensive intestinal metaplasia (cystitis glandularis) or villous adenoma.
-Genes involved: TP53, KRAS, PIK3CA, CTNNB1, APC, and the promoter of TERT.
-Pathogenesis: The sequence of events that lead to Adenocarcinoma of the bladder is the metaplasia of the urinary bladder induced by chronic irritation or infection that can lead to adenocarcinoma.
-Morphology: The morphology associated with adenocarcinoma of the bladder shows 67% are solitary lesions (while urothelial carcinoma tends to be multifocal), tumor surface may be covered by gelatinous material, papillary, nodular, flat, or ulcerated.
-Histology: The histology associated with adenocarcinoma of the bladder shows nests of neoplastic cells floating in abundant extravasated mucin.
How does Adenocarcinoma of the Bladder Present?
Patients with adenocarcinoma of the bladder typically affect males more than females at 68 years of age. The symptoms, features, and clinical findings associated with adenocarcinoma of the bladder include hematuria, rarely with mucusuria, dysuria. Patients are older and mucusuria is more common than in urachal adenocarcinoma.
How is Adenocarcinoma of the Bladder Diagnosed?
Adenocarcinoma of the bladder is diagnosed by urine cytology, CT, MRI, and biopsy.
How is Adenocarcinoma of the Bladder Treated?
Adenocarcinoma of the bladder is treated by radical cystectomy and pelvic lymph node dissection.
What is the Prognosis of Adenocarcinoma of the Bladder?
The prognosis of adenocarcinoma of the bladder variable.
What is Mixed Carcinoma of the Bladder?
Mixed carcinoma of the bladder is mixed high- and low-grade carcinoma of the bladder.
What is the Pathology of Mixed Carcinoma?
The pathology of mixed carcinoma is:
-Etiology: The etiology of mixed carcinoma is environmental exposure.
-Genes involved: FGFR-3, Ras, PIK3CA, PTEN.
-Pathogenesis: The sequence of events that lead to Mixed carcinoma is the molecular pathways that are likely responsible for the development of noninvasive and invasive bladder tumors.
-Morphology: The morphology associated with mixed carcinoma shows variable features.
-Histology: The histology associated with mixed carcinoma shows features of both high grade and low-grade tumors.
How does Mixed Carcinoma Present?
Patients with mixed carcinoma typically affect males. The symptoms, features, and clinical findings associated with mixed carcinoma include painless gross hematuria.
How is Mixed Carcinoma Diagnosed?
Mixed carcinoma is diagnosed by cytology, imaging, and biopsy.
How is Mixed Carcinoma Treated?
Mixed carcinoma is treated by surgical resection.
What is the Prognosis of Mixed Carcinoma?
The prognosis of mixed carcinoma is variable.
What is Sarcoma of the Bladder?
Sarcoma of the bladder is a variant of urothelial carcinoma; morphologically indistinguishable from sarcoma.
What is the Pathology of Sarcoma of the Bladder?
The pathology of sarcoma of the bladder is:
-Etiology: The cause of the sarcoma of the bladder has a malignant clonal origin, with epithelial and mesenchymal differentiation.
-Genes involved: FOXC2, SNAIL, and ZEB1 TERT C228T TP53.
-Pathogenesis: The sequence of events that lead to the Sarcoma of the Bladder is the TERT C228T promoter mutations in 35% of sarcomatoid carcinoma result in epithelial and mesenchymal differentiation.
-Morphology: The morphology associated with Sarcoma of the Bladder shows a gray fleshy cut surface with infiltrative margins similar to sarcoma in appearance.
-Histology: The histology associated with Sarcoma of the Bladder shows most common component is undifferentiated high-grade spindle cell sarcoma, sarcomatoid areas admixed with conventional high-grade urothelial carcinoma.
How does Sarcoma of the Bladder Present?
Patients with sarcoma of the bladder typically affect males two or three times more than females in 45 to 82 years of age. The symptoms, features, and clinical findings associated with sarcoma of the Bladder include gross hematuria, flank pain, an abdominal mass, and hydronephrosis, similar to those of conventional urothelial tumors.
How is Sarcoma of the Bladder Diagnosed?
Sarcoma of the bladder is diagnosed through cystoscopy, CT scan, MRI, and biopsy.
How is Sarcoma of the Bladder Treated?
Sarcoma of the bladder treatment is not standard due to rarity. It is chemotherapy-resistant.
What is the Prognosis of Sarcoma of the Bladder?
The prognosis of the sarcoma of the bladder is poor, as it frequently presents at an advanced stage and is associated with a worse overall survival when compared with pure urothelial carcinoma.
What is Small Cell Carcinoma of the Bladder?
Small cell carcinoma of the bladder is a very rare, poorly differentiated neuroendocrine epithelial bladder tumor characterized clinically by hematuria and/or dysuria and a highly aggressive course.
What is the Pathology of Small Cell Carcinoma of the Bladder?
The pathology of small cell carcinoma of the bladder is:
-Etiology: The etiology of the disease is unknown.
-Genes involved: Overexpression of DLL3 mRNA and protein.
-Pathogenesis: The sequence of events that lead to small cell carcinoma of the bladder is from a multipotent stem cell.
-Morphology: The morphology associated with small cell carcinoma of the bladder shows unifocal mass centered in the renal pelvis, usually invading perinephric adipose tissue, composed of small cells.
-Histology: The histology associated with small cell carcinoma of the bladder shows diffuse growth of small cells with nuclear molding, minimal cytoplasm, indistinct nucleoli, high mitotic activity, and apoptotic bodies.
