Physical injury is the study of the causes and effects of physical disease or injury, aka physical injury, which is damage to the body caused by an external force.
Physical injury includes:
- Mechanical trauma
- Thermal injury
- Electrical injury
- Ionizing radiation injury
- Death
What is Mechanical Trauma?
Mechanical trauma is an injury to any portion of the body from a blow, crush, cut, or penetrating wound.
Examples of mechanical trauma include scratches, grazes, avulsions, tears, chop wounds, etc.
What are the Patterns of Injury?
The patterns of injury are ones that have a distinct pattern that may reproduce the characteristics of the object causing the injury.
Patterns of injury include:
- Abrasions
- Contusions
- Lacerations
- Incisions
- Punctures
What are Abrasions?
Abrasions are the destruction of the skin, which usually involves the superficial layers of the epidermis only.
What are Contusions?
Contusions are the medical term for a bruise and they’re the result of a direct blow or an impact, such as a fall.
What are Lacerations?
Lacerations refer to skin wounds and unlike an abrasion, none of the skin is missing. They may be caused by injury with a sharp object or by impact injury from a blunt object or force.
What are Incisions?
Incisions are produced by a sharp edge and are usually longer than they are deep.
What are Punctures?
Punctures are caused by wood splinters, pins, nails, and glass or scissors and knives and almost any sharp object can potentially cause a puncture wound.
| Abrasions | Contusions | Lacerations | Incisions | Punctures | |
| CAUSE | a lateral rubbing action by a blow, a fall on a rough surface, being dragged in a vehicular accident, fingernails, thorns, or teeth bite | impact with a hard blunt weapon | breach of continuity of tissue involving depth more than the covering epithelium of skin or that of an organ, impact by hard blunt | drawing or saw like the movement of the weapon on the body surface when the weapon is rather light, striking the sharp edge on the body when the weapon is heavy or moderately heavy | the pointed end of a weapon or an object, entering the body |
| CAUSATIVE AGENT | stone, stick, needle, or any other weapon or rough surface of any other material | stone, stick, etc. | rough weapons or objects | a knife or razor, ax, sword | tip of a knife, arrow, needle, blunt end of an iron rod, spear, needles |
| FEATURES | superficial injuries, the lymph or blood which oozes out, and the denuded epithelial debris, dry up within a few hours to form a scab | reddish in color, slightly raised above the surrounding area, painful and tender | shape – usually irregular, margin – irregular, floor – tags of tissue may be seen passing across the floor | shape is elliptical or spindle-shaped, length is greater than breadth and depth, the floor is sharply cut and divided | shape and margin depends mostly on the shape of the weapon, depth is the greatest dimension of a punctured wound |
| TYPES | scratches, grazes, pressure, impact abrasions | patterned bruise, crescent-shaped | split, stretch lacerations, avulsions, tears, cut lacerations | suicidal, homicidal, and accidental, chop wounds | perforated, penetrated wound |
What is Thermal Injury?
Thermal Injury is open flames, steam, contact with hot objects, or hot liquid caused by burning.
Examples of thermal injuries include:
- Thermal burns
- Hyperthermia
- Hypothermia
What are Thermal Burns?
Thermal burns are burns due to external heat sources which raise the temperature of the skin and tissues and cause tissue cell death or charring.
What are Degrees of Burns?
Depth of burn is classified as the first, second, third, or fourth degree. The most useful clinical method to assess burn depth is the extent and speed of capillary refill.
- First degree burns are injuries in which minor epithelial damage of the epidermis exists.
- Second degree burns are injuries in which some portion of the skin appendages remains viable, allowing epithelial repair of the burn wound without skin grafting.
- Third degree burns are full-thickness burns that destroy both epidermis and dermis in which the capillary network of the dermis is completely destroyed.
What are Burn Related Injuries?
Burn related injuries include:
- Inhalation of smoke includes symptoms, such as cough, shortness of breath, hoarseness, headache, and acute mental status changes. Signs that may be useful in determining the degree of injury include soot in airway passages or skin color changes.
- Respiratory damage due to burns includes possible airway obstruction, respiratory failure, and respiratory arrest.
- Shock due to burns is caused by the increase in capillary permeability, coupled with evaporative water loss. Severe burn injury causes coagulation necrosis of tissue that initiates a physiologic response in every organ system that’s directly proportional to the size of the burn.
