Pregnancy pathology is lesions or disorders that may occur to the fetus or placenta during pregnancy, or related conditions.
Pregnancy pathology includes:
- Disorders of early pregnancy
- Disorders of late pregnancy
- Gestational trophoblastic disease
What are Disorders of Early Pregnancy?
Disorders of early pregnancy are medical issues that arise early in pregnancy that may result in pregnancy termination.
Examples of disorders of early pregnancy include:
- Ectopic pregnancy
- Spontaneous abortion
What is Ectopic Pregnancy?
Ectopic pregnancy is the extrauterine implantation of a fertilized egg.
What is the Pathology of Ectopic Pregnancy?
The pathology of ectopic pregnancy is:
-Etiology: The cause of ectopic pregnancy is a pelvic inflammatory disease
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ectopic pregnancy includes four mechanisms including anatomic obstruction preventing passage of the zygote, abnormal conceptus, tubal motility abnormalities, zygote transperitoneal migration.
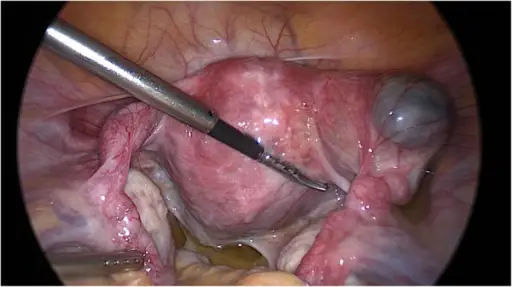
-Morphology: The morphology associated with ectopic pregnancy shows fallopian tubes which are a pair of hollow tubes attached one on each side of the uterus through which the egg travels from the ovary to the uterus.
-Histology: The histology associated with ectopic pregnancy shows the presence of extrauterine chorionic villi or extravillous trophoblast
How does Ectopic Pregnancy Present?
Patients with ectopic pregnancy typically affect females present at the age range of 15-45 years. The symptoms, features, and clinical findings associated with ectopic pregnancy include vaginal bleeding or abdominal pain.
How is Ectopic Pregnancy Diagnosed?
Ectopic pregnancy is diagnosed using visualization of an extrauterine gestational sac by transvaginal ultrasound (TVUS) or histologic confirmation.
How is Ectopic Pregnancy Treated?
Ectopic pregnancy is treated by surgical management (typically salpingectomy or salpingotomy) for hemodynamically unstable patients and methotrexate.
What is the Prognosis of Ectopic Pregnancy?
The prognosis of ectopic pregnancy is poor if not treated in time.
What is Spontaneous Abortion?
Spontaneous abortion is a naturally occurring intrauterine loss.
What is the Pathology of Spontaneous Abortion?
The pathology of spontaneous abortion is:
-Etiology: The cause of spontaneous abortion is fetal factors which include genetic abnormalities, anatomic issues, infectious organisms, or autoimmune conditions.
-Genes involved: Trisomies. Monosomys.
-Pathogenesis: The sequence of events that lead to spontaneous abortion includes chromosomal defects occurring in 4-8 weeks of gestation.
-Morphology: The morphology associated with spontaneous abortion shows a soft hemorrhagic mass of villi and decidua that may be attached to membranes as an intact or ruptured gestational sac.
-Histology: The histology associated with spontaneous abortion shows decidual necrosis and decidual blood vessel thrombi, neutrophilic infiltrate, old/recent hemorrhage, and edematous avascular villi.
How does Spontaneous Abortion Present?
Patients with spontaneous abortion typically affect females present at the age range of 15-45 years. The symptoms, features, and clinical findings associated with spontaneous abortion include crampy pelvic pain, bleeding, and eventual expulsion of tissue.
How is Spontaneous Abortion Diagnosed?
Spontaneous abortion is diagnosed with ultrasound and blood tests.
How is Spontaneous Abortion Treated?
Spontaneous abortion is treated by dialation and curettage (D&C) to remove residual trophoblastic tissue. This is done to confirm intrauterine pregnancy and rule out gestational trophoblastic disease or molar abnormalities.
What is the Prognosis of Spontaneous Abortion?
The prognosis of spontaneous abortion is good, although the female may experience further bouts of spontaneous abortion in the future.
What are Disorders of Late Pregnancy?
Disorders of late pregnancy are health issues that arise late in pregnancy.
Examples of disorders of late pregnancy include:
- Abnormalities of placental implantation
- Preeclampsia
- Eclampsia
- Placental infections
- Twin placentas
What are Abnormalities of Placental Implantation?