How does the Small Cell Carcinoma of the Bladder Present?
Patients with small cell carcinoma of the bladder typically affect males between 59 to 65 years of age. The symptoms, features, and clinical findings associated with small cell carcinoma of the bladder include gross hematuria with dysuria as the second most common symptom.
How is Small Cell Carcinoma of the Bladder Diagnosed?
The small cell carcinoma of the bladder is diagnosed by histopathological data and cystoscopy.
How is Small Cell Carcinoma of the Bladder Treated?
The small cell carcinoma of the bladder is treated with surgical excision.
What is the Prognosis of Small Cell Carcinoma of the Bladder?
The prognosis of small cell carcinoma of the bladder is poor mainly in the case of pure small cell carcinoma.
Urethra pathology:
What is Inflammation of the Urethra?
Inflammation of the urethra is urethritis. Urethritis is typically due to gonococcal or non-gonococcal etiologies.
What is Gonococcal Urethritis?
Gonococcal urethritis is the inflammation of the urethra and is a lower urinary tract.
What is the Pathology of Gonococcal Urethritis?
The pathology of gonococcal urethritis is:
-Etiology: The cause of gonococcal urethritis is Neisseria gonorrhoeae is the leading cause of urethritis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gonococcal urethritis is the periurethral microabscesses.
-Morphology: The morphology associated with gonococcal urethritis shows inflamed urethra.
-Histology: The histology associated with gonococcal urethritis shows polymorphonuclear leukocytes.
How does Gonococcal Urethritis Present?
Patients with gonococcal urethritis typically affect males and females in adolescence and adulthood. The symptoms, features, and clinical findings associated with gonococcal urethritis include dysuria, pruritus, burning, and discharge at the urethral meatus.
How is Gonococcal Urethritis Diagnosed?
Gonococcal urethritis is diagnosed by a urine test, blood test, vaginal culture, cystoscopy, or nucleic acid test.
How is Gonococcal Urethritis Treated?
Gonococcal urethritis is treated by ceftriaxone and azithromycin.
What is the Prognosis of Gonococcal Urethritis?
The prognosis of gonococcal urethritis is excellent with treatment.
What is Non-gonococcal Urethritis?
Non-gonococcal urethritis, inflammation of the urethra, is the most common sexually transmitted illness in men. Urethritis can be infectious or non-infectious.
What is the Pathology of Non-Gonococcal Urethritis?
The pathology of non-gonococcal urethritis is:
-Etiology: The most common cause of non-gonococcal urethritis is Chlamydia trachomatis, mycoplasma genitalium.
-Genes involved: None, non-gonococcal urethritis is an infectious disease.
-Pathogenesis: The sequence of events that lead to Non-gonococcal Urethritis is chlamydia. C. trachomatis typically infects columnar epithelial cells at mucosal sites. It replicates in host cells eventually causing cell death.
-Morphology: The morphology associated with Non-gonococcal Urethritis shows mucopurulent discharge.
-Histology: The histology associated with Non-gonococcal Urethritis shows polymorphonuclear leukocytes without the presence of intracellular gram-negative diplococci on gram stain.
How does Non-Gonococcal Urethritis Present?
Patients with non-gonococcal urethritis typically affect men in adolescence or adulthood. The symptoms, features, and clinical findings associated with non-gonococcal urethritis include pain or a burning sensation upon urination (dysuria), a white/cloudy discharge, and a feeling that one needs to pass urine frequently.
How is Non-Gonococcal Urethritis Diagnosed?
Non-gonococcal urethritis is diagnosed through gram stain of the urethral discharge under a microscope.
How is Non-Gonococcal Urethritis Treated?
Non-gonococcal urethritis is treated with antibiotics.
What is the Prognosis of Non-gonococcal Urethritis?
The prognosis of non-gonococcal urethritis is good. It is generally a self-limited disease and resolves, even without therapy, with no complications in most cases.
What are Tumors of the Urethra?
Tumors of the urethra are neoplastic proliferation forming tumors in the urethra.
Examples of tumors of the urethra include:
Urethral caruncle
What is Urethral Caruncle?
The urethral caruncle is a benign cutaneous condition characterized by distal urethral lesions that are most commonly found in post-menopausal women. They appear red and can be of various sizes. These epidermal growths are found around the posterior portion of the urethral meatus.
What is the Pathology of Urethral Caruncle?
The pathology of the urethral caruncle is:
-Etiology: The cause of urethral caruncle is reduced estrogenization of urethral smooth muscle.
-Genes involved: Not well-understood.
-Pathogenesis: The sequence of events that lead to urethral caruncle is urogenital atrophy due to estrogen deficiency.
-Morphology: The morphology associated with the Urethral caruncle appears red, and can be of various sizes. They can have the appearance of a tumor. These epidermal growths are found around the posterior portion of the urethral meatus.
-Histology: The histology associated with the urethral caruncle shows papillomatous, angiomatous, and granulomatous.
How does Urethral Caruncle Present?
Patients with urethral caruncle typically affect females in the post-menopausal age group. The symptoms, features, and clinical findings associated with urethral caruncle include dysuria, urinary frequency, obstructive symptoms.
How is Urethral Caruncle Diagnosed?
A urethral caruncle is obvious on physical examination. Additionally, cystoscopy can be helpful.
How is Urethral Caruncle Treated?
The urethral caruncle is treated by excision.
What is the Prognosis of Urethral Caruncle?
The prognosis of the urethral caruncle is excellent if pathology confirms the urethral caruncle as the diagnosis.