- Sepsis due to burns remains the major cause of death, immune consequences of this injury have been identified, and are specific deficits in neutrophil chemotaxis, phagocytosis, and intracellular bacterial killing.
- Systemic Inflammatory Response Syndrome (SIRS) can result in multiple organ failures and death.
Speed of care for burns includes immersing the burn in cool tap water or applying cold, wet compresses. This should be done for about 10 minutes or until the pain subsides.
What is Hyperthermia?
Hyperthermia is an abnormally high body temperature caused by a failure of the heat-regulating mechanisms of the body to deal with the heat coming from the environment.
What is Hypothermia?
Hypothermia is a potentially dangerous drop in body temperature caused by prolonged exposure to cold temperatures.
What is Electrical Injury?
Electrical injury is a physiological reaction caused by electric current passing through the body.
What is Ionizing Radiation Injury?
Ionizing Radiation Injury is tissue destruction or changes caused by deeply penetrating electromagnetic waves of high frequency or subatomic particles that form positively and negatively charged particles.
What is Death?
Death is the ultimate physical injury.
What is an Autopsy?
An autopsy is an examination of a body after death to determine the cause of death or the character and extent of changes produced by disease.
What is Forensics?
Forensics is the application of science to criminal and civil laws, mostly during criminal investigation, as governed by the legal standards of admissible evidence and criminal procedure.
What is a Forensic Autopsy?
A forensic autopsy is a series of tests and examinations performed on the body to determine the presence of an injury and to identify any disease that may have caused or contributed to the death.
What is the Approach to Autopsy and Forensics?
The approach to autopsy and forensics involves the following providing information through a postmortem examination of the body. Forensic autopsies differ from medical autopsies in that they fall under the jurisdiction of a local governmental death investigation office (typically a coroner or a medical examiner).
Consent for the autopsy by the person with legal authority to provide consent and confirmation that the decedent is at the proper location isn’t used for the medical examination. Forensics need to assess the scene, and determine the circumstances.
There is a hierarchy that doctors must adhere to when allowing someone to order an autopsy.
The hierarchy of who can legally sign for an autopsy to be performed from highest to lowest priority include:
- The Power of Attorney (either named in an Advanced Care Directive or legally appointed by a judge)
- The surviving spouse or domestic partner
- Adult children
- Parents
- Siblings
- Grandparents
- Nephews or nieces
- Uncles or aunts
- Cousins
- Stepchildren
- Relatives or next of kin of the previously deceased spouse
- Any relative or friend who is assuming custody of the body or responsibility for the burial
How to Prepare for an Autopsy Procedure?
Preparation for the autopsy by:
- Ensuring case is not under medical examiner jurisdiction
- Medical history review
- Discuss autopsy with the medical team involved
- Ensure personal protective equipment is available
- Prepare for photography
- Confirm the identity of the decedent
- Autopsy report
What is Usually on the Differential Diagnosis for an Autopsy?
The differential doagnosis for an autopsy typically includes:
- Sepsis
- Septic shock
- Cardiovascular pathology
- Pulmonary pathology
- Other conditions that are obvious to the patient’s medical history
What is Sepsis?
Sepsis is a potentially life-threatening condition that occurs when the body’s response to an infection damages its own tissues which cause organs to function poorly and abnormally.
What is the Pathology of Sepsis?
The pathology of sepsis is:
-Etiology: The cause of sepsis is inflammation, edema, erythema, discharge of pus, with positive Gram stain and culture results from incision and drainage or deep cultures.
-Pathogenesis: The sequence of events that lead to sepsis is from the effects of circulating bacterial products, mediated by cytokine release and caused by sustained bacteremia. The clinically observable effects of bacteremia in the host are occurring because of cytokines.
-Morphology: The morphology associated with sepsis shows that Gram-positive bacteria are the most common etiologic pathogens, although the incidence of gram-negative sepsis remains substantial, the incidence of fungal sepsis has been rising with more patients on immunosuppressive therapies and more cases of HIV infection.
How does Sepsis Present?
Patients with sepsis typically are males present at the age range of older than 65-years-old. The symptoms, features, and clinical findings associated with sepsis include fever or chills, confusion or disorientation, difficulty breathing, fast heart rate, or low blood pressure (hypotension), extreme pain, and sweaty skin. The signs of sepsis include a change in mental status, systolic blood pressure less than or equal to 100 mm Hg, and respiratory rate higher than or equal to 22 breaths per minute.