Abnormalities of placental Implantation are the large group of disorders that are associated with significant maternal, fetal, and neonatal morbidity such as placenta previa, placenta accrete, vasa previa, and velamentous cord insertion.
What is the Pathology of Abnormalities of Placental Implantation?
The pathology of abnormalities of placental implantation is:
-Etiology: The cause of abnormalities of placental implantation is blood flow problems.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to abnormalities of placental implantation shows decreased or absent decidualized endometrium resulting in abnormal implantation and increased placental adhesion.
-Morphology: The morphology associated with abnormalities of placental implantation shows low-lying placenta, velamentous cord insertion, and fetal vessels that may be near or over the cervical os.
-Histology: The histology associated with abnormalities of placental implantation shows basal chronic villitis, chronic lymphoplasmacytic inflammation in the basal plate, and villous agglutination. Retromembranous hemorrhage, subchorionic intervillous thrombi, and chorionic villi extending into myometrial vascular spaces may also be present.
How does Abnormalities of Placental Implantation Present?
Patients with abnormalities of placental implantation are pregnant females. The symptoms, features, and clinical findings associated with abnormalities of placental implantation include placental bulge with the distorted uterine outline, uterine serosal hypervascularity, and vaginal bleeding.
How is Abnormalities of Placental Implantation Diagnosed?
Abnormalities of placental implantation are diagnosed by doing an ultrasound during the second trimester.
How is Abnormalities of Placental Implantation Treated?
Abnormalities of placental implantation are treated using the medication, pelvic rest, and activity restrictions.
What is the Prognosis of Abnormalities of Placental Implantation?
The prognosis of abnormalities of placental implantation is poor with increased mortality rate.
What is Preeclampsia?
Preeclampsia is a condition with high blood pressure in pregnant women.
What is the Pathology of Preeclampsia?
The pathology of preeclampsia is:
-Etiology: The cause of preeclampsia is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to preeclampsia include defective spiral artery remodeling.
-Histology: The histology associated with preeclampsia shows placenta with villous ischemia.
How does Preeclampsia Present?
Patients with preeclampsia are pregnant females. The symptoms, features, and clinical findings associated with preeclampsia include protein in the urine, swelling in the legs, feet, and hands, weight gain, shoulder pain, belly pain, difficulty breathing, and vision changes.
How is Preeclampsia Diagnosed?
Preeclampsia is diagnosed by high blood pressure and also proteinuria, low platelet count, and pulmonary edema.
How is Preeclampsia Treated?
Preeclampsia is treated by establishing a patent airway and ensuring maternal oxygenation, prophylaxis, and blood pressure management.
What is the Prognosis of Preeclampsia?
The prognosis of preeclampsia is good if properly treated.
What is Eclampsia?
Eclampsia is most commonly defined as the new onset of convulsions and/or coma during pregnancy or in the immediate postpartum period in the presence of preeclampsia.
What is the Pathology of Eclampsia?
The pathology of eclampsia is:
-Etiology: The cause of eclampsia is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to eclampsia includes acute hypertension leads to cytotoxic edema formation, regional hypo-perfusion, and ischemic damage causing cerebral arteries uncontrollably spasm.
-Histology: The histology associated with eclampsia show placenta with villous ischemia.
How does Eclampsia Present?
Patients with eclampsia typically affect females present at the age range of less than 20. The symptoms, features, and clinical findings associated with eclampsia include convulsions, seizures, changes in mental status, frontal and/or occipital headaches, nausea, and/or visual changes.
How is Eclampsia Diagnosed?
Eclampsia is diagnosed by physical exam assessing blood pressure, and laboratory tests.
How is Eclampsia Treated?
Eclampsia is treated by ensuring adequate oxygenation and blood pressure control.
What is the Prognosis of Eclampsia?
The prognosis of eclampsia is good if treated appropriately.
What is Placental Infections?
Placental infections are the infections of the placenta. Infections may reach the placenta by ascending through the birth canal, or spreading through the blood system.
What is the Pathology of Placental Infections?
The pathology of placental infections is:
-Etiology: The cause of placental infections is a placental infection. These may be bacterial or viral.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to placental infections is pathogens accessing the intra-amniotic compartment.
-Morphology: The morphology associated with placental infections shows blastocystic differentiation and syncytiotrophoblast formation.
-Histology: The histology associated with placental infections shows placental villitis.
How does Placental Infections Present?
Patients with placental infections typically affect females present at the age range of 20-45 years. The symptoms, features, and clinical findings associated with placental infections include TORCH infections:
- (T) Toxoplasma
- (O) Other microbes
- (R) Rubella virus
- (C) Cytomegalovirus
- (H) Herpesvirus
TORCH infections may happen early in gestation. TORCH infections may cause chronic issues in the child, which include growth restriction, mental retardation, cardiac issues, and cataracts.
