Agammaglobulinemia aka Bruton agammaglobulinemia is an inherited (genetic) immune system disorder that reduces your ability to fight infections. Agammaglobulinemia is caused by a genetic mutation in a gene called Bruton’s tyrosine kinase.
What is the Pathology of X-linked Agammaglobulinemia?
The pathology of X-linked agammaglobulinemia is:
-Aetiology: The cause of disease X-linked agammaglobulinemia is a gene defect that blocks the growth of normal, mature immune cells called B lymphocytes.
-Pathogenesis: The sequence of events that lead to X-linked agammaglobulinemia are is Bruton tyrosine kinase deficiency causes a failure of B cell development in affected individuals. Immunoglobulin-secreting plasma cells also are absent, deficiency of immunoglobulins results in absent antibody responses and increases the tendency to develop bacterial infections.
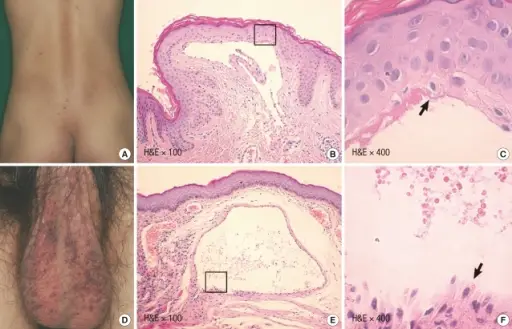
-Morphologic changes in the X-linked agammaglobulinemia involves people with XLA have very small tonsils and lymph nodes. This is because tonsils and lymph nodes are made up of B lymphocytes. In people with XLA, the size of these tissues is reduced because of the absence of B lymphocytes.
How does X-linked Agammaglobulinemia Present?
Patients with X-linked agammaglobulinemia typically affects males because it is unlikely that females will have two altered copies of the gene because it is x-linked. Patients with XLA can clinically present when they are aged 3 months to 5 years because new born cannot produce their own Ig. The symptoms, features, and clinical findings associated with X-linked agammaglobulinemia include: nasal infections, skin infections, meningitis, bronchitis, pneumonia, sepsis, or infection of the blood stream.
How is X-linked Agammaglobulinemia Diagnosed?
X-linked agammaglobulinemia is diagnosed by electrophorphoresis. The diagnosis is confirmed by the absence of BTK protein in monocytes or platelets or by the detection of a mutation in BTK in DNA by using polymerase chain reaction (PCR)-based single-strand conformation polymorphism (SSCP).
How is X-linked Agammaglobulinemia Treated?
X-linked agammaglobulinemia has no cure, but the condition may be treated. Immunoglobulin replacement therapy is a life-long and life-prolonging treatment that restores some of the missing antibodies. Daily oral antibiotics are also utilized to prevent or treat infections.
What is the Prognosis of X-linked Agammaglobulinemia?
The prognosis of X-linked agammaglobulinemia is good as long as patients are diagnosed and treated early with regular intravenous gamma globulin therapy before the sequelae of recurrent infections appear.