Salivary gland pathology diseases or disorders that may happen to the salivary glands.
What are Salivary Glands?
Salivary glands are glands that produce secretions which aid in lubrication and digestion.
There are four types of salivary glands, three major and one minor which include:
- Major
- Parotid
- Submandibular
- Sublingual
- Minor
- Others
The main types of salivary gland pathology includes:
- Xerostomia
- Sialadenitis
- Salivary gland neoplasms
What is Xerostomia?
Xerostomia is defined as a dry mouth resulting from reduced or absent saliva flow. Xerostomia is commonly associated with Sjogren’s syndrome.
What is the Pathology of Xerostomia?
The pathology of xerostomia is:
-Etiology: Xerostomia may be caused by autoimmune, traumatic, or drug related conditions.
-Pathogenesis: The sequence of events that lead to xerostomia imay be immune related issues, or suppression from the CNS, or muscarinic or adrenergic receptor stimulation.
-Histology: The histology associated with xerostomia shows lymphoid infiltration with germinal centers, acinar atrophy, and interstitial fibrosis.
How does Xerostomia Present?
Patients with xerostomia typically are middle aged females. The symptoms, features, and clinical findings associated with xerostomia include often dry mouth, dry eyes, and coughing.
How is Xerostomia Diagnosed?
Xerostomia is diagnosed based on physical exam, and lab tests for autoimmune conditions.
How is Xerostomia Treated?
Xerostomia is treated by the identification and resolution of the underlying cause.
What is the Prognosis of Xerostomia?
The prognosis of xerostomia is good.
What is Sialadenitis?
Sialadenitis is an infection or inflammation of the salivary glands.
What is the Pathology of Sialadenitis?
The pathology of sialadenitis is:
-Etiology: The cause of sialadenitis is most commonly by sialolithiasis, bacterial or viral infections.
-Pathogenesis: The sequence of events that lead to sialadenitis involves inflammation of the salivary glands.
-Histology: The histology associated with sialadenitis shows stones that are readily visualized as high attenuating masses. There may be edema, hyperemia, and acute inflammation with dense lymphohistiocytic infiltrate.
How does Sialadenitis Present?
Patients with sialadenitis are typically males of varying age ranges. The symptoms, features, and clinical findings associated with sialadenitis include pain and swelling.
How is Sialadenitis Diagnosed?
Sialadenitis is diagnosed by physical exam, and biopsy.
How is Sialadenitis Treated?
Sialadenitis is treated by antimicrobial therapy.
What is the Prognosis of Sialadenitis?
The prognosis of sialadenitis is very good.
What is a Mucocele?
A mucocele is an oral lesion that is typically due to trauma.
What is the Pathology of Mucocele?
-The pathology of mucocele is:
-Etiology: The cause of mucocele is most often when a patient repeated trauma such as bites or sucking.
-Pathogenesis: The sequence of events that lead to mucoceles is the disruption of saliva flow from the salivary glands.
-Morphology: Small bump.
-Histology: The histology associated with mucocele shows intact pseudocyst cavity containing mucin, abundant epithelioid foamy histiocytes, neutrophils, and granulation tissue.
How does Mucocele Present?
Patients with mucoceles are typically younger, and are either male or female. The symptoms, features, and clinical findings associated with mucocele include painless, soft, round, dome-shaped, lesions that typically have pearly or clear or blue hues.
How is Mucocele Diagnosed?
Mucocele is diagnosed mainly based on the clinically by physical exam, and perhaps a biopsy.
How is Mucocele Treated?
Mucocele is treated by lifestyle changes, symptomatic management, or excisions.
What is the Prognosis of Mucocele?
The prognosis of mucocele is good.
What is a Ranula?
A ranula is a fluid collection or cyst that typically form under the tongue.
What is the Pathology of Ranula?
The pathology of ranula is:
-Etiology: The cause of ranula is disruption of flow of secretions from salivary glands.
-Pathogenesis: The sequence of events that lead to ranulas is when one of the salivary glands, usually the sublingual gland, is injured or diseased and the saliva no longer reaches the external surface of the mouth.
-Morphology: Oral lesion.
-Histology: The histology associated with ranula shows a well-delineated cavity that contains free mucinous material, the cavity wall lacking an epithelial lining.
How does Ranula Present?