How is Sepsis Diagnosed?
Sepsis is diagnosed with multiple clinical, laboratory, radiologic, and microbiologic data. The diagnosis of sepsis may include blood culture and urine analysis and culture; chemistry studies that can suggest organ dysfunction, such as liver or kidney function tests; chest radiology; diagnostic imaging of the chest and abdomen or pelvis; cardiac studies such as ECG and troponins, as indicated; interventions such as paracentesis, thoracentesis, lumbar puncture, or aspiration of an abscess, as clinically indicated, and; measurement of biomarkers of sepsis such as procalcitonin levels.
How is Sepsis Treated?
Sepsis is treated with intravenous (IV) antibiotics to fight the infection, medications to increase blood pressure, insulin to stabilize blood sugar, corticosteroids to reduce inflammation, and pain relievers to help with discomfort.
What is the Prognosis of Sepsis?
The prognosis of sepsis is fair. It depends on underlying health status and host defenses, prompt and adequate surgical drainage of abscesses, relief of any obstruction of the intestinal or urinary tract, and appropriate and early empiric antimicrobial therapy. If it’s treated in a timely manner and with appropriate therapy, the prognosis is usually good, except in those with intra-abdominal or pelvic abscesses due to organ perforation.
What is Septic Shock?
Septic shock is a severe drop in blood pressure that results in highly abnormal problems with how cells work and produce energy.
What is the Pathology of Septic Shock?
The pathology of septic shock is:
-Etiology: The cause of septic shock is any type of bacteria and fungi, such as candida and viruses, although this is rare.
-Pathogenesis: The sequence of events that lead to septic shock is the activation of host defense mechanisms that result in the influx of activated neutrophils and monocytes, the release of inflammatory mediators, local vasodilation, increased endothelial permeability, and activation of coagulation pathways.
-Morphology: The morphology associated with septic shock shows three families of pattern recognition receptors that are involved in the initiation of the sepsis response.
How does Septic Shock Present?
Patients with septic shock typically are males present at age range of older than 50 years. The symptoms, features, and clinical findings associated with septic shock include the need for medication to maintain systolic blood pressure greater than or equal to 65 mm Hg and high levels of lactic acid in your blood (serum lactate) which means that cells aren’t using oxygen properly. Common symptoms include high fever or chills, intense body pain, fast heart rate, rapid breathing, and rash.
How is Septic Shock Diagnosed?
Septic shock is diagnosed with tests to determine how far along the infection is, what bacteria actually caused the infection that led to sepsis, as well as whether any additional bacterial infections are present, and whether there’s organ damage. In cases where the source of the infection isn’t clear from these tests above other methods include X-rays, CT scan, and MRI.
How is Septic Shock Treated?
Septic shock is treated with intravenous antibiotics to fight infection, vasopressor medications, insulin for blood sugar stability if needed, and corticosteroids. To treat dehydration and help increase blood pressure and blood flow to the organs are used large amounts of intravenous (IV) fluids, and for breathing is used a respirator. To remove a source of infection, such as draining a pus-filled abscess or removing infected tissue, is performed by surgery.
What is the Prognosis of Septic Shock?
The prognosis of septic shock is fair. It’s a severe complication of sepsis and the chances of recovering will depend on the source of the infection, how many organs have been affected, and how soon patients receive treatment after they first begin experiencing symptoms of sepsis.
What is Cardiovascular Pathology?
Cardiovascular pathology is usually caused by a buildup of fatty plaques in your arteries (atherosclerosis).
Examples of cardiovascular pathology include:
- Myocardial infarction
- Pulseless electrical activity
What is Myocardial Infarction?
Myocardial infarction (MI) is the irreversible death (necrosis) of heart muscle secondary to ischemia.
What is the Pathology of Myocardial Infarction?
The pathology of myocardial infarction is:
-Etiology: The cause of myocardial infarction is a coronary artery disease (CAD).
-Pathogenesis: The sequence of events that lead to myocardial infarction is when one or more areas of the heart muscle don’t get enough oxygen or when a part of the heart muscle doesn’t get enough blood. This happens when blood flow to the heart muscle is blocked.
-Morphology: The morphology associated with myocardial infarction shows abnormal cardiac findings on echocardiogram and histology.