How are Placental Infections Diagnosed?
Placental infections is diagnosed by doing pelvic ultrasound and blood tests.
How are Placental Infections Treated?
Placental infections are treated using antibiotics.
What is the Prognosis of Placental Infections?
The prognosis of placental infections is fair if treated properly.
What are Twin Placentas?
Twin placentas are the dizygotic twins form when two separate eggs combine with two individual sperm. Each embryo develops it’s own placenta.
What is the Pathology of Twin Placentas?
The pathology of twin placentas is:
-Etiology: The cause of twin placentas is placental vascular anastomoses.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to twin placentas shows vascular anastomoses between the twins with arteries superficial to veins.
-Morphology: The morphology associated with twin placentas shows dichorionic or monochorionic physiology.
-Histology: The histology associated with twin placentas shows a T zone in the region of the disc where the dividing membranes attach to the chorionic plate.
How does Twin Placentas Present?
Patients with twin placentas typically affect females present at childbearing age. The symptoms, features, and clinical findings associated with twin placentas include acardia.
How is Twin Placentas Diagnosed?
Twin placentas are diagnosed by doing an obstetric ultrasound at a gestational age of 10–14 weeks.
How is Twin Placentas Treated?
Twin placentas is treated with laser fetal surgery.
What is the Prognosis of Twin Placentas?
The prognosis of twin placentas is good.
What are Gestational Trophoblastic Diseases?
Gestational trophoblastic diseases are a group of rare diseases in which abnormal trophoblast cells grow inside the uterus after conception.
Examples of gestational trophoblastic disease include:
- Choriocarcinoma
- Placental site trophoblastic tumor
- Hydatiform Mole
What is Choriocarcinoma?
Choriocarcinoma is cancer that occurs in a woman’s uterus.
What is the Pathology of Choriocarcinoma?
The pathology of choriocarcinoma is:
-Etiology: The cause of choriocarcinoma is hydatidiform mole, spontaneous abortion, ectopic pregnancy, normal term pregnancy, and hyperemesis gravidarum.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to choriocarcinoma includes syncytiotrophoblasts and cytotrophoblasts without the formation of definite placental type villi.
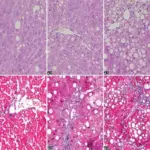
-Morphology: The morphology associated with choriocarcinoma shows syncytiotrophoblasts with eosinophilic cytoplasm. They often surround the cytotrophoblasts, reminiscent of their normal anatomical relationship in chorionic villi.
-Histology: The histology associated with choriocarcinoma shows solid sheets of atypical syncytiotrophoblast, cytotrophoblast, and intermediate trophoblast.
How does Choriocarcinoma Present?
Patients with choriocarcinoma typically affect females present at the age range of 20-49 years. The symptoms, features, and clinical findings associated with choriocarcinoma include increased quantitative chorionic gonadotropin, vaginal bleeding, shortness of breath, hemoptysis, chest pain. Chest X-ray shows multiple infiltrates of various shapes in both lungs.
How is Choriocarcinoma Diagnosed?
Choriocarcinoma is diagnosed through elevated HCG levels and imaging.
How is Choriocarcinoma Treated?
Choriocarcinoma is treated by chemotherapy, single-agent methotrexate, or actinomycin-D.
What is the Prognosis of Choriocarcinoma?
The prognosis of choriocarcinoma is poor as choriocarcinoma may come back within a few months to 3 years after treatment.
What is Placental Site Trophoblastic Tumor?
Placental site trophoblastic tumor is a form of the gestational trophoblastic disease, which is thought to arise from the intermediate trophoblast.
What is the Pathology of Placental Site Trophoblastic Tumor?
The pathology of placental site trophoblastic tumor is:
-Etiology: The cause of placental site trophoblastic tumor is choriocarcinoma.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to placental site trophoblastic tumor shows a tumor neoplastic transformation of intermediate trophoblastic cells that normally play a critical role in implantation.
-Morphology: The morphology associated with placental site trophoblastic tumor shows trophoblast cells.
-Histology: The histology associated with placental site trophoblastic tumor shows proliferating intermediate trophoblast with scarce cytotrophoblasts and syncytiotrophoblastic elements.
How does Placental Site Trophoblastic Tumor Present?
Patients with placental site trophoblastic tumor typically affect females present at the age range of childbearing. The symptoms, features, and clinical findings associated with placental site trophoblastic tumor include vaginal bleeding and amenorrhoea, low beta HCG levels.