Patients with ranula are typically male or female that are typically younger. The symptoms, features, and clinical findings associated with ranula include large, swelling, cystic, translucent to blue lesions on the floor of the mouth.
How is Ranula Diagnosed?
Ranula is diagnosed primarily by physical examination.
How is Ranula Treated?
Ranula is treated by open surgical drainage or removal.
What is the Prognosis of Ranula?
The prognosis of ranula is good.
What is Sialolithiasis?
Sialolithiasis is a benign condition and it’s characterized by salivary stones obstructing the duct.
What is the Pathology of Sialolithiasis?
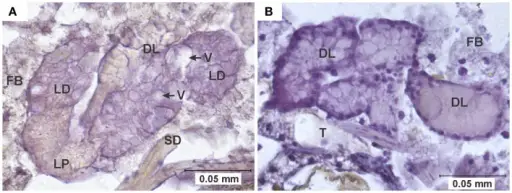
The pathology of sialolithiasis is:
-Etiology: The cause of sialolithiasis is a stone obstructing a salivary duct.
-Pathogenesis: The sequence of events that lead to sialolithiasis is unclear and may be due to multiple intracellular microcalculi that block salivary gland outflow.
-Histology: The histology associated with sialolithiasis shows varying degrees of acinar destruction. There may be inflammation and fibrosis.
How does Sialolithiasis Present?
Patients with sialolithiasis typically are male present at the age range of 30 – 60 years old. The symptoms, features, and clinical findings associated with sialolithiasis include intermittent, pain and swelling of a salivary gland.
How is Sialolithiasis Diagnosed?
Sialolithiasis is diagnosed by physical exam and imaging.
How is Sialolitiasis Treated?
Sialolithiasis is treated by oral pain medication and antibiotics. Some circumstances may warrant surgical management.
What is the Prognosis of Sialolithiasis?
The prognosis of sialolithiasis is good.
What are Salivary Gland Neoplasms?
Salivary neoplasms are among the most cytomorphologically diverse human neoplasms. Among salivary gland neoplasms 80 % arise in the parotid glands, 10 – 15 % arise in the submandibular glands, and the remainder arise in the sublingual and minor salivary glands.
Salivary gland neoplasms can be benign or malignant.
Examples of Benign salivary gland neoplasms include:
- Basal cell adenoma
- Canalicular adenoma
- Ductal papillomas
- Pleomorphic adenoma
- Oncocytoma
- Warthin tumor
What is Basal Cell Adenoma?
Basal cell adenoma is an uncommon type of monomorphous adenoma.
What is the Pathology of Basal Cell Adenoma?
The pathology of basal cell adenoma is:
-Etiology: The cause of basal cell adenoma is unknown.
-Genes involved: CTNNB1 mutations, CYLD1 mutations
-Pathogenesis: The sequence of events that lead to basal cell adenoma is unknown.
-Histology: The histology associated with basal cell adenoma shows 2 types of cells which include basaloid cells and luminal cells. Fibrocellular stroma may also be present.
How does Basal Cell Adenoma Present?
Patients with basal cell adenoma typically are women present at an age range of between their fifth and seventh decades of life. The symptoms, features, and clinical findings associated with basal cell adenoma include a firm and mobile, slow growing, painless mass.
How is Basal Cell Adenoma Diagnosed?
Basal cell adenoma is diagnosed by imaging, fine needle aspiration, and biopsy.
How is Basal Cell Adenoma Treated?
Basal cell adenoma is treated by a surgical excision.
What is the Prognosis of Basal Cell Adenoma?
The prognosis of basal cell adenoma is good.
What is Canalicular Adenoma?
Canalicular adenoma is a benign neoplasm of salivary glands.
What is the Pathology of Canalicular Adenoma?
The pathology of canalicular adenoma is:
-Etiology: The cause of canalicular adenoma may be related to alcohol use or smoking.
-Genes involved: CD117, BCL2, p63
-Pathogenesis: The sequence of events that lead to canalicular adenoma is unknown.
-Morphology: Well-circumscribed small nodule.
-Histology: Bilayered basaloid epithelial cells that make interconnected cords. There are also rows and tubular structures. Cystic dilation of canalicular structures may also be present edematous paucicellular stroma.
How does Canalicular Adenoma Present?