How does Myocardial Infarction Present?
Patients with myocardial infarction typically are males present at age range of older than 35 years. The symptoms, features, and clinical findings associated with myocardial infarction include fatigue, chest discomfort, and malaise.
How is Myocardial Infarction Diagnosed?
Myocardial infarction is diagnosed with laboratory tests that include cardiac biomarkers or enzymes, troponin levels, complete blood cell count, comprehensive metabolic panel, and lipid profile. In the initial evaluation and triage of patients in whom a MI is suspected electrocardiography is used. To definitively diagnose or rule out coronary artery disease coronary angiography is used.
How is Myocardial Infarction Treated?
Myocardial infarction is treated with prehospital care, and emergency department, and inpatient care. The prehospital care includes intravenous access, supplemental oxygen if SaO2 is less than 90 %, pulse oximetry, immediate chewable aspirin and nitroglycerin for active chest pain, and telemetry and prehospital ECG. Sublingual nitroglycerin should be included for the initial stabilization of patients with suspected myocardial infarction. The initiation of beta-blockers is recommended for all patients with ST elevated myocardial infarction (unless beta-blockers are contraindicated). Fibrinolysis should also be considered if the patient is longer than 120 minutes from a percutaneous intervention (PCI) capable facility.
What is the Prognosis of Myocardial Infarction?
The prognosis of myocardial infarction is fair, but is highly variable depending on degree of pathology and care provided.
What is Pulseless Electrical Activity?
Pulseless electrical activity is characterized by unresponsiveness and the lack of a palpable pulse in the presence of organized cardiac electrical activity.
What is the Pathology of Pulseless Electrical Activity?
The pathology of pulseless electrical activity is:
-Etiology: The cause of pulseless electrical activity is a profound cardiovascular insult, such as severe prolonged hypoxia or acidosis or extreme hypovolemia or flow-restricting pulmonary embolus.
-Pathogenesis: The sequence of events that lead to pulseless electrical activity is the initial insult that weakens cardiac contraction, is exacerbated by worsening acidosis, hypoxia, and increasing vagal tone, and leads to inadequate mechanical activity, despite the presence of electrical activity. A vicious cycle is created, causing a major cardiovascular, respiratory, or metabolic derangement that results in the inability of cardiac muscle to generate sufficient force in response to electrical depolarization.
-Morphology: The morphology associated with pulseless electrical activity shows cardiac sarcomeres which length is unattainable causing decreased venous return to the left atrium and the left ventricle is unable to generate sufficient pressure to overcome its afterload.
How does Pulseless Electrical Activity Present?
Patients with pulseless electrical activity are typically elderly females. The symptoms, features, and clinical findings associated with pulseless electrical activity include tension pneumothorax and auto ̶ positive end-expiratory pressure (PEEP), myocardial dysfunction, hyperkalemia, hypothermia.
How is Pulseless Electrical Activity Diagnosed?
Pulseless electrical activity is diagnosed with measuring a core temperature, QRS duration, tests of values for arterial blood gases (ABGs), and serum electrolyte levels that may provide information regarding serum pH, oxygenation, serum potassium concentration, and glucose evaluation.
How is Pulseless Electrical Activity Treated?
Pulseless electrical activity is treated with needle decompression of pneumothorax, pericardiocentesis for tamponade, volume infusion, correction of body temperature, administration of thrombolytics, or surgical embolectomy.
What is the Prognosis of Pulseless Electrical Activity?
The prognosis of pulseless electrical activity is poor unless a rapidly reversible cause is identified and corrected. The electrocardiographic (ECG) characteristics are related to the patient’s prognosis and the more abnormal the ECG characteristics, the less likely the patient is to recover from PEA.
What is Pulmonary Pathology?
Pulmonary pathology is respiratory diseases that include asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, pneumonia, and lung cancer.
Examples of pulmonary pathology include:
- Pulmonary embolism
What is a Pulmonary Embolism?
A pulmonary embolism is a blockage in one of the pulmonary arteries in the lungs.
What is the Pathology of Pulmonary Embolism?
The pathology of pulmonary embolism is:
-Etiology: The cause of pulmonary embolism is a clump of material that gets wedged into an artery in the lungs, such as blood clots, fat from the marrow of a broken long bone, part of a tumor, and air bubbles. Pulmonary embolisms can be caused by blood clots that travel to the lungs from deep veins in the legs. Deep vein thrombosis is a rare condition in which blood clots travel from veins in other parts of the body.