How is Placental Site Trophoblastic Tumor Diagnosed?
Placental site trophoblastic tumor is diagnosed using blood tests and ultrasound.
How is Placental Site Trophoblastic Tumor Treated?
Placental site trophoblastic tumor is treated with hysterectomy.
What is the Prognosis of Placental Site Trophoblastic Tumor?
The prognosis of placental site trophoblastic tumor is poor.
What is Hydatiform Mole?
Hydatiform mole is a rare complication of pregnancy characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta. Trophoblastic tumor is also known as molar pregnancy.
Examples of hydatiform mole include:
- Complete mole
- Partial mole
- Invasive mole
What is a Complete Mole?
A complete mole is the most common type and does not contain metal parts.
What is the Pathology of Complete Mole?
The pathology of the complete mole is:
-Etiology: The cause of a complete mole is a single sperm (90% of the time) or two (10% of the time) sperm combining with an egg that has lost its DNA.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to complete mole shows diploid (45, XX, rarely 46, XY), absent fetus/embryo, diffuse swelling of villi, and diffuse trophoblastic hyperplasia.
-Morphology: The morphology associated with complete mole shows all the chorionic villi are vesicular, and no sign of embryonic or fetal development is present.
-Histology: The histology associated with complete mole shows diffuse, villous enlargement with marked hydropic changes.
How does Complete Mole Present?
Patients with complete mole typically affect females present at the age range of 18-55 years. The symptoms, features, and clinical findings associated with complete mole include painless vaginal bleeding, the uterus may be larger than expected, or the ovaries may be enlarged, hyperemesis, increased blood pressure, high HCG levels.
How is Complete Mole Diagnosed?
Complete mole is diagnosed using ultrasound and histopathological examination.
How is Complete Mole Treated?
Complete mole is treated by uterine suction or by surgical curettage, and methotrexate.
What is the Prognosis of Complete Mole?
The prognosis of the complete mole is good if treated in a timely manner.
What is a Partial Mole?
A partial mole is a mole where there might be identifiable fetal residues.
What is the Pathology of Partial Mole?
The pathology of the partial mole is:
-Etiology: The cause of partial mole is excess of paternal chromosomes promotes the growth of the placental tissue.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to partial mole shows triploid, (69 XXY, 69, XXY, 69, XXX), abnormal fetus/embryo, focal swelling of villi, focal trophoblastic hyperplasia.
-Morphology: The morphology associated with partial mole shows villi are vesicular, whereas others appear more normal, and embryonic/fetal development may be seen but the fetus is always malformed and is never viable.
-Histology: The histology associated with partial mole shows heterogeneity in villous size with 2 discrete populations; large, hydropic villi, and small, fibrotic villi.
How does Partial Mole Present?
Patients with partial mole typically affect female present at the age range of 20-55 years. The symptoms, features, and clinical findings associated with partial mole include painless vaginal bleeding, the uterus may be larger than expected, or the ovaries may be enlarged, hyperemesis, increased blood pressure, high HCG levels.
How is Partial Mole Diagnosed?
Partial mole is diagnosed using blood tests and histopathological examination.
How is Partial Mole Treated?
Partial mole is treated uterine suction or by surgical curettage, and methotrexate.
What is the Prognosis of Partial Mole?
The prognosis of the partial mole is good if treated in a timely manner.
What is an Invasive Mole?
An Invasive Mole is a subtype of gestational trophoblastic neoplasms (GTNs) that usually develops from the malignant transformation of trophoblastic tissue after molar evacuation.
What is the Pathology of Invasive Mole?
The pathology of the invasive mole is:
-Etiology: The cause of invasive mole is the evacuation of a molar pregnancy.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to invasive mole shows molar gestation invading myometrium or uterine vessels.
-Morphology: The morphology associated with invasive mole shows edematous trophoblastic tissue and hydropic chorionic villi invading the myometrium with or without vascular and extrauterine invasion.
-Histology: The histology associated with invasive mole shows abnormal (dysmorphic) chorionic villi and extravillous trophoblast invades myometrium and blood vessels.
How does Invasive Mole Present?
Patients with invasive mole typically affect women present at the age range of childbearing/reproductive. The symptoms, features, and clinical findings associated with invasive mole include vaginal bleeding and persistent elevation of hCG.
How is Invasive Mole Diagnosed?
Invasive mole is diagnosed using blood tests and radiologic examination.
How is Invasive Mole Treated?
Invasive mole is treated with chemotherapy.
What is the Prognosis of Invasive Mole?
The prognosis of an invasive mole is good with an 80 percent cure rate.