Patients with canalicular adenoma typically are females present at age range of from the 4th to 9th decades of life. The symptoms, features, and clinical findings associated with canalicular adenoma include a painless mass that may be swollen.
How is Canalicular Adenoma Diagnosed?
Canalicular adenoma is diagnosed by physical exam and biopsy.
How is Canalicular Adenoma Treated?
Canalicular adenoma is treated by complete surgical excision.
What is the Prognosis of Canalicular Adenoma?
The prognosis of canalicular adenoma is good if properly treated
What is Ductal Papillomas?
Ductal papillomas are benign papillary neoplasms that generally occur in minor salivary glands. They include both intraductal papillomas and inverted ductal papillomas.
What is the Pathology of Ductal Papillomas?
The pathology of ductal papillomas is:
-Etiology: The cause of ductal papillomas is unknown, though some authors have related it to human papillomavirus (HPV) infection.
-Genes: Unknown.
-Pathogenesis: The sequence of events that lead to ductal papillomas is papillomatous proliferation due to neoplastic proliferation of any epithelium of the ductal system.
-Histology: Unicystic lesions lined by papillary proliferation with bland cuboidal to columnar epithelial cells with fibrovascular cores.
How does Ductal Papillomas Present?
Patients with ductal papillomas typically are either male or female present at age range of adults. The symptoms, features, and clinical findings associated with ductal papillomas include painless submucosal lesions.
How is Ductal Papillomas Diagnosed?
Ductal papillomas is diagnosed by physical exam, imaging, and biopsy.
How is Ductal Papilloma Treated?
Ductal papillomas are treated by simple excision surgery.
What is the Prognosis of Ductal Papillomas?
The prognosis of ductal papillomas is fair.
What is Pleomorphic Adenoma?
Pleomorphic adenoma is the most common salivary gland tumor.
What is the Pathology of Pleomorphic Adenoma?
The pathology of pleomorphic adenoma is:
-Etiology: The cause of pleomorphic adenoma is cellular proliferation.
-Genes involved: PLAG1 fusion (chromosome 8q12) or HMGA2 fusion (chromosome 12q14-15).
-Pathogenesis: The sequence of events that lead to pleomorphic adenoma is the proliferation of myoepithelial and epithelial cells of the ducts and there is also a marked increase in stromal components.
-Histology: The histology associated with pleomorphic adenoma shows epithelial and myoepithelial tissue in a myxoid background.
How does Pleomorphic Adenoma Present?
Pleomorphic adenomas are more common in females. The symptoms, features, and clinical findings associated with pleomorphic adenoma include slow growing, painless, well circumscribed mass involving salivary gland.
How is Pleomorphic Adenoma Diagnosed?
Pleomorphic adenoma is diagnosed by physical exam, fine needle aspiration, and biopsy.
How is Pleomorphic Adenoma Treated?
Pleomorphic adenoma is treated by surgical excision.
What is the Prognosis of Pleomorphic Adenoma?
The prognosis of pleomorphic adenoma is fair.
What is Oncocytoma?
Oncocytoma is a rare salivary gland tumor consisting of oncocytes with many mitochondria.
What is the Pathology of Oncocytoma?
The pathology of oncocytoma is:
-Etiology: The cause of oncocytoma is related to viral insult.
-Pathogenesis: The sequence of events that lead to oncocytoma is not known.
-Histology: The histology associated with oncocytoma is benign epithelial tumors with oncocytes with eosinophilic granular cytoplasm that contain many mitochondria.
How does Oncocytoma Present?
Patients with oncocytoma typically are slightly predominant in female gender, present at age range of most commonly from the sixth to eighth decades. The symptoms, features, and clinical findings associated with oncocytoma include a lobulated, mobile mass.
How is Oncocytoma Diagnosed?
Oncocytoma is diagnosed by imaging, fine needle aspiration, and biopsy.
How is Oncocytoma Treated?
Oncocytoma is treated by complete surgical excision.
What is the Prognosis of Oncocytoma?
The prognosis of oncocytoma is fair.
What is Warthin Tumor?
Warthin tumor is a tumor that effects the parotid gland. Warthin tumor is also called papillary cystadenoma lymphomatosum papilliferum.
What is the Pathology of Warthin Tumor?
The pathology of Warthin tumor is:.
-Pathogenesis: The sequence of events that lead to Warthin tumor is unknown, but thought to be related to smoking.