-Pathogenesis: The sequence of events that lead to pulmonary embolism is the portions of the lung with blocked arteries that are robbed of blood and may die.
-Morphology: The morphology associated with pulmonary embolism shows multiple clots in many cases, obstructions in the arteries inside your lungs, and pulmonary infarction.
How does Pulmonary Embolism Present?
Patients with pulmonary embolism typically are either males or females present at the age range of older years. The symptoms, features, and clinical findings associated with pulmonary embolism include shortness of breath, chest pain that’s felt when breathing in deeply, coughing, bending or stooping, and cough. Other signs and symptoms that can occur include rapid or irregular heartbeat, lightheadedness or dizziness, fever, excessive sweating, and clammy or discolored skin (cyanosis). Leg pain and swelling are caused by a deep vein thrombosis and usually occur in the calf. Pulmonary embolism can also lead to pulmonary hypertension.
How is Pulmonary Embolism Diagnosed?
Pulmonary embolism is diagnosed with a medical history, a physical exam, and tests that include blood tests, chest x-ray, CT pulmonary angiography, ultrasound, MRI, ventilation-perfusion scan (V/Q scan), and pulmonary angiogram.
How is Pulmonary Embolism Treated?
Pulmonary embolism is treated with medications, such as blood thinners (anticoagulants) and clot dissolvers (thrombolytics). Surgical procedures include clot removal and vein filter. It’s important to continue treatment because of the risk of another deep vein thrombosis or pulmonary embolism.
What is the Prognosis of Pulmonary Embolism?
The prognosis of pulmonary embolism is fair. It can be life-threatening, but prompt treatment greatly reduces the risk of death. Protection against pulmonary embolism includes taking measures to prevent blood clots in the legs.
What are other Conditions that Should be Assessed at an Autopsy?
Other conditions include:
- Patient-related medical issues
- Anomalies
What Should be on the Differential for Pediatric-Related Autopsies?
The differential for pediatric-related autopsies should include:
- Shaken baby syndrome
- Sudden infant death syndrome (SIDS)
- Pediatric cardiovascular anomalies
What is Shaken Baby Syndrome?
The shaken baby syndrome is a serious brain injury resulting from forcefully shaking an infant or toddler.
What is the Pathology of Shaken Baby Syndrome?
The pathology of the shaken baby syndrome is:
-Etiology: The cause of the shaken baby syndrome is when someone shakes a baby or toddler due to frustration or anger, often because the child won’t stop crying.
-Pathogenesis: The sequence of events that lead to the shaken baby syndrome is a baby that’s forcefully shaken, his/her fragile brain moves back and forth inside the skull and this causes bruising, swelling, and bleeding.
-Morphology: The morphology associated with the shaken baby syndrome shows that survivors may develop certain medical conditions, such as partial or total blindness, developmental delays, learning problems, or behavior issues, intellectual disability, seizure disorders, and cerebral palsy.
How does Shaken Baby Syndrome Present?
Patients with the shaken baby syndrome typically are either males or females present at the age range of infants. The symptoms, features, and clinical findings associated with the shaken baby syndrome include breathing problems, extreme fussiness or irritability, poor eating, difficulty staying awake, vomiting, pale or bluish skin, seizures, coma, and paralysis.
How is Shaken Baby Syndrome Diagnosed?
The shaken baby syndrome is diagnosed with various tests that include skeletal survey, eye exam, blood tests, magnetic resonance imaging (MRI), and computerized tomography (CT) scan.
How is Shaken Baby Syndrome Treated?
The shaken baby syndrome is treated with emergency treatment that includes breathing support and surgery to stop bleeding in the brain.
What is the Prognosis of Shaken Baby Syndrome?
The prognosis of shaken baby syndrome is good. It’s preventable and help is available for parents who are at risk of harming a child. Also, parents can educate other caregivers about the dangers of the shaken baby syndrome.
What is Sudden Infant Death Syndrome (SIDS)?
Sudden infant death syndrome (SIDS) is the unexplained death, usually during sleep, of a seemingly healthy baby less than a year old.
What is the Pathology of Sudden Infant Death Syndrome (SIDS)?