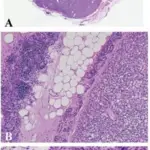
-Histology: The histology associated with Warthin tumor shows a double layer of epithelial cells and a dense lymphoid stroma. Variable germinal centers and cystic spaces may be present. There are polypoid projections of lymphoepithelial elements, and surface palisading of oncocytic columnar cells with adjacent basal cells.
How does Warthin Tumor Present?
Patients with Warthin tumor are typically older males that smoke. The symptoms, features, and clinical findings associated with Warthin tumor include a parotid mass.
How is Warthin Tumor Diagnosed?
Warthin tumor is diagnosed by physical exam, fine needle aspiration, and biopsy.
How is Warthin Tumor Treated?
Warthin tumor is treated by surgical excision.
What is the Prognosis of Warthin Tumor?
The prognosis of Warthin tumor is fair.
What is Acinic Cell Carcinoma?
Acinic cell carcinoma is a malignant epithelial neoplasm involving the the salivary glands.
What is the Pathology of Acinic Cell Carcinoma?
The pathology of acinic cell carcinoma is:
-Etiology: The cause of acinic cell carcinoma is unknown.
-Genes involved: Recurrent (t[4;9][q13;q31]) genomic rearrangement.
-Pathogenesis: The sequence of events that lead to acinic cell carcinoma is the growth of malignant cells.
-Histology: The histology associated with acinic cell carcinoma shows microcystic, solid, papillary cystic, or follicular growth of acinar cells. The cytoplasm may be granular to vacuolated. Nuclei tend to be eccentric and round. Nucleoli tend to be conspicuous.
How does Acinic Cell Carcinoma Present?
Patients with acinic cell carcinoma typically are more common females than males, and are middle aged. The symptoms, features, and clinical findings associated with acinic cell carcinoma include a slow growing painful mass.
How is Acinic Cell Carcinoma Diagnosed?
Acinic cell carcinoma is diagnosed by physical exam, imaging, and biopsy.
How is Acinic Cell Carcinoma Treated?
Acinic cell carcinoma is treated by complete surgical excision.
What is the Prognosis of Acinic Cell Carcinoma?
The prognosis of acinic cell carcinoma is fair to poor.
What is Adenocarcinoma of the Salivary Gland?
Adenocarcinoma is cancer that does not fit an exact classification and it can occur in the major salivary glands (usually the parotid glands) or in the minor salivary glands. A painless lump is the most common symptom. It appears in parotid gland, submandibular gland, palate or buccal mucosa.
What is the Pathology of Adenocarcinoma of the Salivary Gland?
The pathology of adenocarcinoma is:
-Etiology: The cause of adenocarcinoma may be smoking, or toxin related.
-Genes involved: EGFR gene amplification, high HER2 gene copy number, KRAS mutation
-Pathogenesis: The sequence of events that lead to adenocarcinoma is the classic malignant transformation.
-Histology: The histology associated with adenocarcinoma glandular or ductal features involved by malignant cells.
How does Adenocarcinoma of the Salivary Gland Present?
Patients with adenocarcinoma of the salivary glands are typically males, of a wide age range. The symptoms, features, and clinical findings associated with adenocarcinoma include a painless mass.
How is Adenocarcinoma of the Salivary Gland Diagnosed?
Adenocarcinoma is diagnosed by physical exam, laboratory testing, fine needle aspiration, and biopsy.
How is Adenocarcinoma of the Salivary Gland Treated?
Adenocarcinoma is treated by complete surgical excision.
What is the Prognosis of Adenocarcinoma of the Salivary Gland?
The prognosis of adenocarcinoma is poor. The 5 year survival rate is 60%
What is Adenoid Cystic Carcinoma?
Adenoid cystic carcinoma is a cancer of the salivary glands.
What is the Pathology of Adenoid Cystic Carcinoma?
The pathology of adenoid cystic carcinoma is:
-Etiology: The cause of adenoid cystic carcinoma is unknown.
-Genes involved: MYB, MYBL1 or NFIB gene
-Pathogenesis: The sequence of events that lead to adenoid cystic carcinoma is malignant glandular tissue.
-Histology: The histology associated with adenoid cystic carcinoma shows malignant ductal and myoepithelial cells. There is typically a cribriform pattern.
How does Adenoid Cystic Carcinoma Present?