The pathology of sudden infant death syndrome (SIDS) is:
-Etiology: The cause of sudden infant death syndrome (SIDS) is a gene or a change to the genes that cause certain health problems, or problems in the part of the brain that controls breathing, heart rate, blood pressure, temperature, and waking from sleep.
-Genes involved: 22q11 deletion syndrome, trisomy 21, 18, and 13.
-Pathogenesis: The sequence of events that lead to sudden infant death syndrome (SIDS) is the infant has an underlying (e.g., brainstem) abnormality that makes him unable to respond to low oxygen or high carbon dioxide blood levels, the infant is exposed to a triggering event such as sleeping face down on its tummy, and these events occur during a vulnerable stage in the infant’s development, i.e., the first six months of life.
How does Sudden Infant Death Syndrome (SIDS) Present?
Patients with sudden infant death syndrome (SIDS) typically are either males or females present at the age range of less than 1 year. The symptoms, features, and clinical findings associated with sudden infant death syndrome (SIDS) include its association with problems in the ability of the baby to arouse from sleep, to detect low levels of oxygen, or a buildup of carbon dioxide in the blood. Babies may re-breathe exhaled carbon dioxide when they sleep face down. In SIDS babies, rising carbon dioxide levels don’t activate nerve cells in the brainstem which stimulate the brain’s respiratory and arousal centers.
How is Sudden Infant Death Syndrome (SIDS) Diagnosed?
Sudden infant death syndrome (SIDS) is diagnosed only when all other causes of death have been excluded following a death scene investigation, an autopsy, and a review of the clinical history.
How is Sudden Infant Death Syndrome (SIDS) Treated?
Sudden infant death syndrome (SIDS) is treated with reducing the baby’s risk of SIDS by putting a baby to sleep on his back, using a firm sleep surface, and keeping fluffy blankets and stuffed animals out of his/her crib, not overheating a baby or his room when he/she sleeps, not smoking when pregnant and not allowing anyone to smoke around a baby, and breastfeeding.
What is the Prognosis of Sudden Infant Death Syndrome (SIDS)?
The prognosis of sudden infant death syndrome (SIDS) is poor.
What are Pediatric Cardiovascular Anomalies?
Pediatric cardiovascular anomalies are congenital heart defects that mean that a child was born with a problem in the structure of his or her heart.
What is the Pathology of Pediatric Cardiovascular Anomalies?
The pathology of pediatric cardiovascular anomalies is:
-Etiology: The cause of pediatric cardiovascular anomalies is genetics, certain medical conditions, some medications, and environmental or lifestyle factors, such as smoking.
-Genes involved: TBX2, TBX20, TBX3, TBX5, etc.
-Pathogenesis: The sequence of events that lead to pediatric cardiovascular anomalies is abnormal connections that allow blood to flow where it normally wouldn’t, for example, holes in the walls between heart chambers. Heart valve problems include stenosis- valves that are narrowed and don’t open completely or regurgitation- valves that don’t close completely.
-Morphology: The morphology associated with pediatric cardiovascular anomalies shows a combination of 4 defects: a hole in the wall between the heart’s ventricles, a narrowed passage between the right ventricle and pulmonary artery, a shift in the connection of the aorta to the heart, and thickened muscle in the right ventricle.
How do Pediatric Cardiovascular Anomalies Present?
Patients with pediatric cardiovascular anomalies typically are either males or females present at the age range of infants. The symptoms, features, and clinical findings associated with pediatric cardiovascular anomalies include pale gray or blue skin color (cyanosis), rapid breathing, swelling in the legs, belly, or areas around the eyes, and shortness of breath during feedings, leading to poor weight gain. In older children, symptoms may include easily becoming short of breath during exercise or activity, easily tiring during exercise or activity, fainting during exercise or activity, and swelling in the hands, ankles, or feet.
How are Pediatric Cardiovascular Anomalies Diagnosed?
Pediatric cardiovascular anomalies are diagnosed with pulse oximetry, electrocardiogram, echocardiogram, chest X-ray, cardiac catheterization, and heart magnetic resonance imaging (MRI).
How are Pediatric Cardiovascular Anomalies Treated?
Pediatric cardiovascular anomalies are treated with medications that include blood pressure drugs (angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and beta-blockers), diuretics, and heart rhythm drugs (antiarrhythmics). Surgery and heart procedures include fetal cardiac intervention, cardiac catheterization, heart surgery, and heart transplant.