Patients with adenoid cystic carcinoma are typically older. The symptoms, features, and clinical findings associated with adenoid cystic carcinoma include a firm growing mass.
How is Adenoid Cystic Carcinoma Diagnosed?
Adenoid cystic carcinoma is diagnosed by physical exam, fine needle aspiration, and biopsy.
How is Adenoid Cystic Carcinoma Treated?
Adenoid cystic carcinoma is treated by complete surgical resection. Radiation and chemotherapy may also be needed.
What is the Prognosis of Adenoid Cystic Carcinoma?
The prognosis of adenoid cystic carcinoma is poor, with a 5 year overall survival rate of 80%.
What is Malignant Mixed Tumor?
Malignant mixed tumor is a rare tumor of salivary glands.
What is the Pathology of Malignant Mixed Tumor?
The pathology of malignant mixed tumor is:
-Etiology: The cause of malignant mixed tumor is from a pre-existing benign mixed tumor that mutates.
-Genes involved: PLAG1, HMGA2, MDM2, HER2, HMGIC, and TP53.
-Pathogenesis: The sequence of events that lead to malignant mixed tumor is malignant transformation of glandular cells.
-Histology: The histology associated with malignant mixed tumor shows a carcinomatous component that may be salivary duct carcinoma, and a myoepithelial carcinoma or epithelial myoepithelial carcinoma.
How does Malignant Mixed Tumor Present?
Patients with malignant mixed tumor typically are older males. The symptoms, features, and clinical findings associated with malignant mixed tumor include a palpable mass in the salivary gland.
How is Malignant Mixed Tumor Diagnosed?
Malignant mixed tumor is diagnosed by physical exam, fine needle aspiration, and biopsy.
How is Malignant Mixed Tumor Treated?
Malignant mixed tumor is treated by surgical excision.
What is the Prognosis of Malignant Mixed Tumor?
The prognosis of malignant mixed tumor is poor, with a 15% 5 year survival rate.
What is Mucoepidermoid Carcinoma?
Mucoepidermoid carcinoma is a malignant glandular neoplasm of the salivary glands.
What is the Pathology of Mucoepidermoid Carcinoma?
The pathology of mucoepidermoid carcinoma is:
-Etiology: The cause of mucoepidermoid carcinoma thought o be due to environmental or genetic factors.
-Genes involved: MAML2 fusion
-Pathogenesis: The sequence of events that lead to mucoepidermoid carcinoma is malignant stem or progenitor cells in excretory ducts.
-Histology: The histology associated with mucoepidermoid carcinoma shows solid, cystic or mixed growth patterns that may have papillary or glandular growth patterns.
How does Mucoepidermoid Carcinoma Present?
Patients with mucoepidermoid carcinoma typically are females that are older. The symptoms, features, and clinical findings associated with mucoepidermoid carcinoma include a painless swelling mass that might cause slight pressure.
How is Mucoepidermoid Carcinoma Diagnosed?
Mucoepidermoid carcinoma is diagnosed by physical exam, fine needle aspiration, and biopsy.
How is Mucoepidermoid Carcinoma Treated?
Mucoepidermoid carcinoma is treated by complete surgical resection.
What is the Prognosis of Mucoepidermoid Carcinoma?
The prognosis of mucoepidermoid carcinoma is poor.
What is Squamous Cell Carcinoma of the salivary gland?
Squamous cell carcinoma of the salivary gland is a malignant epithelial tumor of the salivary gland.
What is the Pathology of Squamous Cell Carcinoma of the salivary gland?
The pathology of squamous cell carcinoma is:
-Etiology: The cause of squamous cell carcinoma of the salivary gland is unknown.
-Genes involved: TP53, p16
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma is due to carcinogenesis associated with TP53 genetic mutation, and p16 mutations.
-Histology: The histology associated with squamous cell carcinoma shows malignant squamous cells.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically are older males that smoke. The symptoms, features, and clinical findings associated with squamous cell carcinoma include a firm mass.
How is Squamous Cell Carcinoma Diagnosed?
Squamous cell carcinoma is diagnosed by physical eczema, fine needle aspiration, and biopsy.
How is Squamous Cell Carcinoma Treated?
Squamous cell carcinoma is treated by radical surgery and radiation therapy.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of squamous cell carcinoma is poor.