What is the Prognosis of Pediatric Cardiovascular Anomalies?
The prognosis of pediatric cardiovascular anomalies is good. Living with a congenital heart defect can make some children feel stressed or anxious and talking to a therapist or counselor may help them learn new ways to manage stress and anxiety.
What are Postmortem Changes?
Postmortem changes are signs or indications of death.
Postmortem changes include:
- Algormortis
- Livormortis
- Pallormortis
- Rigormortis
What is Algormortis?
Algor mortis is the normal cooling of a body after death as it equilibrates with the ambient temperature.
What is Livormortis?
Livor mortis is the process where blood pools into dependent tissues following cessation of the circulation.
What is Pallormortis?
Pallor mortis is a paleness that develops in a corpse approximately 15 minutes to 2 hours after death.
What is Rigormortis?
Rigor mortis is a postmortem change resulting in the stiffening of the body muscles due to chemical changes in their myofibrils.
The timing for rigor mortis includes four significant stages of rigor mortis: autolysis, bloat, active decay, and skeletonization.
| POSTMORTEM CHANGE | DEFINITION |
| Algor mortis | The process by which the body cools after death. |
| Livor mortis | The purple-red coloration that appears on dependent portions of the body other than areas exposed to pressure after the heart ceases to beat. |
| Pallor mortis | A paleness that develops in a corpse approximately 15 minutes to 2 hours after death. |
| Rigor mortis | The postmortem stiffening of the body’s muscles. |
What is the Mechanism of Death?
The mechanism of death is the specific physiological derangement that actually led to the cessation of life.
There are five categories for the mechanism of death which include:
- Accidental
- Homicidal
- Natural
- Suicidal
- Undetermined
What is an Accidental Mechanism of Death?
An accidental mechanism of death is an unnatural death that’s caused by an accident, such as a slip and fall, traffic collision, or accidental poisoning.
What is a Homicidal Mechanism of Death?
Homicidal mechanism of death is the action of one person directly causing the death of another, a death that occurs during and is related to the commission of a felony.
What is a Natural Mechanism of Death?
Natural mechanism of death includes respiratory and cardiovascular diseases.
What is a Suicidal Mechanism of Death?
Suicidal mechanism of death is caused by injuring oneself with the intent to die but doesn’t die as a result of his/her actions.
What is an Undetermined Mechanism of Death?
Undetermined mechanism of death is assigned to cases of unnatural death when a clear preponderance of evidence supporting a specific manner (homicide, accident, or suicide) is not available.
| MECHANISM OF DEATH | DEFINITION |
| Accidental | A death caused by an accident like a traffic collision, fall, and slip, or anything else without malicious intent. |
| Homicidal | A volitional act to kill another that might result from negligent, reckless, or accidental activities. |
| Natural | The end result of a disease or an internal malfunction due to old age. |
| Suicidal | The act of causing one’s own death on intention. |
| Undetermined | Unnatural death when a clear preponderance of evidence supporting a specific manner isn’t available. |
What is the Cause of Death?
The cause of death is the specific injury, issue, or disease that leads to death.
How are Injuries Classified?
Injuries are classified as:
- Asphyxia
- Blunt force injuries
- Drowning
- Electrical injuries
- Fire death injuries
- Gunshot wounds
- Sharp force injuries
- Temperature related deaths
- Motor vehicle deaths
- Substance Abuse
What are Asphyxia Injuries?
Asphyxia injuries are the result of a protracted crush injury to the upper torso or epigastrium in which venous hypertension is transmitted to the valveless veins of the upper body.
What are Blunt Force Injuries?
Blunt force injuries are traumas of the body by forceful impact, falls, or physical attack with a dull object.
What are Drowning Injuries?
Drowning injuries are among the top 10 causes of mortality for children and young people worldwide. It results in hypoxia, which can damage multiple organs, particularly the brain.
What are Electrical Injuries?
Electrical injuries are damages caused by generated electrical current passing through the body. Symptoms include skin burns, damage to internal organs and other soft tissues to cardiac arrhythmias, and respiratory arrest.
What are Fire Death Injuries?
Fire death injuries are usually caused by smoke inhalation of the toxic gases produced by fires. Only about 30 % of fire-related deaths and injuries are caused by flames and burns.
What are Gunshot Wound Injuries?
Gunshot wound injuries are caused by a projectile from a firearm and may include bleeding, broken bones, organ damage, infection of the wound, loss of the ability to move part of the body, and, in more severe cases, death.
What are Sharp Force Injuries?
Sharp force injuries are characterized by a relatively well-defined traumatic separation of tissues caused by pointed objects or objects with sharp edges.
What are Temperature Related Death Injuries?
Temperature-related death injuries are caused when people are exposed to the extreme heat that can lead to heat exhaustion, heatstroke, heart attacks, strokes, and other forms of cardiovascular disease.
What are Motor Vehicle Death Injuries?
Motor vehicle death injuries are traumatic brain injuries, internal bleeding, broken ribs, or spinal cord injuries that typically occur due to head-on collisions, driver- or passenger-side impacts, or rollovers caused by driver negligence or reckless behavior.
What are Substance Abuse Injuries?
Substance Abuse injuries are injuries that may happen either as a direct result of the toxic effects of drugs and alcohol or as a consequence related to drug use, which can include anything from seizures, asphyxiation, respiratory arrest, hypoxic brain injury, and more.
What is an Autopsy?
An autopsy is a medical examination of a deceased person that involves the following:
- External examination
- Internal examination
- Microscopic examination
- Clinicopathologic correlation
What is an External Examination for an Autopsy?
An External examination for an autopsy is a detailed description of the decedent’s remains including scars, surgical incisions, medical devices, tattoos, etc., but no internal cuts are made on the body and no organs are examined.
What is an Internal Examination for an Autopsy?
An Internal examination for an autopsy is when the pathologist removes and dissects the chest, abdominal and pelvic organs, and, if necessary, the brain. It’s unusual to examine the face, arms, hands, or legs internally.
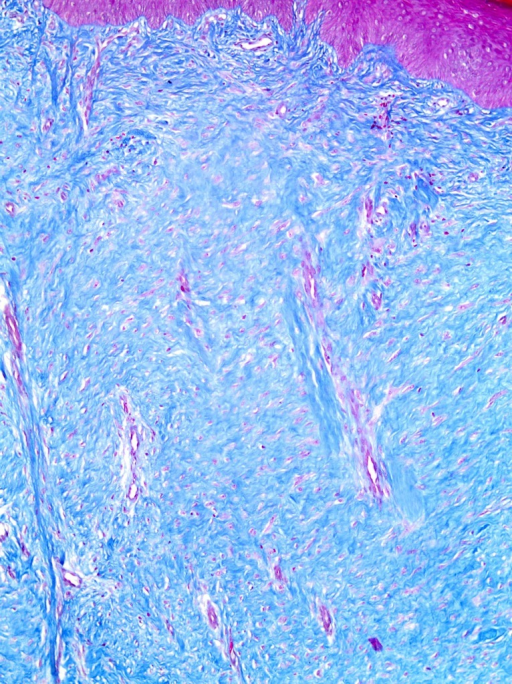
What is a Microscopic Examination for an Autopsy?
A Microscopic examination for an autopsy is performing the histologic examination in all cases regardless of cause and manner of death. It should be used, as needed, in certain circumstances but is not necessary as a matter of routine.
What is a Clinicopathologic Correlation for an Autopsy?
A Clinicopathologic correlation for an autopsy is an objective summary and correlation of clinical findings with gross and microscopic findings and with the results of other studies performed at autopsy, to describe the death and elucidate the sequence of events leading to death.
What are Other Studies that may be used in an Autopsy or Forensic Case?
Other studies that may be used in an autopsy or forensic case include:
- Clinical chemistry tests
- Special stains
- Crime scene investigation
What are Clinical Chemistry Tests?
Clinical chemistry tests are examinations that measure concentrations or activities of substances (ions, molecules, complexes) in body fluids.
What are Special Stains?
Special stains are processes that generally employ a dye or chemical that has an affinity for the particular tissue component that’s to be demonstrated and they allow the presence or absence of certain cell types, structures or microorganisms to be viewed microscopically.
What is a Crime Scene Investigation?
A crime scene investigation is the use of physical evidence at the scene of the crime and the use of deductive and inductive reasoning to gain knowledge of the events surrounding the crime.
What are the Timelines for Reporting Autopsy Results?
The timelines for reporting autopsy results are:
- 48 hours after the case is accessioned for the provisional autopsy diagnosis (PAD)
- 2 months after the case is accessioned for the final report